The fentanyl crisis demands robust responses, and outreach team programs are vital in providing education, harm reduction, and treatment access within communities. These programs face barriers like stigma, limited funding, and legal restrictions. Effective strategies include community partnerships, harm reduction initiatives, and comprehensive support services. Government involvement is crucial, as it offers funding, policy support, and coordination to enhance outreach efforts. Together, these resources enable outreach programs to combat the fentanyl crisis and save lives more effectively.
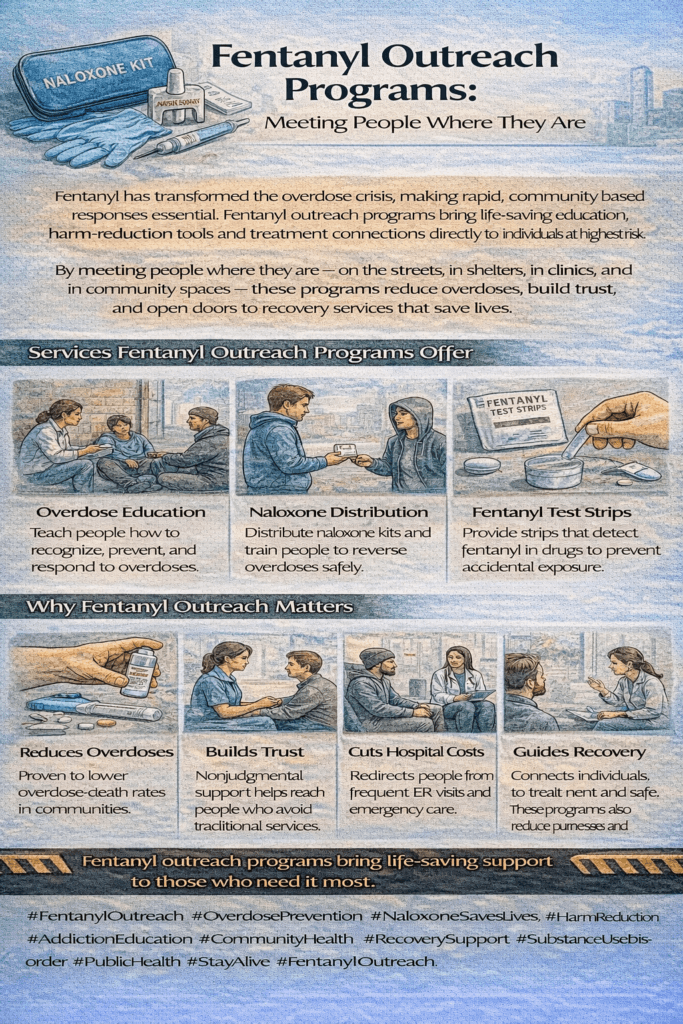
How Outreach Teams Can Help Combat the Fentanyl Addiction Crisis
The fentanyl addiction crisis has escalated into one of the most pressing public health challenges today. To address this crisis, outreach team programs that provide comprehensive education, harm reduction services, treatment access, and ongoing support can significantly impact the situation. By meeting individuals where they are and addressing the complexities of addiction, these programs can reduce overdose incidents, save lives, and guide individuals toward recovery. In addition to direct support, collaboration with community stakeholders and ongoing adaptation based on real-time data will allow these outreach efforts to become a cornerstone in combating fentanyl addiction.
1. Education and Awareness
Outreach programs can play a pivotal role in raising awareness about the risks associated with fentanyl use and overdose prevention.
- Community Education: Offering workshops and distributing informative materials on the dangers of fentanyl and treatment options can empower the public to make informed decisions.
- Targeted Campaigns: Focusing on high-risk groups like teenagers, young adults, and current opioid users through specialized campaigns can inform them about safe practices and available resources.
2. Early Intervention and Screening
By reaching out to vulnerable populations early, outreach teams can identify and address addiction before it spirals out of control.
- Street Outreach: Teams can connect with individuals in the most vulnerable environments, such as shelters and community centers, providing immediate assistance and access to resources.
- Screening for Use: Routine screenings for fentanyl and other opioids in community settings can help identify individuals at risk and direct them toward services for addiction management and treatment.
3. Harm Reduction Services
Harm reduction efforts are crucial in reducing the immediate dangers posed by fentanyl use.
- Naloxone Distribution: By distributing naloxone kits and providing training on overdose reversal, outreach teams can save lives by enabling bystanders to respond quickly to opioid overdoses.
- Safe Use Education: Educating users on safer practices—such as avoiding use alone, using fentanyl test strips, and recognizing overdose symptoms—can reduce the risk of fatal overdoses.
4. Access to Treatment
Providing immediate access to treatment is critical to addressing fentanyl addiction effectively.
- Mobile Health Services: Outreach programs can offer on-site medical care through mobile health units, including access to medication-assisted treatment (MAT) using buprenorphine or methadone.
- Referral Networks: Establishing robust referral systems ensures individuals are quickly connected to detox centers, rehabilitation programs, and mental health services.
5. Support and Counseling
Addressing the emotional and psychological aspects of addiction is vital for long-term recovery.
- Peer Support Programs: Peer outreach workers with lived addiction experiences can foster trust and offer relatable guidance and support.
- Counseling Services: Providing on-the-spot counseling and mental health services helps individuals manage the psychological challenges of addiction and any co-occurring mental health conditions.
6. Resource Navigation
Individuals facing addiction often struggle with navigating social systems, and outreach programs can help them connect with critical resources.
- Case Management: Dedicated case managers can help individuals access healthcare, social services, housing, and employment opportunities.
- Follow-Up Care: Ongoing check-ins and follow-up appointments can ensure individuals stay engaged with their recovery plan and receive continuous support.
7. Community Engagement and Partnerships
Building a strong community response to the fentanyl crisis requires collaboration between multiple stakeholders.
- Collaborate with Local Organizations: Partnerships with local health departments, law enforcement, schools, and community groups can help coordinate a response to addiction.
- Community Events: Organizing events to unite the community can help reduce the stigma surrounding addiction and highlight available resources.
8. Data Collection and Analysis
Data-driven approaches enable outreach programs to adapt to the changing landscape of fentanyl use.
- Track Outcomes: Collecting data on the success of various program elements enables outreach teams to continuously improve their approaches.
- Identify Trends: Monitoring trends in fentanyl use and overdose hotspots enables more targeted and effective outreach efforts.
9. Advocacy
Advocating for policies that prioritize harm reduction and treatment access is critical to achieving long-term success in the fight against fentanyl addiction.
- Policy Advocacy: Outreach programs can be crucial for advancing policy changes that increase funding for addiction services and expand access to treatment.
- Public Health Initiatives: Working alongside public health officials can help implement broader initiatives that address both supply- and demand-side aspects of the fentanyl crisis.
By integrating these strategies, outreach teams can not only provide immediate relief to those struggling with fentanyl addiction but also contribute to long-term solutions. The multifaceted approach of education, harm reduction, access to treatment, and ongoing support makes these programs vital in the fight against the opioid epidemic.
Breaking Down Barriers: Strengthening Outreach Team Programs to Combat the Fentanyl Addiction Crisis
The fentanyl addiction crisis continues to ravage communities across the nation, but effective outreach team programs hold the potential to make a significant difference. However, these programs face substantial barriers that limit their effectiveness. Overcoming these obstacles requires a concerted effort to reduce stigma, secure sufficient funding, advocate for supportive policies, improve accessibility and engagement, provide integrated care, ensure proper training, address cultural and language needs, and establish effective data collection systems.
By addressing these key barriers, outreach programs can improve their ability to combat fentanyl addiction, leading to better health outcomes and safer communities.
1. Stigma and Discrimination
Public Stigma: Widespread negative attitudes toward individuals with substance use disorders can prevent people from seeking help or engaging with outreach services.
Self-Stigma: Internalized shame or guilt can deter individuals from seeking support, further marginalizing those in need.
Reducing stigma through public awareness campaigns, promoting understanding of addiction as a medical condition, and encouraging empathy can create an environment where more people feel safe seeking help.
2. Funding and Resource Limitations
Insufficient Funding: Many outreach programs struggle with limited financial resources, which can limit their capacity to hire qualified staff, expand services, and provide crucial materials such as naloxone kits and fentanyl test strips.
Resource Allocation: With limited resources, outreach teams may face tough decisions regarding service prioritization, making it difficult to maintain or expand their efforts.
Advocating for increased funding, developing strategic partnerships, and optimizing resource allocation are essential to maintaining sustainable and impactful outreach programs.
3. Legal and Policy Barriers
Regulatory Restrictions: Legal limitations on distributing harm reduction tools like naloxone or fentanyl test strips can hinder outreach teams’ ability to save lives.
Criminalization of Substance Use: Policies that emphasize punitive measures over treatment discourage individuals from seeking help for fear of legal consequences.
Policy reform focused on harm reduction and decriminalization can empower outreach teams to better serve affected communities and ensure that individuals are not punished for seeking help.
4. Access and Accessibility
Geographic Barriers: People in rural or remote areas often have limited access to outreach services, exacerbated by limited transportation options.
Service Hours and Locations: Outreach programs may not be accessible during times or in locations convenient for the populations they aim to serve.
Expanding mobile outreach services and providing flexible hours can help bridge the accessibility gap, ensuring that help reaches those in need, wherever they are.
5. Trust and Engagement
Mistrust of Authorities: Many individuals struggling with substance use disorders distrust outreach workers, especially if they believe the workers are connected to law enforcement.
Engagement Challenges: Encouraging sustained engagement with outreach services can be difficult, especially among transient or hard-to-reach populations.
Building relationships through peer support workers and trauma-informed care can foster trust and provide consistent, non-judgmental support, encouraging long-term engagement.
6. Comprehensive Support Services
Lack of Holistic Care: Addiction rarely exists in isolation, and many outreach programs lack the resources to address associated issues like mental health, housing, and employment.
Integration with Healthcare Systems: The lack of coordination between outreach services and healthcare systems creates care gaps, making it harder for individuals to access comprehensive support.
Developing a holistic, integrated care model that includes mental health, housing assistance, and employment support ensures that individuals receive the multifaceted care they need to recover.
7. Training and Staffing
Limited Training: Outreach workers often lack sufficient training in dealing with the complexities of fentanyl addiction, overdose response, and trauma-informed care.
Staff Burnout: The emotional toll and high demand on outreach workers can lead to burnout, affecting program sustainability and service quality.
Providing ongoing training, mentorship, and mental health support for outreach workers can enhance their effectiveness and longevity, ensuring consistent care for those in need.
8. Cultural and Language Barriers
Cultural Sensitivity: Programs may struggle to connect with diverse communities without offering culturally appropriate care.
Language Barriers: A lack of multilingual staff and resources prevents non-English speaking individuals from accessing vital services.
Investing in culturally competent care and ensuring multilingual support can broaden the reach of outreach programs and make them more accessible to diverse populations.
9. Data and Evaluation
Insufficient Data: A lack of comprehensive data on program outcomes can hinder funding efforts and prevent necessary improvements.
Evaluation Challenges: Substance use disorders are complex, making it difficult to measure the long-term impact of outreach services.
By establishing robust data collection and evaluation mechanisms, outreach teams can track outcomes, demonstrate effectiveness, and continuously refine their approaches to best meet the needs of those they serve.
Overcoming these barriers is essential for improving the effectiveness of outreach team programs in addressing the fentanyl addiction crisis. When equipped with adequate resources, supportive policies, and culturally competent care, outreach teams can drive meaningful change, helping individuals find the path to recovery and creating safer, healthier communities.
Government Support: Enhancing Outreach Programs in the Fight Against the Fentanyl Crisis
The fentanyl addiction crisis has placed immense pressure on communities, but government actions have significantly bolstered outreach programs’ ability to respond effectively. Through funding, supportive policies, harm reduction initiatives, education, data monitoring, collaboration, and regulatory changes, governments are providing critical infrastructure to expand the reach and impact of these programs. These comprehensive measures are essential to overcoming the complex challenges posed by fentanyl addiction.
1. Funding and Grants
Governments at the federal, state, and local levels have allocated significant resources to support outreach teams in tackling the opioid epidemic.
- Federal Grants: Programs like the State Opioid Response (SOR) grants provide states with substantial funding to support outreach efforts, including prevention, treatment, and recovery services.
- Local and State Funding: State and local governments have dedicated funds to initiatives such as naloxone distribution and harm reduction programs, enabling outreach teams to operate more effectively.
- Public-Private Partnerships: In some cases, governments collaborate with private organizations to co-fund programs, ensuring a broader reach and sustainable impact.
2. Policy and Legislation
Government policy changes have created a more supportive environment for outreach teams to operate and engage with individuals at risk.
- Good Samaritan Laws: These laws protect individuals who call for medical help during an overdose from legal prosecution, encouraging timely intervention without fear of arrest.
- Expansion of MAT: Governments have expanded access to Medication-Assisted Treatment (MAT), allowing outreach programs to connect individuals with practical, evidence-based treatments for opioid addiction.
- Decriminalization Efforts: Some areas are shifting away from punitive drug policies toward a focus on treatment, making it easier for outreach teams to engage users without the fear of legal consequences.
3. Harm Reduction Initiatives
Harm reduction is a central component of outreach programs, and government support has been pivotal in making life-saving tools accessible.
- Naloxone Access: Governments have increased access to naloxone, a life-saving opioid overdose reversal drug, through distribution programs, over-the-counter availability, and widespread training initiatives.
- Fentanyl Test Strips: States have begun legalizing and promoting the use of fentanyl test strips, allowing individuals to test substances for the presence of fentanyl and take precautions.
- Safe Injection Sites: In certain areas, governments support supervised injection sites where individuals can use drugs under medical supervision, reducing overdose risks and linking users to services.
4. Education and Training
Education and training efforts by the government have equipped both professionals and the public with the knowledge needed to combat fentanyl addiction.
- Public Awareness Campaigns: Government-run campaigns educate the public about the dangers of fentanyl, the signs of overdose, and how to respond in an emergency.
- Training Programs: Training healthcare providers, first responders, and community workers on addiction, overdose response, and naloxone use ensures that help is always available when needed.
5. Data Collection and Monitoring
Real-time data is critical for outreach teams to respond effectively, and government-led data collection systems provide valuable insights.
- Overdose Surveillance: Governments have established overdose monitoring systems that provide real-time data on overdose hotspots, allowing outreach programs to target their efforts in high-risk areas.
- Research Funding: Governments fund research into addiction treatment and prevention strategies, helping improve the methods and tools available to outreach programs.
6. Collaboration and Coordination
Government-led collaboration across multiple sectors has helped create a comprehensive response to the opioid crisis.
- Interagency Task Forces: Governments often establish task forces to coordinate responses to the opioid epidemic, bringing together agencies from health, law enforcement, education, and other sectors.
- Public Health Partnerships: Outreach programs benefit from partnerships between public health departments and community organizations, ensuring their efforts align with broader public health goals.
7. Support for Innovation
Governments are also fostering innovation by supporting the development of new approaches to addiction treatment and overdose prevention.
- Pilot Programs: Government funding for pilot programs allows outreach teams to test innovative strategies, helping scale the most effective approaches to fighting fentanyl addiction.
- Telehealth Services: The expansion of telehealth services, especially during the COVID-19 pandemic, has made addiction treatment and support more accessible, complementing in-person outreach efforts.
8. Legal and Regulatory Support
Governments are helping outreach programs overcome legal and regulatory barriers that might otherwise limit their effectiveness.
- Regulatory Changes: Regulations now make it easier for outreach teams to distribute harm reduction supplies like naloxone and fentanyl test strips, ensuring these tools reach those most in need.
- Insurance Coverage: Efforts to expand insurance coverage for addiction treatment have improved access to affordable care, enabling outreach programs to link individuals to necessary services.
Through these critical actions, governments have enabled outreach teams to operate more effectively in their mission to combat the fentanyl addiction crisis. These programs can help build healthier communities and achieve more successful recovery outcomes by providing the funding, policies, and tools needed to support individuals at risk.
Strengthening Fentanyl Addiction Outreach: Key Community Resource Strategies for Lasting Impact
Tackling the fentanyl addiction crisis requires a multifaceted approach that mobilizes community resources and enhances outreach programs. By leveraging partnerships, harm-reduction strategies, education, mobile outreach, peer support, and more, outreach teams can create a sustainable, impactful response to the crisis. These strategies strengthen the support network for individuals in need, ultimately improving health outcomes and building more resilient communities.
1. Partnerships with Local Organizations
Collaborating with local organizations can dramatically expand the resources and services available to individuals battling fentanyl addiction.
- Healthcare Providers: Outreach teams should partner with hospitals, clinics, and mental health providers to ensure comprehensive care, including medication-assisted treatment (MAT), counseling, and rehabilitation services.
- Nonprofits and NGOs: Collaborations with nonprofits that specialize in substance use disorder (SUD) treatment, mental health, and social services can broaden the range of resources and create a holistic support system for individuals in recovery.
2. Harm Reduction Services
Harm reduction is essential to any outreach program, providing immediate, life-saving interventions for those at risk.
- Naloxone Distribution: Distribute naloxone kits widely through partnerships with pharmacies, health departments, and community organizations. Provide training to ensure individuals know how to administer naloxone during an overdose.
- Fentanyl Test Strips: Providing fentanyl test strips allows individuals to test substances for the presence of fentanyl, reducing the risk of overdose by encouraging safer usage practices.
3. Education and Awareness Campaigns
Raising awareness about fentanyl and its risks through education can help prevent addiction and inform communities about available support.
- Public Education: Conduct widespread education campaigns to raise awareness about fentanyl dangers, signs of overdose, and resources for help, engaging the entire community.
- School Programs: Implement targeted educational programs to teach students about the risks of drug use and how to seek help when needed.
4. Mobile Outreach Units
Mobile outreach units are crucial for reaching individuals who may not have access to healthcare or harm reduction services due to geographic or socio-economic barriers.
- Mobile Clinics: Deploy mobile health units to provide medical care, harm-reduction supplies, and counseling in high-risk areas, making it easier for individuals to access help where they are.
- Street Outreach Teams: Train outreach workers to engage with homeless populations and other hard-to-reach groups, offering immediate support and resources in their communities.
5. Peer Support and Mentorship
Peer support is a powerful tool in addiction recovery, providing individuals with relatable mentors who understand their struggles.
- Peer Support Programs: Employ individuals with lived experience of addiction to offer peer support, helping to build trust and connection with those currently struggling with fentanyl use.
- Mentorship Programs: Establish mentorship programs where individuals in recovery can guide and support those in the early stages, offering hope and practical advice for long-term recovery.
6. Access to Basic Needs and Social Services
Addressing basic needs like housing, employment, and education is critical to breaking the cycle of addiction and supporting sustained recovery.
- Housing Support: Partner with local housing organizations to secure stable housing for individuals in recovery, providing the stability needed for long-term success.
- Employment and Education: Collaborate with job-training and educational programs to provide opportunities for skill development and employment, thereby reducing socioeconomic factors that can contribute to substance use.
7. Family Support Services
Addiction doesn’t just affect individuals; it impacts families and entire communities. Providing support for families can foster a healthier environment for recovery.
- Family Counseling: Offer family counseling services to help families navigate the challenges of supporting a loved one through addiction and fostering communication and understanding.
- Education for Families: Provide educational resources for families about the nature of addiction, treatment options, and how to create a supportive environment for recovery.
8. Community-Based Support Groups
Creating spaces for individuals to share experiences and seek support within their communities can significantly impact recovery efforts.
- Support Groups: Facilitate community-based support groups for individuals struggling with addiction, offering a safe space to share experiences and coping strategies.
- Community Centers: Utilize community centers as hubs for support group meetings, educational workshops, and resource distribution, fostering a sense of connection and belonging.
9. Advocacy and Policy Change
Advocating for policy changes at every level is essential to creating a supportive legal and social framework for outreach programs.
- Advocacy Campaigns: Push for policies that support harm reduction strategies, expand funding for SUD services, and decriminalize substance use, enabling outreach programs to operate without legal hindrances.
- Public Health Initiatives: Work with public health officials to develop broader initiatives that reduce both the supply and demand for illicit fentanyl.
10. Training and Capacity Building
Equipping professionals and volunteers with the necessary skills and knowledge is vital for the effectiveness and sustainability of outreach programs.
- Training for First Responders: Provide specialized training for first responders—such as police, firefighters, and paramedics—on how to handle overdoses and compassionately interact with individuals with SUDs.
- Community Volunteer Training: Train community volunteers to support outreach efforts, increase program capacity and reach, and empower the community to take an active role in combating the crisis.
By leveraging these strategies, outreach programs can strengthen their impact and sustainability in the fight against the fentanyl addiction crisis. Through collaboration, education, peer support, and focusing on meeting immediate and long-term needs, outreach teams can create lasting change and build healthier, more resilient communities.
Frequently Asked Questions
Here are some common questions:
1. What is a fentanyl outreach program?
It is a community-based program that provides overdose prevention education, harm-reduction tools, and connections to treatment for people at high risk of fentanyl overdose.
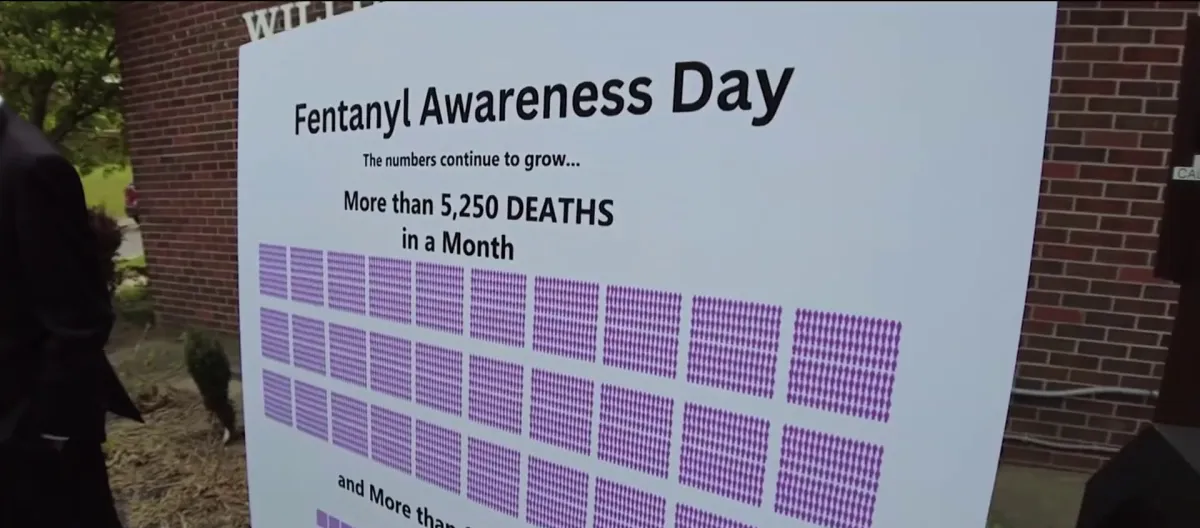
2. Why are fentanyl outreach programs needed?
Fentanyl is extremely potent and fast-acting. Many at-risk individuals do not access traditional healthcare, so outreach brings life-saving services directly to them.
3. What services do these programs provide?
Common services include naloxone distribution, overdose response training, fentanyl test strips, health screenings, wound care, and referrals to treatment and housing resources.
4. Do outreach programs encourage drug use?
No. They focus on keeping people alive and safe while building trust and guiding individuals toward treatment and recovery when they are ready.
5. How does naloxone help in outreach programs?
Naloxone can reverse opioid overdoses. Outreach teams distribute it and train people to recognize overdose signs and respond quickly.
6. What are fentanyl test strips?
They are simple tools that allow individuals to test drugs for hidden fentanyl before use, reducing accidental overdose risk.
7. Who works on outreach teams?
Teams often include peer recovery specialists, nurses, social workers, counselors, and community health workers.
8. Why is peer support important in outreach?
Peers with lived experience build trust, reduce stigma, and help individuals feel safe accepting support.
9. Can outreach programs connect people to addiction treatment?
Yes. They provide direct referrals to detox, medication-assisted treatment, counseling, and recovery services.
10. Do fentanyl outreach programs save lives?
Yes. Communities with strong outreach programs show reduced overdose deaths and improved connections to care.
Conclusion
Outreach team programs are essential in tackling the fentanyl crisis by providing critical services such as education, harm reduction, and treatment access. Despite barriers such as stigma, limited funding, and legal challenges, these programs can significantly enhance their impact through strategic community partnerships and comprehensive support services. Government involvement plays a crucial role by offering financial support, policy adjustments, and coordination efforts that strengthen these outreach initiatives. By addressing these challenges collaboratively, outreach programs can more effectively mitigate the devastating effects of the fentanyl crisis and save countless lives.
Video: Fentanyl Outreach Goes Where People Need It Most #OverdosePrevention #CommunityHealth #StayAlive