Medication for Opioid Use Disorder (MOUD) has become one of the most effective interventions for reducing opioid-related deaths and supporting long-term recovery. Medications such as methadone, buprenorphine, and naltrexone stabilize brain chemistry, reduce cravings, and protect against fatal overdose. Research consistently shows that individuals who remain on MOUD for extended periods experience significantly higher survival rates than those who discontinue treatment early. However, medication alone is not enough. Successful long-term outcomes depend on active self-management, supportive family involvement, and strong community resources that together reinforce treatment engagement and recovery stability.
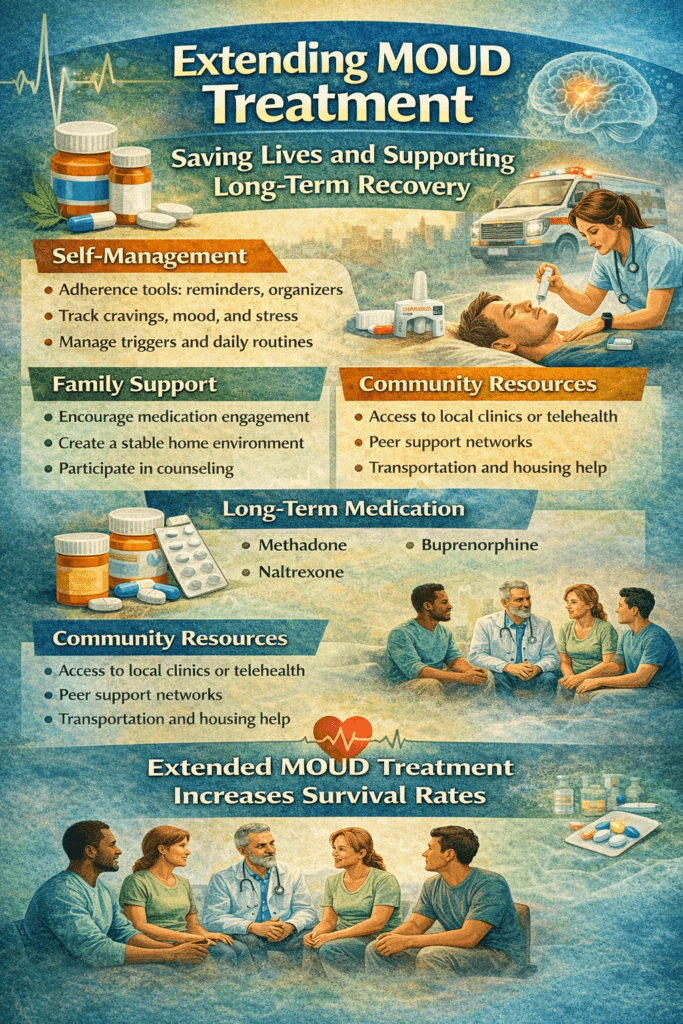
Extending MOUD Treatment: How Longer Medication Use Increases Survival Rates
Medication for Opioid Use Disorder (MOUD) has transformed addiction treatment by reducing cravings, preventing withdrawal, and lowering overdose risk. Medications such as methadone, buprenorphine, and naltrexone stabilize brain chemistry and allow individuals to rebuild daily functioning. However, a growing body of research indicates that the duration of MOUD use is among the strongest predictors of survival. Extending MOUD treatment duration significantly increases recovery stability and reduces fatal outcomes.
Opioid addiction is a chronic brain disorder, not a short-term condition. When MOUD is discontinued prematurely, brain reward systems remain vulnerable, cravings return, and tolerance decreases. This combination dramatically increases the risk of relapse and fatal overdose. Studies consistently demonstrate that individuals who stay on MOUD for longer periods have lower rates of relapse, hospitalization, and mortality compared to those who discontinue treatment prematurely.
Extended MOUD treatment also provides a protective structure. Continued medication adherence supports emotional regulation, reduces impulsivity, and allows time for therapy, employment stability, family repair, and healthy routine development. These psychosocial gains strengthen long-term recovery and reduce the likelihood of returning to opioid use.
Another survival benefit comes from reduced exposure to illicit opioids. As fentanyl contamination in drug supplies increases overdose risk, remaining on prescribed MOUD offers a safe, controlled alternative that prevents dangerous fluctuations in opioid tolerance. This protective effect is especially critical during early recovery when relapse risk is highest.
Despite the proven benefits, stigma and misunderstanding often pressure individuals to discontinue MOUD prematurely. Modern addiction science emphasizes that long-term medication is not replacing one addiction with another — it is treating a chronic medical condition. Just as individuals with diabetes require ongoing medication, many people with opioid use disorder need extended MOUD for sustained health.
Extending MOUD duration saves lives. When combined with counseling, self-management strategies, family support, and community resources, long-term medication treatment offers the strongest foundation for survival, recovery, and improved quality of life.
Self-Management Strategies for Staying on MOUD and Increasing Survival Rates
Medication for Opioid Use Disorder (MOUD) is one of the most effective, life-saving treatments for opioid addiction. Medications such as methadone, buprenorphine, and naltrexone reduce cravings, stabilize brain chemistry, and dramatically lower overdose risk. Research consistently shows that individuals who remain on MOUD for extended periods have significantly higher survival rates than those who stop treatment early. However, long-term success depends not only on access to medication but also on active self-management practices that support sustained engagement in care.
A primary self-management strategy is consistent medication adherence. Taking MOUD exactly as prescribed maintains steady opioid receptor stabilization and prevents withdrawal or craving cycles. Using pill organizers, phone reminders, or linking medication routines with daily habits helps prevent missed doses. Regular communication with healthcare providers ensures dosages remain effective as recovery progresses.
Self-monitoring is another essential tool. Tracking cravings, mood changes, stress levels, and sleep patterns helps individuals recognize early warning signs of relapse. Many people benefit from journaling or using recovery apps to share data with treatment teams for timely adjustments in care.
Managing triggers and stress supports long-term medication success. Identifying high-risk situations, developing coping responses, practicing relaxation techniques, and engaging in structured daily routines reduce emotional vulnerability. As brain stability improves on MOUD, practicing these strategies strengthens long-term relapse prevention.
Lifestyle habits also play a key role. Balanced nutrition, hydration, regular physical activity, and consistent sleep schedules enhance medication effectiveness and improve emotional regulation. Avoiding alcohol or non-prescribed substances further protects recovery stability.
Finally, staying connected to support systems reinforces self-management. Peer recovery groups, counseling, telehealth check-ins, and family encouragement provide accountability and motivation. Individuals who view MOUD as part of an ongoing wellness plan—rather than a temporary fix—develop confidence and long-term commitment.
Self-management transforms extended MOUD treatment into a daily practice of recovery. When individuals actively participate in their care, remain consistent with medication, and build supportive routines, survival rates increase, relapse risk decreases, and lasting recovery becomes achievable.
Family Support Strategies for Extended MOUD Treatment and Increased Survival Rates
Medication for Opioid Use Disorder (MOUD) is one of the most powerful tools in reducing overdose deaths and improving long-term recovery outcomes. Medications such as methadone, buprenorphine, and naltrexone stabilize brain chemistry, reduce cravings, and protect individuals from the dangers of illicit opioid use. Research consistently shows that people who remain on MOUD for longer periods have significantly higher survival rates. Family support plays a crucial role in helping individuals stay engaged in extended medication treatment.
One important family strategy is to recognize that MOUD is a long-term medical treatment, not a temporary detoxification tool. When families learn that opioid use disorder is a chronic brain condition, they are more likely to support continued medication rather than pressure loved ones to stop early. Education reduces stigma and replaces judgment with informed encouragement.
Families can also support medication adherence. Helping establish daily routines, offering transportation to clinic appointments, or providing gentle reminders promotes consistency without becoming controlling. Celebrating treatment milestones reinforces motivation and confidence.
Emotional support is equally essential. Individuals adjusting to long-term MOUD may experience frustration, shame, or fear of being judged for staying on medication. Families that practice active listening, calm communication, and reassurance create a safe environment where recovery can continue without secrecy or isolation.
Creating a stable home environment further strengthens treatment success. Removing substance-related triggers, encouraging healthy routines, and participating in positive shared activities reduce relapse risk. Family involvement in counseling or education sessions also helps identify early warning signs and crisis-response plans.
Finally, families must practice healthy boundaries. Supporting recovery entails encouraging independence and personal responsibility, rather than controlling treatment decisions. Balanced involvement builds trust and self-efficacy.
When extended MOUD treatment is combined with strong family support, survival rates improve, relapse risk decreases, and long-term recovery becomes more sustainable. Families who learn, support, and grow together become a powerful force in saving lives and rebuilding futures.
Community Resource Strategies for Extended MOUD Treatment and Increased Survival Rates
Medication for Opioid Use Disorder (MOUD) is a proven, life-saving treatment that reduces cravings, prevents withdrawal, and protects individuals from fatal overdose. Medications such as methadone, buprenorphine, and naltrexone stabilize brain function and allow people to rebuild their lives. Research consistently shows that individuals who remain on MOUD for extended periods have significantly higher survival rates. Community resources play a vital role in making long-term treatment accessible, consistent, and sustainable.
A key community strategy is expanding access to MOUD services. Community health centers, outpatient clinics, mobile treatment units, and telehealth programs allow individuals to receive medication management without long travel distances or long waitlists. Pharmacies that collaborate with treatment programs further enhance convenience and continuity of care.
Provider training is another essential resource. Communities that invest in the education of physicians, nurses, counselors, and peer recovery coaches in MOUD delivery reduce treatment gaps and stigma. When providers understand that extended medication treatment saves lives, individuals receive more consistent encouragement to stay in care.
Peer recovery networks strengthen long-term engagement. Community-based recovery groups, mentoring programs, and harm-reduction organizations provide accountability, shared experience, and emotional support. These connections help individuals remain motivated to continue medication treatment through challenges.
Practical support services also remove barriers to extended MOUD use. Transportation assistance, housing programs, employment services, and legal aid help stabilize daily life, thereby ensuring that treatment remains a priority. When basic needs are met, individuals are far more likely to stay engaged in care.
Finally, public education campaigns play a powerful role. Communities that promote MOUD as a legitimate medical treatment reduce stigma and encourage families and individuals to seek help early and remain in treatment longer.
When community resources align with medical care, extended MOUD treatment becomes realistic and sustainable. With accessible clinics, trained providers, peer support, and social services, survival rates increase, overdose deaths decline, and recovery becomes a lasting possibility rather than a short-term intervention.
Frequently Asked Questions
Here are some common questions:
What is extended MOUD treatment?
Extended MOUD treatment means continuing medications for opioid use disorder — such as methadone, buprenorphine, or naltrexone — for long periods rather than stopping after short-term stabilization.
Why is extended MOUD treatment important?
Opioid use disorder is a chronic brain condition. Staying on MOUD long-term keeps brain chemistry stable, reduces cravings, and lowers the risk of relapse and fatal overdose.
Does longer MOUD treatment really increase survival rates?
Yes. Research consistently shows that individuals who remain on MOUD for extended periods have significantly lower overdose death rates and higher long-term recovery success.
Is extended MOUD replacing one addiction with another?
No. MOUD medications are medically supervised treatments that stabilize brain function and do not produce the harmful compulsive behaviors seen in addiction.
How long should someone stay on MOUD?
There is no fixed timeline. Duration depends on individual needs, recovery stability, mental health, and medical guidance. Many benefit from months or years of treatment.
What happens if MOUD is stopped too early?
Stopping medication prematurely increases withdrawal, cravings, relapse risk, and vulnerability to fatal overdose due to lost tolerance.
Can someone function normally while on MOUD?
Yes. Most individuals on stable MOUD doses work, attend school, care for their families, and lead productive lives.
What side effects occur with long-term MOUD?
Side effects vary by medication but are usually manageable under medical supervision. Providers monitor health regularly during extended treatment.
Does extended MOUD include counseling?
Yes. Medication works best when combined with therapy, peer support, and recovery planning.
Can families support long-term MOUD?
Absolutely. Family encouragement, education, and emotional support improve treatment engagement and success.
Are community resources important for extended MOUD?
Yes. Access to clinics, telehealth, peer groups, transportation, and housing services helps individuals remain in long-term care.
Where can someone access extended MOUD treatment?
Addiction specialists, primary care providers, community health clinics, and behavioral health centers offer MOUD programs.
Conclusion
Extended MOUD treatment saves lives, but its full benefits are realized when combined with daily self-management practices, compassionate family support, and accessible community services. Self-management fosters consistency and personal responsibility; families provide emotional stability and encouragement; and community resources remove barriers to ongoing care. When these elements work together, individuals are more likely to remain in treatment, avoid relapse, and achieve lasting recovery. As addiction care continues to evolve, integrating extended medication treatment with supportive personal and social strategies offers the strongest foundation for survival, healing, and long-term wellness in opioid use disorder.
Video: Extended MOUD Saves Lives #addictiontreatment #overdoseprevention