Alcohol treatment in the U.S. has evolved from institutional care to personalized approaches like therapy, medication, and digital tools. While offering more options, these also come with challenges, including high costs, access gaps, and ethical concerns. The best treatment depends on individual readiness, health, values, and support for a genuinely effective recovery.
From Asylums to Recovery Ecosystems: A Brief History of Alcoholism Treatment Facilities in the U.S.
The evolution of alcoholism treatment facilities in the United States tells a powerful story—one that mirrors changing beliefs about addiction, the role of science and society, and how we care for people in recovery. What began as moral reform efforts rooted in stigma has grown into a diverse system of care emphasizing health, evidence, and long-term support.
Let’s take a concise walk through the major milestones that shaped today’s alcoholism treatment landscape:
🏛️ 18th–19th Century: Moral Reform & Temperance
- Early Beliefs: Alcoholism was seen primarily as a moral failure or sin. Treatment, if offered, was spiritual or punitive.
- Temperance Movement (1800s): Sparked widespread abstinence campaigns and led to early sober societies, such as the Washingtonian Movement (1840), which pioneered peer support.
- Inebriate Homes and Asylums: Facilities like the New York State Inebriate Asylum (1864) became the first in the U.S. dedicated solely to addiction treatment, though rooted in isolation and moral reform.
🏥 Early 20th Century: Medicalization & Institutionalization
- Prohibition (1920–1933): While alcohol was banned, dependence was not treated; many with AUD were placed in jails or psychiatric hospitals.
- Medical Voices: Figures like Dr. Benjamin Rush (early 1800s) and later Dr. E.M. Jellinek (1940s) began reframing alcoholism as a medical disease rather than a character flaw.
🤝 Mid-20th Century: Peer Support & Hospital-Based Care
- Alcoholics Anonymous (AA), 1935: AA’s creation marked a major turning point—its 12-step, peer-based model emphasized spiritual growth and community support, becoming a cornerstone of recovery.
- Hospital Integration (1940s–50s): Institutions like the Yale Center of Alcohol Studies opened the first specialized alcohol treatment units.
- Minnesota Model (1960s): Blended 12-step principles with medical and psychological care—this became the template for modern inpatient rehab centers.
🏢 1970s–1980s: Rise of the Rehab Industry & Public Support
- Federal Action: The 1970 Alcohol Abuse and Alcoholism Prevention, Treatment, and Rehabilitation Act created the NIAAA, boosting research and funding.
- Insurance Coverage Expanded: More people could access inpatient rehab.
- Rehab Boom: Private and nonprofit facilities grew rapidly, popularizing 28-day residential treatment and group therapy models.
🧠 1990s–2000s: Evidence-Based Treatment & Dual Diagnosis
- Mental Health Integration: Recognized that many individuals with AUD also have co-occurring mental health disorders like depression or PTSD.
- New Therapies: Introduction of CBT, Motivational Interviewing, and approved medications like naltrexone and acamprosate.
- Outpatient Expansion: Intensive Outpatient Programs (IOPs) and harm reduction strategies began gaining ground.
🌐 2010s–Present: Innovation, Integration, and Recovery-Oriented Systems
- Affordable Care Act (2010): Made addiction treatment an essential health benefit, expanding access.
- ROSC Model: Shifted focus from isolated treatment episodes to Recovery-Oriented Systems of Care—supporting recovery through housing, employment, peer support, and family engagement.
- Technology & Telehealth: Platforms like teletherapy, apps, and digital recovery tools are now key parts of the treatment landscape.
- MAT Growth: Expanded use of Medication-Assisted Treatment, particularly during the opioid crisis, which also supports many people with alcohol use disorder.
📌 Summary Timeline of Key Developments
| Era | Key Features |
|---|---|
| 1800s | Moral reform, inebriate homes, abstinence societies |
| Early 1900s | Prohibition, institutionalization, medical theories emerge |
| 1930s–50s | AA founded, disease model gains ground |
| 1960s–70s | Minnesota Model, federal treatment funding begins |
| 1980s–90s | Expansion other rehab industry, recognition of dual diagnosis |
| 2000s–2020s | Evidence-based care, MAT, recovery ecosystems, tech integration |
In summary, the history of alcoholism treatment reflects an ongoing shift—from judgment and isolation to evidence-based, compassionate care. While no single approach works for everyone, the most effective treatment is one that is science-informed, culturally competent, and aligned with the individual’s personal goals and values.
Recovery is not a one-size-fits-all journey—it’s a lifelong process of healing, growth, and empowerment. Understanding the path behind us helps illuminate the diverse and hopeful road ahead.
From Asylums to Evidence: How Alcoholism Treatment Evolved Across Centuries
Alcohol treatment has come a long way from its early days of moral judgment and isolation. Through science, cultural shifts, and clinical advances, past approaches have gradually transformed into today’s more compassionate, personalized, and evidence-based methods. Understanding this evolution not only offers historical insight but also highlights how modern recovery pathways continue to be shaped by the successes—and failures—of the past.
Here’s a breakdown of historical treatments and how they contributed to today’s alcoholism care:
1. Inebriate Asylums → Specialized Residential Treatment
Then:
In the 1800s, institutions like the New York State Inebriate Asylum were among the first to offer dedicated spaces for those struggling with alcohol use. These environments were moralistic and custodial, relying heavily on isolation and abstinence.
Now:
These early models laid the groundwork for today’s residential treatment centers. Modern programs provide structured, therapeutic environments with medical detox, psychological support, and peer-led groups. Models like the Minnesota Model integrate medical staff, 12-step facilitation, and individual care plans.
2. Moral Reform & Temperance Movements → Peer Support & Abstinence Models
Then:
Groups like the Washingtonian Society in the 1840s emphasized abstinence through peer support and moral persuasion, often influenced by religious values.
Now:
This spirit lives on in Alcoholics Anonymous (AA), founded in 1935. AA’s 12-step model remains a cornerstone of recovery support, focusing on fellowship, spiritual growth, and personal accountability.
3. Institutional “Drying-Out” → Medical Detoxification
Then:
Those with alcohol use disorder were often jailed or institutionalized to “dry out,” without access to proper medical care; treatment was punitive rather than therapeutic.
Now:
Medically supervised detoxification is now the standard, ensuring safe withdrawal through pharmacological support (e.g., benzodiazepines) and monitoring. Detox is recognized as just the first step in a longer recovery process.
4. The Disease Concept (Jellinek Curve) → Modern Medical Model
Then:
In the 1940s–50s, Dr. E.M. Jellinek proposed that alcoholism is a chronic, progressive disease. His work challenged the notion that addiction was purely a moral failing.
Now:
This concept forms the basis of the biopsychosocial model, which views alcohol use disorder as influenced by biological, psychological, and social factors. It paved the way for the integration of treatment into mainstream healthcare.
5. Minnesota Model → Integrated, Multidisciplinary Treatment
Then:
Developed in the 1950s, the Minnesota Model combined 12-step philosophy, professional and peer teams, and family education.
Now:
Most inpatient and outpatient rehabs today use a version of this model, enhanced with evidence-based practices like trauma-informed care, co-occurring disorder treatment, and person-centered planning.
6. Behavioral Therapies → CBT & Motivational Interviewing
Then:
Behavioral treatments in the 1970s and ’80s targeted habits, triggers, and relapse risks.
Now:
These evolved into Cognitive Behavioral Therapy (CBT) and Motivational Interviewing (MI), two gold-standard, science-backed treatments that focus on changing thought patterns and strengthening internal motivation.
7. Punitive Approaches → Recovery-Oriented Systems of Care (ROSC)
Then:
Alcoholism was once criminalized or treated with social exclusion. The Prohibition era reflected broader stigmas toward substance use.
Now:
We now recognize recovery as a long-term, multifaceted process. Recovery-Oriented Systems of Care (ROSC) focus on building recovery capital, peer support, housing, employment, and reintegration into society—rather than punishment.
8. Folk Remedies & Aversion → Medication-Assisted Treatment (MAT)
Then:
Historically, treatments included aversive methods (e.g., emetics) and unproven folk remedies.
Now:
MAT is now an evidence-based pillar of modern treatment. FDA-approved medications like naltrexone, acamprosate, and disulfiram help reduce cravings, support abstinence, and improve recovery outcomes when combined with therapy and support.
📌 Summary Table: The Journey of Alcoholism Treatment
| Historical Practice | Modern Evolution |
|---|---|
| Inebriate asylums | Residential rehab centers |
| Moral reform/temperance | AA, peer support, abstinence models |
| Institutional detox | Medical detox with pharmacological support |
| Disease model (Jellinek) | Biopsychosocial, chronic care model |
| Minnesota Model | Integrated, multidisciplinary treatment programs |
| Early behavioral therapy | CBT, MI, relapse prevention |
| Criminalization/punishment | Recovery-oriented care and legal diversion |
| Aversion/folk remedies | Medication-Assisted Treatment (MAT) |
In conclusion, the history of alcohol treatment is not just a timeline of changing methods—it’s a mirror of evolving beliefs about human behavior, health, and dignity. From asylums and shame-based approaches to personalized, science-driven care, we’ve come a long way. Understanding where we’ve been helps us appreciate the diverse options available today and reminds us that treatment must continue to evolve with compassion, science, and respect for individual experience.
The Future of Alcoholism Treatment: Personalized, Integrated, and Technology-Driven Care
Alcoholism treatment is undergoing a powerful transformation. The traditional model—short-term, abstinence-only rehab—is being replaced by an approach that recognizes addiction as a complex, chronic condition requiring personalized, long-term, and integrative care. Today’s cutting-edge strategies blend science, technology, mental health, and social support to meet individuals where they are and help them build a sustainable path to recovery.
Here’s a look at the latest concepts reshaping how we understand and treat alcohol use disorder (AUD):
Latest Concepts in Treating Alcoholism
1. Personalized & Precision Medicine
Treatment is increasingly tailored to each individual using genetics, brain imaging, and personal history.
- Example: Certain genetic markers predict better responses to medications like naltrexone.
- Future: AI-driven tools may soon recommend custom treatment plans based on a person’s biological and behavioral data.
2. Medication-Assisted Treatment (MAT) Expansion
Medications are no longer seen as optional—they’re becoming central to care.
- Current options:
- Naltrexone: reduces cravings
- Acamprosate: stabilizes brain chemistry
- Disulfiram: discourages drinking via aversion
- Emerging options:
- Topiramate and gabapentin (off-label use)
- Psychedelic therapy (e.g., psilocybin) is showing early success
- Future: MAT will be routinely combined with treatment and peer support.
3. Neuroscience-Based Treatments
New technologies are targeting the brain directly to improve outcomes.
- Methods include:
- Neurofeedback
- Transcranial Magnetic Stimulation (TMS)
- Deep Brain Stimulation (DBS) (experimental)
- Future: These brain-based tools will likely be paired with talk therapy and medications for comprehensive care.
4. Integrated Dual Diagnosis Treatment
Up to half of people with AUD also struggle with mental health conditions.
- Now: Integrated treatment approaches for co-occurring disorders
- Future: Broader use of trauma-informed care and therapies like EMDR, Dialectical Behavior Therapy (DBT), and Acceptance & Commitment Therapy (ACT) in addiction settings.
5. Recovery-Oriented Systems of Care (ROSC)
We’re moving from crisis stabilization to long-term support.
- Includes:
- Peer coaches
- Recovery housing
- Employment and life-skills training
- Family engagement
- Future: Recovery ecosystems will be embedded into communities, providing ongoing, holistic support.
6. Digital & Telehealth Solutions
Technology is closing the gap for people who can’t access in-person treatment.
- Now:
- Teletherapy and virtual Intensive Outpatient Programs (IOPs)
- Apps like reSET-O, SoberGrid for cravings and support
- Future:
- AI therapy bots
- Wearables that track stress, cravings, or alcohol levels
- VR exposure therapy for practicing refusal skills
7. Harm Reduction & Flexible Goals
Abstinence is no longer the only acceptable outcome.
- Now: Programs support reduced drinking and quality-of-life improvements
- Future: More personalized care pathways will reflect individual readiness, culture, and life goals.
8. Culturally-Informed and Equity-Based Care
Treatment is being reshaped to acknowledge systemic factors like poverty, racism, and historical trauma.
- Now: Providers are incorporating Indigenous practices, bilingual services, and community voices
- Future: More inclusive systems will remove barriers and provide truly person-centered care.
Future Practice Modalities in Alcoholism Treatment
| Modality | Description |
|---|---|
| AI-Powered Personalized Plans | Algorithms match individuals to ideal therapies based on genetics and progress. |
| Psychedelic-Assisted Therapy | Use of psilocybin or MDMA in trauma-informed settings. |
| Wearables & Biofeedback | Devices detect early relapse signs and prompt real-time interventions. |
| Virtual Reality Training | VR simulates real-world triggers to build resistance skills. |
| Digital Therapeutics (DTx) | FDA-approved apps that offer behavioral therapy via smartphone. |
| Recovery Ecosystems | Integrated systems including housing, jobs, and peer support. |
| Public Health + Justice Reform | Diversion programs, recovery courts, and treatment over incarceration. |
In summary, today’s alcoholism treatment reflects a significant paradigm shift: from one-size-fits-all rehab to dynamic, long-term care that treats the whole person. The future is personalized, science-based, digitally supported, and socially conscious. While traditional abstinence models remain relevant, what’s emerging is a flexible system that empowers individuals to choose their own path, backed by data, compassion, and community.
Recovery is no longer just about stopping drinking—it’s about rebuilding a life worth staying sober for.
Balancing Progress: The Hidden Challenges of Modern Alcohol Treatment
Modern alcohol treatment is undergoing a revolution. Breakthroughs in neuroscience, digital health, medication-assisted therapy (MAT), and precision medicine are transforming how we understand and treat alcohol use disorder (AUD). These innovations promise more personalized, effective, and flexible pathways to recovery.
But alongside the excitement lies a more complex reality: not all new treatments are equally accessible, equitable, or universally effective. As we adopt new technologies and approaches, it’s critical also to recognize their limitations, risks, and ethical dilemmas.
Here’s a breakdown of the major disadvantages and concerns facing the latest concepts in alcohol treatment:
⚠️ 1. Accessibility and Cost
Advanced treatments like Transcranial Magnetic Stimulation (TMS), psilocybin-assisted therapy, and genetic testing often come with a steep price tag.
- These options are typically found in urban, private, or academic clinics, leaving many patients behind.
- Insurance coverage is inconsistent and rarely includes long-term recovery supports.
- Digital therapy tools require reliable internet, smartphones, and basic tech literacy—not always a given, especially among older adults or low-income populations.
⚠️ 2. Health Equity Gaps
Innovative care models can unintentionally widen disparities in treatment access.
- Rural, underserved, and marginalized groups are often excluded from the latest offerings.
- Cultural and language mismatches between clients and providers reduce trust and treatment effectiveness.
- Those with more “recovery capital”—such as financial security, strong social networks, or higher education—are more likely to benefit from new models.
⚠️ 3. Scientific and Regulatory Uncertainty
Many new treatments sound promising—but not all are ready for widespread use.
- Psychedelic therapy and digital therapeutics are still being studied and lack robust long-term outcomes.
- Premature commercialization could lead to unsafe use or exploitation of vulnerable individuals.
- FDA regulations and DEA restrictions pose legal hurdles that can slow access, even when early evidence is encouraging.
⚠️ 4. Over-Reliance on Technology
While tech-based tools can increase convenience, they may weaken the therapeutic relationship.
- AI therapy bots and app-based interventions risk losing the human connection that is often central to healing.
- Data privacy is a significant concern when sensitive mental health and addiction histories are stored online.
- People with cognitive challenges or trauma histories may find digital-only approaches ineffective or overwhelming.
⚠️ 5. Ethical Dilemmas
With innovation comes responsibility—and many new tools raise ethical red flags.
- Genetic screening can raise concerns about privacy, consent, and potential misuse.
- AI-driven care recommendations may unintentionally reinforce biases or reduce individualized decision-making.
- Psychedelic-assisted therapies pose unique challenges around informed consent, psychological safety, and spiritual boundaries.
⚠️ 6. Fragmentation of Care
As the number of treatment options increases, care can become confusing or disjointed.
- Patients may juggle multiple providers, platforms, or programs without precise coordination.
- The lack of integration between medical, psychological, and community services can undermine outcomes and continuity.
⚠️ 7. Resistance from Traditional Systems
Not all providers or institutions are ready to change.
- 12-step-only models may reject medications or harm-reduction principles.
- Stigma and outdated beliefs persist in healthcare systems, courts, and even some treatment centers.
- This slow adoption of newer approaches delays progress for many who could benefit from alternatives.
⚠️ 8. Commodification of Recovery
When recovery becomes a product, there’s a risk that profit outweighs people.
- Corporate rehab chains and private tech platforms may prioritize branding or business over ethics and outcomes.
- Over-medicalization can overshadow the importance of peer support, community, and lived experience in sustaining recovery.
📌 Summary Table: Disadvantages of Modern Alcohol Treatment
| Disadvantage | Description |
|---|---|
| Cost & Accessibility | High-tech treatments often expensive and limited in availability |
| Health Equity Gaps | Underserved populations may be excluded or poorly served |
| Scientific Uncertainty | New treatments lack long-term outcome data |
| Tech Overuse | Can reduce human connection and exclude digitally underserved individuals |
| Ethical Concerns | Includes privacy, informed consent, and bias in emerging tools |
| Care Fragmentation | Poor coordination among providers and services |
| Traditional Resistance | Hesitance to adopt newer, non-abstinence-based or MAT models |
| Commodification of Care | Risk of shifting focus from people to profits |
In summary, innovation in alcohol treatment is exciting—and necessary. But it must be balanced with caution, compassion, and equity. The most effective recovery systems will be those that integrate cutting-edge science with human-centered care, ensuring that no one is left behind.
As we move forward, it’s critical to ask:
Who benefits from this treatment?
Who might be excluded?
**And how can we ensure every innovation serves the real goal—**not just sobriety, but a fulfilling, self-directed life in recovery?
Actual progress means making recovery not only more effective—but also more inclusive, ethical, and person-centered.
Ethical Dilemmas of Modern Alcohol Treatment: Balancing Innovation with Integrity
As alcohol treatment evolves through neuroscience, AI, psychedelics, and digital platforms, it brings new hope—but also complex ethical dilemmas. These advancements push boundaries of what’s possible, but also force us to ask: Are we doing what’s right—for everyone?
Here are the key ethical challenges shaping the future of alcohol treatment:
⚖️ 1. Informed Consent and Autonomy
Advanced therapies like genetic testing and psychedelic-assisted treatment require clear, detailed explanations. Yet many patients may not fully grasp the risks or long-term effects. In court-mandated or hospital-based treatment, consent may be more pressured than voluntary, blurring ethical lines.
🔐 2. Privacy and Data Security
Digital apps and wearables collect sensitive data—sometimes without users fully understanding how it will be stored or shared. If insurers or employers gain access, there’s a risk of discrimination. Transparency, consent, and security are critical to ethical data use.
⚠️ 3. Equity and Access
High-cost, high-tech treatments like TMS or precision medicine are often out of reach for low-income, rural, or BIPOC communities. While science advances, the ethical question remains: Who gets to benefit?
🌍 4. Cultural Sensitivity and Stigma
Some treatments may clash with cultural or religious beliefs. Harm reduction models may be dismissed in abstinence-only environments—and vice versa. Ignoring cultural perspectives can alienate individuals and reduce treatment effectiveness.
🧪 5. Use of Emerging or Experimental Therapies
Psychedelic-assisted therapies and digital therapeutics hold promise—but many are still experimental. Vulnerable individuals may try unproven treatments out of desperation. Without safeguards, there’s a risk of psychological harm, boundary violations, or exploitation.
🤖 6. Artificial Intelligence in Treatment
AI-driven care plans may automate decisions at the cost of human nuance. Hidden algorithmic biases could misrepresent needs or lead to unequal treatment. The ethical concern: Who is accountable when AI gets it wrong?
⚖️ 7. Autonomy vs. Public Health
Harm reduction strategies that support moderated drinking may conflict with policies promoting abstinence or safety. Ethical tensions arise when personal freedom must be weighed against community risks—like DUI or alcohol-related violence.
🧠 8. Medicalization and Loss of Holistic Recovery
Focusing on medications and brain-based treatments may overshadow critical recovery factors like social support, housing, and purpose. Ethical care should integrate—not replace—community, identity, and lived experience.
📌 Summary Table: Ethical Dilemmas in Modern Alcohol Treatment
| Risks of ignoring holistic, community-based paths to recovery | Description |
|---|---|
| Informed Consent | New treatments may be hard to fully explain or understand |
| Privacy and Data Use | Risk of misuse or exploitation of sensitive health data |
| Health Equity | Limited access for underserved populations |
| Cultural Sensitivity | Treatments may conflict with personal, spiritual, or cultural values |
| Experimental Therapy Risks | Early-stage treatments could exploit desperate or vulnerable individuals |
| AI and Bias | Algorithmic tools may misjudge needs or carry built-in discrimination |
| Autonomy vs. Public Health | Tension between individual choice and societal safety |
| Over-Medicalization | Risks ignoring holistic, community-based paths to recovery |
In summary, ethical care is not just about doing what works—it’s about doing what’s right. As alcohol treatment becomes more technologically advanced, we must ensure it remains human, equitable, and inclusive.
True innovation considers not just outcomes, but also access, dignity, cultural respect, and long-term wellbeing. We can embrace progress without leaving people behind—if ethics stay at the core.
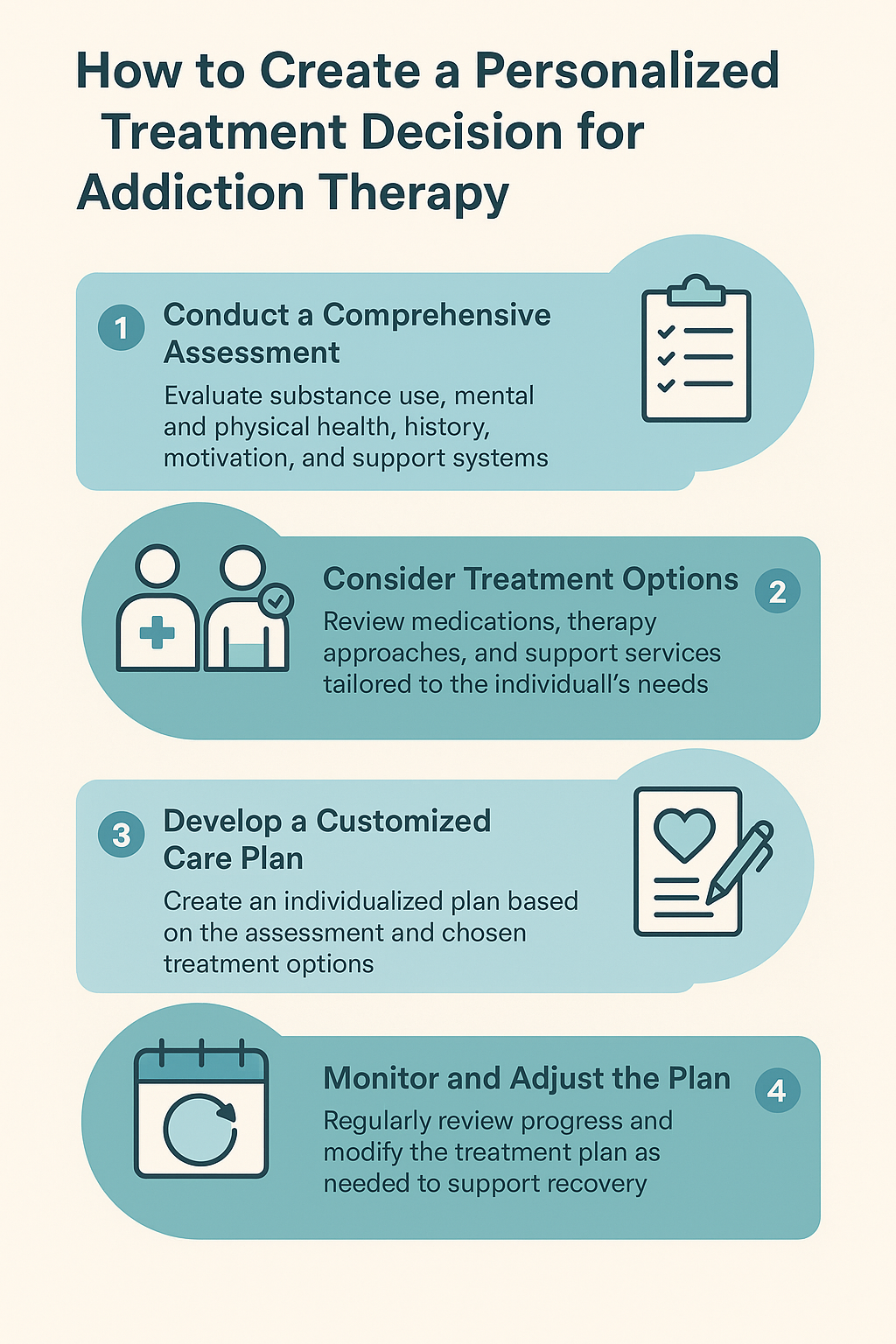
Finding the Right Fit: A Self-Management Guide to Choosing Alcohol Treatment
Choosing a treatment plan for Alcohol Use Disorder (AUD) is a deeply personal decision—there’s no one-size-fits-all approach. With today’s diverse range of treatment options, from inpatient rehab to digital apps, the most successful outcomes often start with self-awareness. That’s where self-management comes in.
Self-management means actively participating in your recovery journey—choosing methods that fit your unique needs, lifestyle, values, and goals. Rather than trying to fit into a rigid program, you design a path that works for you.
Here’s a guide to help you choose the right treatment modality using self-management criteria:
✅ 1. Readiness to Change
Ask Yourself: Am I ready to stop drinking altogether, reduce drinking, or explore my options?
- If you’re ready to stop: Abstinence-based programs like 12-step fellowships (AA) or inpatient rehab may be best.
- If you’re not ready to quit: Try harm reduction approaches, such as moderation-based therapy or medications like naltrexone.
- Not sure yet? Motivational interviewing or pre-treatment counseling can help you clarify your goals.
✅ 2. Level of Alcohol Dependence
Assess severity using tools such as the AUDIT or DSM-5 criteria.
- Mild to Moderate Dependence: Outpatient therapy, counseling, support groups, or self-help apps may be appropriate.
- Severe Dependence or Risk of Withdrawal: You may need medical detox, residential treatment, or MAT (Medication-Assisted Treatment) to ensure safety.
✅ 3. Physical and Mental Health Status
If you have co-occurring mental health conditions like depression, PTSD, or anxiety:
- Look for integrated dual-diagnosis treatment centers.
- Seek therapies like CBT (Cognitive Behavioral Therapy), ACT (Acceptance & Commitment Therapy), or EMDR.
- Chronic medical issues? Choose programs with on-site medical support.
✅ 4. Personal Values and Beliefs
What matters most to you spiritually, culturally, or personally?
- Spiritual or religious: 12-step programs may feel meaningful.
- Secular or science-based: Consider SMART Recovery, CBT, or LifeRing.
- Culturally specific needs: Look for programs that honor your identity—whether based on race, gender, culture, or LGBTQ+ status.
✅ 5. Lifestyle and Daily Responsibilities
Can you step away from your current obligations—or do you need flexibility?
- Inpatient rehab: Intensive, immersive, but requires a time-out from life.
- Outpatient programs or telehealth: Can be scheduled around work, family, or school.
- Self-guided tools/apps: Ideal for privacy, flexibility, or early-stage engagement.
✅ 6. Support System
Do you have a supportive family or peer network?
- Yes: Consider involving them through family therapy or peer support groups.
- No: Look for services that help build community—like group therapy, recovery housing, or recovery coaching.
✅ 7. Access to Resources
Think realistically about what’s available to you:
- Do you have insurance or a way to pay for care?
- Are services nearby?
- Do you have a smartphone or Wi-Fi for digital tools?
Choose a sustainable and affordable option—consistency is more important than complexity.
✅ 8. Treatment Goals
What’s your end goal?
- Abstinence
- Controlled drinking
- Reducing harm
- Improving mental/emotional health
Some programs are strictly abstinence-based, while others support flexible, self-defined goals. Choose what aligns with your values and current phase of recovery.
✅ 9. Learning Style and Preferences
How do you best absorb and apply new information?
- Talk it out? → Choose individual or group counseling.
- Prefer reading and exercises? → Try CBT workbooks, journaling, or online modules.
- Hands-on and experiential? → Explore art therapy, meditation retreats, or nature-based programs.
✅ 10. Track Record and Evidence Base
Are you drawn to scientific backing or peer tradition?
- Evidence-based: CBT, MAT, MI (Motivational Interviewing), DBT.
- Peer-supported: 12-step, spiritual-based programs—less studied, but valuable for many.
If research and outcome data are essential to you, opt for modalities with strong clinical evidence.
📌 Self-Management Decision Checklist
| Do I need medical care, or can I manage outpatient recovery? | Questions to Ask |
|---|---|
| Readiness to Change | Am I ready to stop, reduce, or just explore options? |
| Dependence Level | Do I need medical care or can I manage outpatient recovery? |
| Health Status | Do I need integrated mental or physical health support? |
| Values & Beliefs | Do I prefer spiritual, secular, or culturally tailored approaches? |
| Lifestyle Demands | Can I take time off, or do I need flexible treatment options? |
| Social Support | Do I have people supporting me, or do I need to build community? |
| Financial/Tech Access | Can I afford treatment, and do I have the tech to use digital tools? |
| Recovery Goals | What do I want—abstinence, moderation, harm reduction, or healing? |
| Learning Style | Do I prefer talk therapy, workbooks, or hands-on activities? |
| Treatment Track Record | Do I want evidence-based care or peer-based, traditional methods? |
Frequently Asked Questions
Here are some common questions:
Question: How to create a personalized treatment decision worksheet based on these self-management factors?
Answer:
Step-by-Step Guide: Creating a Personalized Treatment Decision Worksheet
🔹 Step 1: Title & Basic Info
Title: My Alcohol Treatment Decision Worksheet
Optional Fields:
- Name:
- Date:
- Support person/clinician:
🔹 Step 2: Self-Management Criteria Checklist
Create a section for each self-management factor. For each one, include:
- A short explanation
- A few example options
- Checkboxes or space for notes
📋 SAMPLE TEMPLATE: Personalized Treatment Decision Worksheet
🧠 1. Readiness to Change
What stage am I at right now?
☐ I’m ready to stop drinking completely
☐ I want to reduce but not stop drinking
☐ I’m not ready to change, but I want to learn more
Notes: _______________________________________
🔬 2. Level of Alcohol Use/Dependence
What best describes my drinking pattern?
☐ Mild/moderate (I can cut back without withdrawal)
☐ Severe (I may need medical detox)
☐ I’m unsure – I want an assessment
Notes: _______________________________________
❤️ 3. Physical & Mental Health Needs
Do I have co-occurring conditions?
☐ I need integrated mental health/addiction care
☐ I have a chronic health issue (e.g., liver, diabetes)
☐ I need trauma-informed care
Notes: _______________________________________
🌱 4. Personal Beliefs and Values
Which approaches align with my values?
☐ I prefer a spiritual approach (e.g., 12-step)
☐ I prefer a secular or science-based program (e.g., SMART)
☐ I need culturally sensitive care
Notes: _______________________________________
⏰ 5. Time and Lifestyle Fit
What works with my schedule and responsibilities?
☐ Inpatient (I can commit full-time)
☐ Outpatient (I need to work/parent/study)
☐ Telehealth or app-based (most flexible)
Notes: _______________________________________
👥 6. Support System
Who can support my recovery?
☐ I have supportive friends/family
☐ I want to join a peer group
☐ I need to build a new support network
Notes: _______________________________________
💰 7. Cost & Access
What are my limits and options?
☐ I have insurance coverage
☐ I need low-cost or sliding scale options
☐ I can pay out-of-pocket for specialty care
Notes: _______________________________________
🎯 8. Treatment Goals
What do I want to achieve?
☐ Abstinence
☐ Reduced use/harm reduction
☐ Better mental health and well-being
☐ All of the above
Notes: _______________________________________
📚 9. Learning Style and Preferences
How do I engage best with treatment?
☐ I learn through talking (counseling, groups)
☐ I like reading/working independently (apps, workbooks)
☐ I want experiential or creative methods (e.g., art, mindfulness)
Notes: _______________________________________
🧪 10. Evidence and Outcomes
Do I want treatments supported by science?
☐ Yes – I prefer evidence-based methods (CBT, MAT)
☐ I’m open to traditional/peer-led programs
☐ I want to explore both
Notes: _______________________________________
🔍 Final Section: My Top Priorities
What matters most to me in choosing a treatment plan?
(e.g., flexibility, privacy, cultural fit, effectiveness)
📄 How to Use the Worksheet:
- Please bring it to a healthcare provider, recovery coach, or counselor.
- Use it to compare treatment options.
- Please review and update it as your goals and readiness evolve.
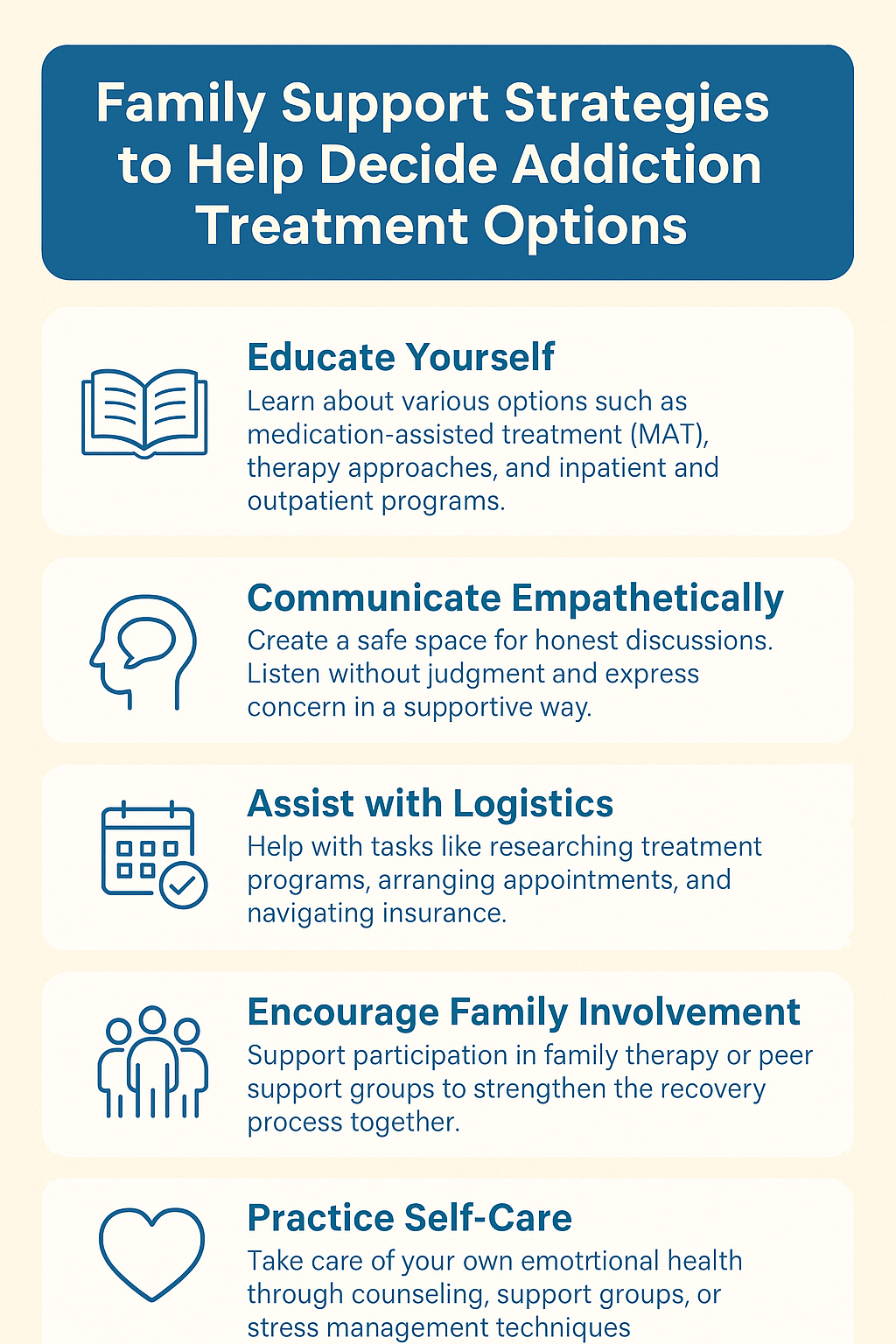
Question: What family support strategies can help decide alcohol treatment options?
Answer: Family Support Strategies for Deciding Alcohol Treatment Options
When a loved one is facing alcohol use disorder (AUD), families often play a critical role in helping identify and choose the most appropriate treatment. But it’s not just about pushing someone into rehab—adequate family support involves understanding, communication, and collaboration. Here are key strategies families can use to support thoughtful, person-centered decisions about alcohol treatment:
✅ 1. Learn About Treatment Options Together
Why it matters: Many families feel overwhelmed or misinformed about what’s available.
What to do:
- Research different modalities together (e.g., inpatient, outpatient, MAT, harm reduction, 12-step, CBT).
- Use credible sources (NIAAA, SAMHSA, Mayo Clinic, etc.).
- Consider attending educational sessions or webinars on addiction treatment.
✅ 2. Respect Autonomy & Readiness to Change
Why it matters: Recovery is most successful when the individual feels empowered to choose.
What to do:
- Use motivational language (e.g., “How do you feel about getting help?”).
- Avoid ultimatums or guilt.
- Recognize that readiness to change may evolve over time (use tools like the Stages of Change model).
✅ 3. Help Identify Personal Goals
Why it matters: Treatment should match the person’s recovery goals—not just the family’s hopes.
What to do:
- Ask: “What do you want out of treatment—abstinence, moderation, better health, mental wellness?”
- Align treatment type with these goals (e.g., harm reduction vs. abstinence-based programs).
- Reassure them that goals can change over time.
✅ 4. Encourage a Health Assessment
Why it matters: Physical and mental health conditions may influence the most suitable care.
What to do:
- Support your loved one in getting an assessment from a primary care provider, psychiatrist, or addiction specialist.
- Offer to go with them to appointments if appropriate and welcomed.
- Ask providers for integrated or dual-diagnosis treatment options if co-occurring issues are present.
✅ 5. Help Navigate Practical Barriers
Why it matters: Access to treatment can be blocked by logistical issues.
What to do:
- Assist with researching insurance coverage, cost estimates, and nearby available services.
- Offer support with transportation, childcare, or time off from work if needed.
- Explore telehealth or online programs for added flexibility.
✅ 6. Consider Family-Inclusive Programs
Why it matters: Family dynamics often impact recovery, and involvement improves outcomes.
What to do:
- Look for programs that include family therapy or education.
- Participate in sessions that focus on communication, boundaries, and support.
- Attend support groups for families (e.g., Al-Anon, SMART Recovery Family & Friends).
✅ 7. Model a Nonjudgmental, Supportive Attitude
Why it matters: Shame and stigma can prevent people from seeking or continuing care.
What to do:
- Express unconditional support: “I care about you, no matter where you are in this process.”
- Validate their efforts, even small steps like attending an assessment or reading about recovery.
- Be patient—relapse or ambivalence doesn’t mean failure.
✅ 8. Promote Self-Management and Shared Decision-Making
Why it matters: Collaborative decision-making increases treatment engagement and outcomes.
What to do:
- Help your loved one explore self-management tools (checklists, apps, workbooks).
- Talk through the pros and cons of different options together.
- Let them take the lead while offering your input and support.
✅ 9. Focus on Long-Term Recovery Support
Why it matters: Recovery doesn’t end after 30 days—families can be long-term allies.
What to do:
- Help explore ongoing options like outpatient therapy, peer recovery coaching, or sober housing.
- Encourage development of a recovery plan that includes social, emotional, and lifestyle goals.
- Maintain open communication and a recovery-friendly home environment.
✅ 10. Take Care of Yourself, Too
Why it matters: Family members often experience stress, burnout, or codependency.
What to do:
- Seek your own support (Al-Anon, therapy, support groups).
- Set boundaries while maintaining compassion.
- Remember: You’re supporting recovery—you’re not responsible for managing it.
🧩 Summary: Family Support Strategies for Treatment Decision-Making
| Strategy | Purpose |
|---|---|
| Learn together | Build shared understanding of treatment options |
| Respect readiness | Support change without pressure or guilt |
| Identify personal goals | Match treatment to individual values and aims |
| Get health assessments | Ensure appropriate clinical support |
| Navigate barriers | Make access to care more realistic and practical |
| Choose family-inclusive programs | Address shared dynamics and foster healing |
| Be nonjudgmental | Reduce shame and increase treatment engagement |
| Promote shared decision-making | Empower loved one with collaborative planning |
| Support long-term care | Emphasize recovery as an ongoing journey |
| Practice self-care | Maintain family well-being and emotional balance |
Final Thought:
Your role as a family member isn’t to control the outcome—but to create a supportive space where your loved one feels safe, respected, and encouraged to make empowered choices about their recovery, when families walk alongside—rather than ahead or behind—the chances of meaningful, sustained recovery grow stronger.
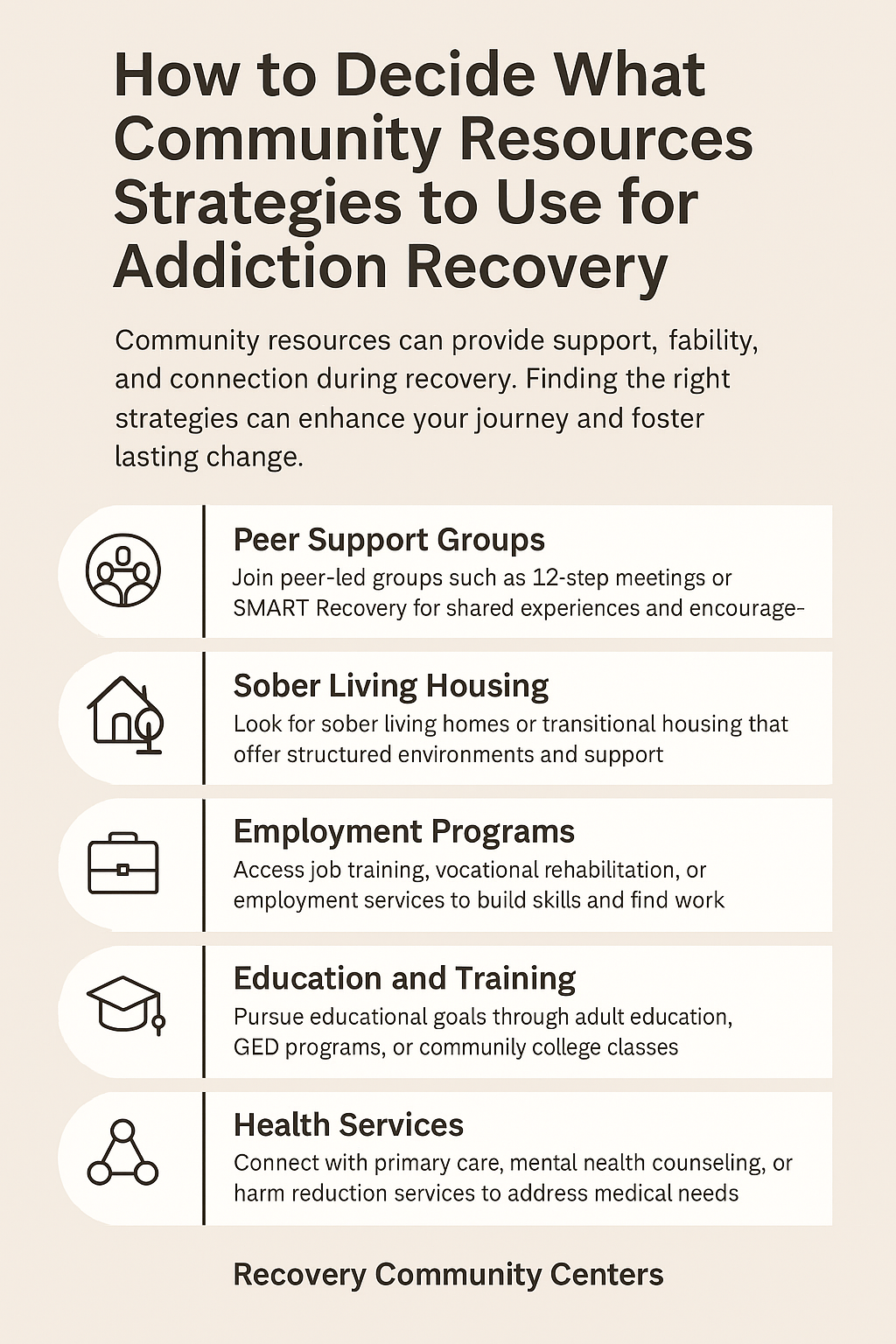
Question: How can an individual decide what community resources and strategies to use for alcohol recovery?
Answer: Deciding which community resource strategies to use for alcohol recovery is an essential step in building a strong support system beyond clinical treatment. Community resources can help address emotional, social, financial, and practical needs—making recovery more sustainable and personalized.
Here’s a structured, self-guided approach to help individuals choose the right community-based strategies for their alcohol recovery:
✅ 1. Assess Your Recovery Needs
Start by identifying the specific areas of your life that could benefit from support.
Ask Yourself:
- Do I need emotional support or connection?
- Am I struggling with housing, employment, or legal issues?
- Do I need sober social activities or mentorship?
- Would peer support or spiritual guidance help?
🧩 Strategy: Make a “Recovery Needs Checklist” to clarify which areas to focus on.
✅ 2. Define Your Recovery Goals
Different community resources support different types of recovery goals.
Examples:
- Abstinence: Choose abstinence-based support groups like Alcoholics Anonymous (AA) or Celebrate Recovery.
- Harm Reduction: Look for groups like Moderation Management or clinics that support controlled use goals.
- Whole-life recovery: Seek programs offering help with employment, housing, or parenting (e.g., recovery community centers).
🎯 Choose strategies that align with your personal definition of recovery.
✅ 3. Consider Cultural and Personal Fit
Not all community resources are equally helpful to everyone—match services to your identity, values, and comfort level.
Ask Yourself:
- Do I prefer secular or spiritual spaces?
- Do I feel more comfortable in groups that share my cultural, racial, or gender identity?
- Do I want structured meetings or informal, peer-based support?
🌐 Look for culturally-specific recovery programs, LGBTQ+ friendly spaces, or bilingual services.
✅ 4. Evaluate Accessibility and Logistics
A great resource isn’t helpful if you can’t access it consistently.
Consider:
- Location (Is it near you?)
- Cost (Free, sliding scale, or paid?)
- Format (In-person, online, hybrid?)
- Schedule (Does it work with your work/family obligations?)
📲 Use directories like SAMHSA Treatment Locator, 211.org, or local United Way services to search by zip code.
✅ 5. Start Small and Experiment
It’s okay not to know what will work—try a few options and observe how they feel.
Examples:
- Attend different peer support meetings (AA, SMART Recovery, LifeRing).
- Visit a local Recovery Community Organization (RCO) or recovery café.
- Try a sober group activity (e.g., art therapy, a fitness group, or a mutual aid event).
🧪 Keep an open mind. You don’t have to commit immediately—just explore.
✅ 6. Ask for Peer Recommendations
Others in recovery can share what worked for them.
Where to ask:
- Support groups
- Online recovery communities (e.g., Reddit’s r/stopdrinking, InTheRooms)
- Peer recovery coaches or mentors
👥 Peer advice is especially valuable for discovering local, lesser-known resources.
✅ 7. Use Community-Based Professionals
Don’t overlook help from non-clinical professionals in your area.
Examples:
- Peer Recovery Coaches: Trained individuals with lived experience in recovery.
- Faith leaders: Spiritual or pastoral counseling.
- Social workers or case managers: Help navigate services like housing, benefits, or transportation.
💡 These professionals can help bridge the gap between clinical treatment and real-world recovery.
✅ 8. Build a Recovery Ecosystem
Use a combination of community resources that meet different needs.
Example Recovery Resource Mix:
| Area of Need | Resource Example |
|---|---|
| Emotional support | AA or SMART Recovery group |
| Housing or legal aid | Local Recovery Community Organization |
| Vocational support | Job placement services or workforce center |
| Spiritual guidance | Faith-based recovery group or clergy |
| Fun/sobriety activities | Sober sports, art, music, or game nights |
🔄 Revisit and adjust your ecosystem as your recovery progresses.
✅ 9. Trust Your Intuition and Feedback
You are the expert on what feels right for your recovery.
Ask Yourself After Trying a Resource:
- Did I feel welcomed and respected?
- Did I leave feeling stronger or overwhelmed?
- Can I see myself returning?
🧭 Your emotional response is a powerful guide.
✅ 10. Stay Flexible and Reassess Often
Your needs will evolve. Periodically ask:
- “What’s missing in my recovery right now?”
- “What’s working well—and what’s not?”
Add, remove, or adjust strategies based on what supports your growth and stability.
📌 Summary: Self-Guided Questions to Choose Community Resources
| Criteria | Key Questions |
|---|---|
| Recovery Needs | What areas of life need the most support right now? |
| Goals | Am I aiming for abstinence, harm reduction, or lifestyle change? |
| Cultural/Personal Fit | Do I feel safe and seen in this space? |
| Accessibility | Can I access it easily and regularly? |
| Peer Recommendations | What do others in recovery suggest? |
| Professional Guidance | Who can help me coordinate and connect? |
| Experimentation | Am I willing to try and see what works? |
| Integration | Do I have a mix of supports covering different areas? |
| Emotional Feedback | How did I feel after participating? |
| Flexibility Over Time | Do I review and adapt my plan as I grow? |
🌱 Final Thought
Choosing community resources is an act of empowerment. You’re not just finding help—you’re building a life around recovery. The right strategies don’t just support sobriety—they help you feel connected, understood, and fulfilled.
When you take the time to explore and choose what works for you, your recovery becomes not just possible—but deeply personal and sustainable.
Conclusion
The evolution of alcohol treatment—from early abstinence-based models to today’s diverse, science-backed modalities—reflects growing recognition of addiction as a complex, treatable condition. While modern treatments offer more personalized and flexible options, they also introduce challenges, including unequal access, ethical concerns, and risks of over-reliance on technology or medication. Navigating these options requires individuals to carefully assess their readiness, personal goals, and health needs. A thoughtful, self-guided approach ensures the chosen treatment not only aligns with evidence but also respects individual values and long-term recovery success.
Videos: What’s the BEST Community Resource for Your Addiction Recovery Needs?
What Are the Best Ways to Support a Loved One With Addiction?
Is PERSONALIZED Addiction Therapy the KEY to Lasting Recovery?