Dual addiction disorder, also known as co-occurring disorders, involves the simultaneous presence of two or more substance use disorders or mental health conditions. Treating this complex issue is challenging, especially in rural areas with limited access to care. However, communities can take steps to overcome barriers by expanding telehealth services, increasing awareness, developing culturally competent care, and strengthening peer support networks. These efforts can improve access to comprehensive treatment and support individuals in rural communities on their recovery journeys.
Understanding Dual Addiction Disorders: Challenges and Treatment Approaches
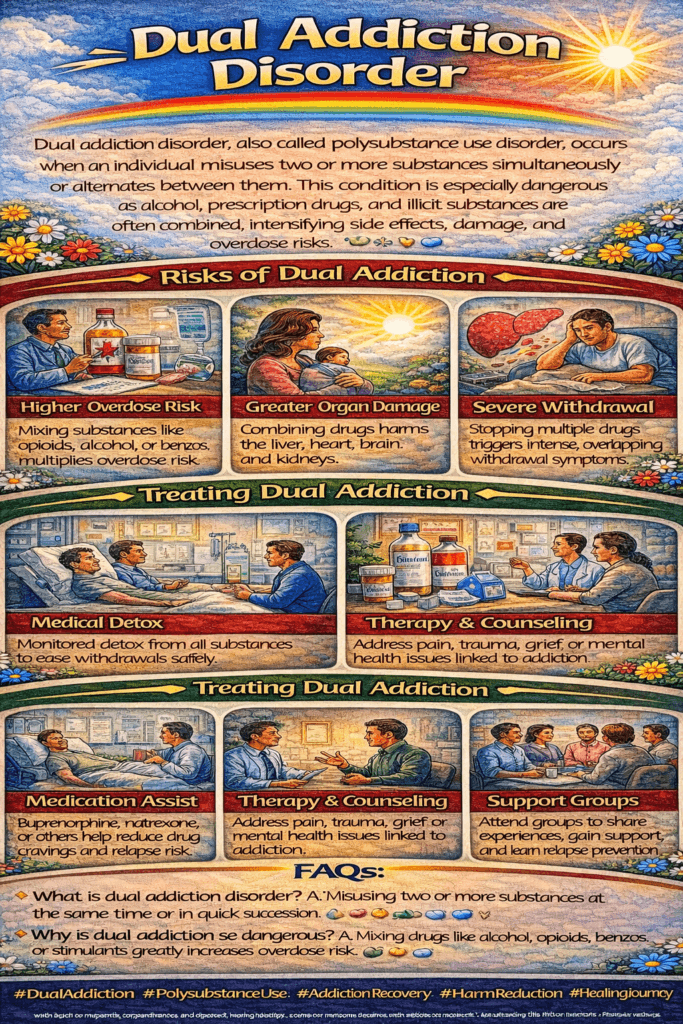
Dual addiction disorders, also known as co-occurring disorders or comorbidities, refer to the presence of two or more substance use disorders or mental health conditions co-occurring in an individual. This complex condition typically involves struggling with addiction to multiple substances, such as alcohol and opioids, or dealing with addiction alongside mental health issues like depression, anxiety, or bipolar disorder. Dual addiction can significantly complicate diagnosis, treatment, and recovery, as each condition may interact and exacerbate the symptoms of the other. Understanding these challenges and adopting integrated treatment approaches are crucial for effective management.
What Are Dual Addiction Disorders?
Dual addiction disorders occur when an individual is affected by more than one substance use disorder or a combination of substance use and mental health disorders. These conditions often co-exist, making it difficult to separate their effects. The interaction between multiple addictions or between substance use and mental health issues can intensify symptoms and create a more challenging path to recovery.
Common Examples of Dual Addiction Disorders
- Alcohol and Opioid Use Disorder: Individuals who struggle with both alcohol and opioid addiction may face compounding health risks. The combined effects of these substances on the central nervous system can increase the risk of overdose and exacerbate cognitive and motor impairments. The challenge in treatment lies in addressing the withdrawal symptoms of both substances simultaneously.
- Cocaine and Marijuana Use Disorder: Dual addiction to cocaine and marijuana can impair judgment, lead to cognitive deficits, and increase risk-taking behavior. Those experiencing this dual addiction often struggle with co-occurring mental health conditions like anxiety or depression, complicating their treatment.
- Methamphetamine and Benzodiazepine Use Disorder: Both methamphetamine and benzodiazepines are highly addictive, with contrasting effects on the brain. Methamphetamine is a stimulant, while benzodiazepines are depressants. Combining these substances can result in severe health complications, including cardiovascular problems, psychosis, and an increased risk of overdose.
- Heroin and Stimulant Use Disorder: Dual addiction to heroin and stimulants, such as cocaine or methamphetamine, can lead to intense cravings and mood swings. The combination of these substances often results in physical and psychological health issues, and individuals may experience difficulties in maintaining stable employment or relationships.
- Alcohol and Prescription Medication Misuse: When alcohol use disorder co-occurs with the misuse of prescription medications, such as opioids, benzodiazepines, or stimulants, the health risks multiply. Overdose, liver damage, and cognitive impairment are significant concerns, requiring a careful balance in treatment.
- Opioid and Sedative Use Disorder: Combining opioids with sedative medications, such as benzodiazepines or sleep aids, increases the risk of respiratory depression, overdose, and other life-threatening reactions. Treatment needs to address the dependence on both substances with a careful, often slower detox process.
- Cannabis and Tobacco Use Disorder: Dual addiction to cannabis and tobacco can result in chronic respiratory issues and cardiovascular problems. These substances may be used together to enhance effects or alleviate withdrawal symptoms, creating a reinforcing cycle of dependence.
Challenges in Diagnosis and Treatment
Diagnosing dual addiction disorders can be complex due to the overlapping symptoms of substance use and mental health conditions. For example, it may be challenging to determine whether a symptom, such as anxiety, is due to a mental health disorder or substance withdrawal. A comprehensive assessment is essential to distinguish between the effects of different substances and any underlying mental health conditions.
Treatment for dual addiction disorders requires an integrated approach that addresses both substance use and mental health concerns concurrently. This means employing a combination of medication-assisted treatment (MAT), behavioral therapy, counseling, and support groups to target all aspects of an individual’s condition.
Effective Treatment Approaches
- Integrated Treatment Programs: These programs combine substance use and mental health treatment in a single setting, ensuring that both conditions are addressed simultaneously. Coordinated care among healthcare providers allows for a holistic approach that can improve outcomes.
- Medication-Assisted Treatment (MAT): MAT may be used to manage withdrawal symptoms and reduce cravings for substances like opioids and alcohol. It can also help stabilize mood and reduce the risk of relapse for individuals with co-occurring mental health disorders.
- Cognitive Behavioral Therapy (CBT): CBT is an evidence-based approach that helps individuals identify and change harmful thoughts and behaviors associated with substance use and mental health conditions. It can be particularly beneficial in managing the psychological aspects of addiction.
- Support Groups and Peer Support: Groups such as Narcotics Anonymous (NA) or Dual Recovery Anonymous (DRA) offer peer support from individuals with similar experiences. This shared understanding can provide encouragement and motivation during recovery.
- Family Therapy: Involving family members in the treatment process can improve outcomes, as family dynamics often play a role in the development and maintenance of dual addiction disorders. Family therapy helps to educate loved ones about addiction and recovery, creating a supportive environment.
- Relapse Prevention Strategies: Sustaining recovery requires developing relapse prevention plans that include coping skills for managing triggers and stress. This may involve lifestyle changes, stress management techniques, and ongoing counseling.
Dual addiction disorders present unique challenges in treatment, as the interplay between multiple substances or between substance use and mental health issues can intensify symptoms and complicate recovery. Effective treatment requires an integrated approach that addresses all aspects of an individual’s condition, from substance use to co-occurring mental health concerns. With a comprehensive treatment plan, individuals with dual addiction disorders can achieve long-term recovery and improve their quality of life.
Understanding, recognizing, and addressing the complexities of dual addiction disorders are essential steps toward better health outcomes and a more supportive approach to managing the opioid crisis and substance use issues overall.
Strategies for Effectively Treating Dual Addiction Disorders
Treating dual addiction disorders—where an individual struggles with two or more substance use disorders or co-occurring mental health conditions—requires a comprehensive and integrated approach. Each condition can exacerbate the other, making the recovery process more challenging. However, with the right strategies, individuals can achieve sustainable recovery and improve their quality of life. Here are several commonly used treatment strategies for managing dual addiction disorders:
1. Comprehensive Assessment
The first step in treating dual addiction disorder is conducting a thorough evaluation to assess the extent and nature of each condition. This assessment includes analyzing substance use patterns, mental health symptoms, medical history, and social support systems. A comprehensive understanding of the individual’s situation allows for the development of a tailored and effective treatment plan.
2. Integrated Treatment Plans
Integrated treatment involves simultaneously addressing substance use disorders and co-occurring mental health conditions. Treatment plans must be personalized to meet each individual’s unique needs. An integrated approach may include a combination of individual therapy, group therapy, medication management, and psychosocial interventions. Integrated treatment can improve overall outcomes by targeting all aspects of an individual’s health.
3. Psychotherapy
Evidence-based psychotherapies are a cornerstone in the treatment of dual addiction disorders. Some commonly used therapies include:
- Cognitive-Behavioral Therapy (CBT): CBT helps individuals identify and change negative thought patterns that contribute to substance use and mental health symptoms. It equips individuals with coping skills for managing cravings and addressing triggers.
- Dialectical Behavior Therapy (DBT): DBT focuses on improving emotional regulation, mindfulness, and distress tolerance. It is beneficial for individuals with co-occurring conditions such as borderline personality disorder.
- Motivational Interviewing (MI): MI helps individuals explore their motivations for change, overcome ambivalence, and set achievable recovery goals. It is effective in promoting treatment engagement.
4. Medication-Assisted Treatment (MAT)
MAT can be an effective tool for managing withdrawal symptoms and reducing cravings associated with substance use disorders. The choice of medication depends on the substances involved. Common medications include:
- Buprenorphine and Methadone: Used for opioid use disorder to reduce withdrawal symptoms and cravings.
- Naltrexone: Can be used for both opioid and alcohol use disorders to block the effects of these substances and reduce cravings.
- Acamprosate: Helps individuals with alcohol use disorder maintain abstinence by reducing cravings.
Combining MAT with therapy ensures a more holistic approach to recovery.
5. Dual Diagnosis Support Groups
Support groups specifically designed for individuals with co-occurring disorders offer a safe space for sharing experiences, receiving peer support, and gaining insights into managing both substance use and mental health challenges. Dual Recovery Anonymous (DRA) and other similar groups focus on the unique experiences of individuals with dual addiction disorders, providing valuable encouragement and motivation for sustained recovery.
6. Family Therapy
Family therapy can play a significant role in the recovery process. Involving family members in treatment helps to improve communication, resolve conflicts, and strengthen relationships. It also allows family members to gain a better understanding of addiction and mental health issues, enabling them to provide better support. Addressing family dynamics that may contribute to substance use or exacerbate mental health symptoms is crucial for long-term success.
7. Holistic Approaches
Incorporating holistic therapies can promote overall well-being and support recovery from both addiction and mental health disorders. These approaches may include:
- Mindfulness and Meditation: Helps individuals manage stress and stay grounded in the present moment.
- Yoga and Exercise: Physical activity can improve mood, reduce stress, and promote overall health.
- Nutrition Counseling: A balanced diet can support physical and mental health during recovery.
- Stress Reduction Techniques: Teaching individuals how to cope effectively can help prevent relapse.
8. Continuing Care and Aftercare
Establishing a relapse prevention plan and accessing ongoing support through outpatient therapy, support groups, and community resources are crucial for maintaining recovery. Aftercare programs can include sober living arrangements and ongoing counseling to help individuals stay on track. Monitoring progress and making necessary adjustments to the treatment plan can prevent relapse and promote long-term recovery.
9. Collaboration with Other Providers
Coordinating care with other healthcare providers ensures that all aspects of an individual’s health are addressed. This collaboration may involve psychiatrists, primary care physicians, and specialists working together to provide comprehensive treatment for both substance use and mental health conditions. An interdisciplinary approach improves the quality and effectiveness of care.
10. Cultural Sensitivity and Trauma-Informed Care
Recognizing the impact of cultural factors and past trauma on an individual’s recovery journey is crucial for effective treatment. Providing culturally sensitive and trauma-informed care can enhance treatment outcomes by creating a safe and supportive environment. This approach involves understanding the individual’s background, respecting cultural differences, and addressing any trauma-related issues that may be contributing to substance use or mental health conditions.
In summary, treating dual addiction disorders requires a holistic and multidisciplinary approach that addresses the complex interplay between substance use and mental health conditions. By integrating evidence-based therapies, medication management, family involvement, and ongoing support, individuals can achieve sustained recovery and improved quality of life. With a comprehensive treatment strategy, individuals with dual addiction disorders can navigate the challenges of recovery and build a healthier, more fulfilling future.
Recovery is possible with the right combination of treatments, support, and a commitment to healing. By embracing integrated and individualized approaches, healthcare providers and communities can help individuals overcome dual addiction disorders and thrive in recovery.
Overcoming Barriers to Treating Dual Addiction Disorder in Rural Communities
Treating dual addiction disorder—when an individual struggles with two or more substance use disorders or co-occurring mental health conditions—in rural communities presents unique challenges. These challenges stem from various barriers that hinder access to comprehensive care and complicate the recovery process. Understanding these barriers and implementing strategies to overcome them is essential for improving treatment outcomes for individuals in rural areas. Here are some common treatment barriers for dual addiction disorder in rural communities and potential solutions:
1. Limited Access to Treatment Facilities
Rural areas often have fewer healthcare facilities and treatment centers, making it difficult for individuals to access specialized care for substance use disorders and mental health conditions. This scarcity limits the availability of detox programs, inpatient facilities, and outpatient clinics, which are crucial for treating dual addiction disorders.
Solution: Expanding mobile treatment services, establishing satellite clinics, and increasing the number of community health centers can help bridge the access-to-care gap. Partnerships with urban treatment centers can also allow for outreach programs that periodically bring specialized services to rural communities.
2. Transportation Challenges
Reliable transportation options can be limited in rural areas, making it difficult for individuals to travel to treatment centers or attend therapy sessions regularly. Long distances between home and treatment facilities add to the logistical challenges.
Solution: Developing transportation assistance programs, offering gas vouchers, and utilizing telehealth for therapy sessions can reduce the burden of travel. Additionally, arranging mobile clinics or transportation services can improve access to care for individuals without personal vehicles.
3. Shortage of Mental Health Professionals
Rural communities may face a shortage of mental health professionals, including psychiatrists, psychologists, and counselors. This shortage makes it difficult to access specialized care for co-occurring disorders, which often require the expertise of trained professionals.
Solution: Incentivizing healthcare providers to practice in rural areas through loan forgiveness programs, tax benefits, and competitive salaries can help attract more mental health professionals. Implementing training programs that empower existing healthcare workers to provide essential mental health and addiction services can also mitigate the effects of workforce shortages.
4. Stigma and Privacy Concerns
In small, close-knit rural communities, higher levels of stigma surrounding mental health and addiction can prevent individuals from seeking treatment. Concerns about confidentiality and fear of judgment may deter individuals from accessing necessary care.
Solution: Community education initiatives aimed at reducing stigma can help shift attitudes toward addiction and mental health. Encouraging anonymous or private telehealth services can also alleviate concerns about confidentiality and make individuals more comfortable seeking help.
5. Limited Insurance Coverage
Rural residents may have limited access to health insurance coverage or face higher out-of-pocket costs for treatment, making it financially challenging to access comprehensive care for dual addiction disorder.
Solution: Expanding Medicaid coverage and advocating for insurance policies that include mental health and addiction treatment can help reduce financial barriers to care. Community health centers that offer sliding scale fees based on income can also provide affordable options for those without insurance.
6. Lack of Culturally Relevant Services
Treatment programs in rural areas may not always be tailored to meet the unique cultural needs and preferences of rural residents. This lack of culturally competent care can lead to lower engagement and retention in treatment.
Solution: Offering culturally relevant treatment approaches that respect local traditions, values, and language can increase engagement. Training providers in cultural competence and incorporating local customs into treatment planning can make services more accessible and acceptable to rural populations.
7. Isolation and Social Support
Social isolation is often more pronounced in rural areas due to geographical distances and limited access to support networks. This can exacerbate feelings of loneliness and make it difficult for individuals to find the social support needed for recovery.
Solution: Establishing local support groups, peer recovery networks, and community-based recovery programs can help reduce isolation. Using telehealth platforms to connect individuals with online support groups can also provide a sense of community and encouragement.
8. Barriers to Telehealth Services
While telehealth can help address access-to-care gaps, challenges such as limited internet connectivity and low technological literacy may prevent rural residents from effectively using these services.
Solution: Expanding broadband access in rural areas and providing technology training programs can improve the feasibility of telehealth. Offering phone-based services as an alternative to internet-based telehealth can also help reach individuals with limited connectivity.
9. Limited Availability of Medication-Assisted Treatment (MAT)
Access to medication-assisted treatment for opioid use disorder, such as buprenorphine or methadone, may be limited in rural areas due to regulatory restrictions, lack of prescribing providers, or challenges with pharmacy access.
Solution: Expanding the number of qualified healthcare providers who can prescribe MAT, allowing nurse practitioners and physician assistants to provide MAT, and offering tele-MAT services can improve access. Establishing community-based dispensing programs can also help ensure individuals can access these critical medications.
10. Workforce Shortages
Rural communities often struggle to recruit and retain qualified healthcare professionals, including addiction specialists and mental health providers. This exacerbates existing barriers to accessing comprehensive treatment for dual addiction disorders.
Solution: Workforce development initiatives can address these shortages by offering financial incentives to healthcare professionals who commit to practicing in rural areas for a specified period. Additionally, expanding training opportunities for rural residents seeking careers in healthcare can help build a local workforce.
Overall, addressing the treatment barriers for dual addiction disorder in rural communities requires a multifaceted approach that includes expanding telehealth services, increasing funding for rural healthcare infrastructure, and providing culturally competent care. By reducing stigma through community education initiatives and implementing policies that incentivize healthcare providers to practice in rural areas, rural communities can make significant strides in improving access to comprehensive care for dual addiction disorder.
To overcome these challenges, collaboration between government agencies, healthcare organizations, community leaders, and advocacy groups is essential. By working together, we can ensure that individuals in rural communities receive the support they need to recover and improve their quality of life. With targeted strategies and a commitment to equity, it is possible to make substantial progress in overcoming the barriers to treating dual addiction disorders in rural settings.
How Communities Can Combat Barriers to Treatment for Dual Addiction Disorder
Communities play a crucial role in overcoming barriers to treatment for dual addiction disorder, where individuals face both substance use and mental health challenges simultaneously. By taking proactive steps to improve access to care, provide support services, and foster a recovery-friendly environment, communities can help individuals achieve lasting recovery. Here are several strategies communities can implement to address these challenges effectively:
1. Expand Access to Telehealth Services
Communities can advocate for expanding telehealth services to overcome barriers related to transportation, geographic isolation, and limited availability of healthcare providers. Telehealth services, including virtual therapy sessions and telemedicine appointments, make it easier for individuals in remote or underserved areas to access the care they need.
Action Steps:
- Work with local healthcare providers and legislators to expand telehealth infrastructure.
- Provide training to community members on using telehealth platforms.
- Offer assistance programs to improve internet access and technological literacy.
2. Increase Awareness and Education
Community-based initiatives can raise awareness about dual addiction disorder, reduce stigma, and promote understanding of available treatment options. Educating the general public and healthcare providers about co-occurring disorders can improve recognition, encourage early intervention, and facilitate better management of these conditions.
Action Steps:
- Launch public awareness campaigns that address the stigma and misconceptions surrounding dual addiction.
- Organize educational events, workshops, and seminars for healthcare providers to enhance their knowledge of integrated treatment approaches.
- Incorporate stories of recovery into media efforts to provide hope and inspiration.
3. Develop Culturally Competent Services
Communities must ensure that treatment programs and support services are culturally sensitive and responsive to the needs of diverse populations. This involves providing services that account for cultural, linguistic, and social factors that may influence an individual’s experience with addiction and mental health.
Action Steps:
- Offer language interpretation services for individuals seeking treatment.
- Recruit a diverse workforce of healthcare providers who reflect the community’s cultural backgrounds.
- Integrate cultural practices into treatment plans, such as traditional healing approaches or culturally significant activities.
4. Strengthen Peer Support Networks
Peer support can be an invaluable resource for individuals struggling with dual addiction disorders. Peer-led groups, recovery centers, and mutual aid networks foster connections, offer encouragement, and provide insights from others who have lived through similar experiences.
Action Steps:
- Facilitate the development of peer-led support groups and recovery communities.
- Create spaces where individuals can share their experiences, learn from one another, and build a sense of belonging.
- Support training programs for peer recovery coaches to assist individuals throughout their recovery journey.
5. Collaborate with Local Providers
Community collaboration with local healthcare providers, including primary care clinics, mental health centers, and substance abuse treatment facilities, can help coordinate care and expand access to integrated treatment services for dual addiction disorders.
Action Steps:
- Establish partnerships with local healthcare organizations to share resources and expertise.
- Develop referral networks that connect individuals to appropriate treatment options quickly.
- Coordinate care plans that address both substance use and mental health needs simultaneously.
6. Advocate for Policy Change
Policy advocacy is vital for addressing systemic barriers that limit access to treatment. Community leaders and advocacy groups can push for changes in funding, insurance coverage, and regulations that impact the availability of mental health and addiction services.
Action Steps:
- Work with policymakers to increase funding for addiction treatment programs and mental health services.
- Advocate for expanded insurance coverage that includes integrated treatment for co-occurring disorders.
- To make evidence-based care more accessible, address regulatory barriers, such as limitations on prescribing medication-assisted treatment (MAT).
7. Address Social Determinants of Health
Substance use and mental health challenges are often linked to underlying social determinants of health, such as poverty, homelessness, unemployment, and lack of access to education. Addressing these factors can improve an individual’s overall well-being and reduce the risk of substance use.
Action Steps:
- Support housing stability initiatives, job training programs, and educational opportunities.
- Provide access to social services that help individuals meet their basic needs, such as food security and transportation assistance.
- Implement community programs that foster resilience and promote mental health.
8. Promote Collaboration and Integration
Creating a coordinated approach to treatment involves bringing together healthcare providers, social service agencies, law enforcement, schools, and other community stakeholders. This collaboration can facilitate comprehensive and integrated treatment approaches for dual addiction disorder.
Action Steps:
- Develop a community task force to coordinate efforts across different sectors.
- Share data and resources to identify service gaps and develop targeted interventions.
- Establish integrated care models that combine medical, mental health, and social services.
9. Provide Support for Families
Supporting families affected by dual addiction disorder is essential for promoting recovery and resilience. Families often play a critical role in the recovery process, and providing them with the resources and support they need can positively impact treatment outcomes.
Action Steps:
- Offer family education programs that teach coping skills, effective communication, and self-care strategies.
- Provide access to family support groups and counseling services.
- Develop respite care programs to give caregivers a break when needed.
10. Invest in Prevention and Early Intervention
Communities can invest in prevention efforts and early intervention programs to identify and address substance use and mental health issues before they escalate. Prevention programs in schools, community outreach initiatives, and screening programs in healthcare settings can catch problems early and provide timely support.
Action Steps:
- Implement school-based prevention programs that educate students about the risks of substance use.
- Conduct outreach initiatives to reach at-risk populations in the community.
- Establish routine screening for substance use and mental health conditions in healthcare settings to facilitate early intervention.
In summary, combatting barriers to treatment for dual addiction disorder requires a comprehensive and community-driven approach. By expanding telehealth services, increasing awareness, providing culturally competent care, strengthening peer support networks, and addressing social determinants of health, communities can create supportive environments that promote recovery and well-being. Collaboration among community members, organizations, and policymakers is critical to making meaningful progress in addressing this complex public health issue.
Through collective action, communities can improve access to treatment, help individuals achieve sustained recovery, and lead fulfilling lives. By embracing a holistic approach and working together, we can break down barriers to treatment and pave the way for a healthier, more resilient community.
Frequently Asked Questions
Here are some common questions:
Q: What is dual addiction disorder?
A: It is when a person has both a substance addiction and a mental health disorder at the same time.
Q: Why do dual disorders develop?
A: Many people use substances to cope with untreated mental health symptoms.
Q: Can one disorder cause the other?
A: Yes. Mental health conditions can lead to substance use, and substance use can worsen mental illness.
Q: Why is dual diagnosis treatment different?
A: Both addiction and mental health must be treated together for recovery to succeed.
Q: What treatments are used?
A: Medical detox, therapy, psychiatric care, medication, and peer recovery support.
Q: Can people recover from dual addiction disorder?
A: Absolutely. With integrated treatment and long-term support, recovery is very achievable.
Conclusion
Dual addiction disorder presents significant challenges for individuals and communities alike, requiring comprehensive treatment approaches that address both substance use and mental health issues. However, accessing such treatment in rural communities can be particularly difficult due to various barriers, including limited resources and geographical isolation. Nevertheless, communities can implement strategies to alleviate these barriers, such as expanding telehealth services, increasing awareness, and strengthening support networks. By working together to overcome these challenges, rural communities can better support individuals struggling with dual addiction disorder, fostering a path to recovery and improved well-being for all.
Video: Both Addicted AND Mentally Ill #dualdiagnosis #realstory