Permanent drug memories create strong links between drug experiences and cues, triggering cravings that often lead to relapse. These memories involve brain regions such as the dopamine system, the hippocampus, the amygdala, and the prefrontal cortex. Effective management combines self-help techniques, supportive family environments, and community resources such as therapy and peer groups to reduce triggers and strengthen recovery.
Why Drug Memories Never Fade: How the Brain Links Cues to Cravings
Have you ever wondered why some people relapse after years of sobriety, often without warning? The answer lies in how the brain forms and stores drug memories. These are powerful, long-lasting memories that link specific cues—like certain people, places, emotions, or even smells—to the pleasurable effects of drug use.
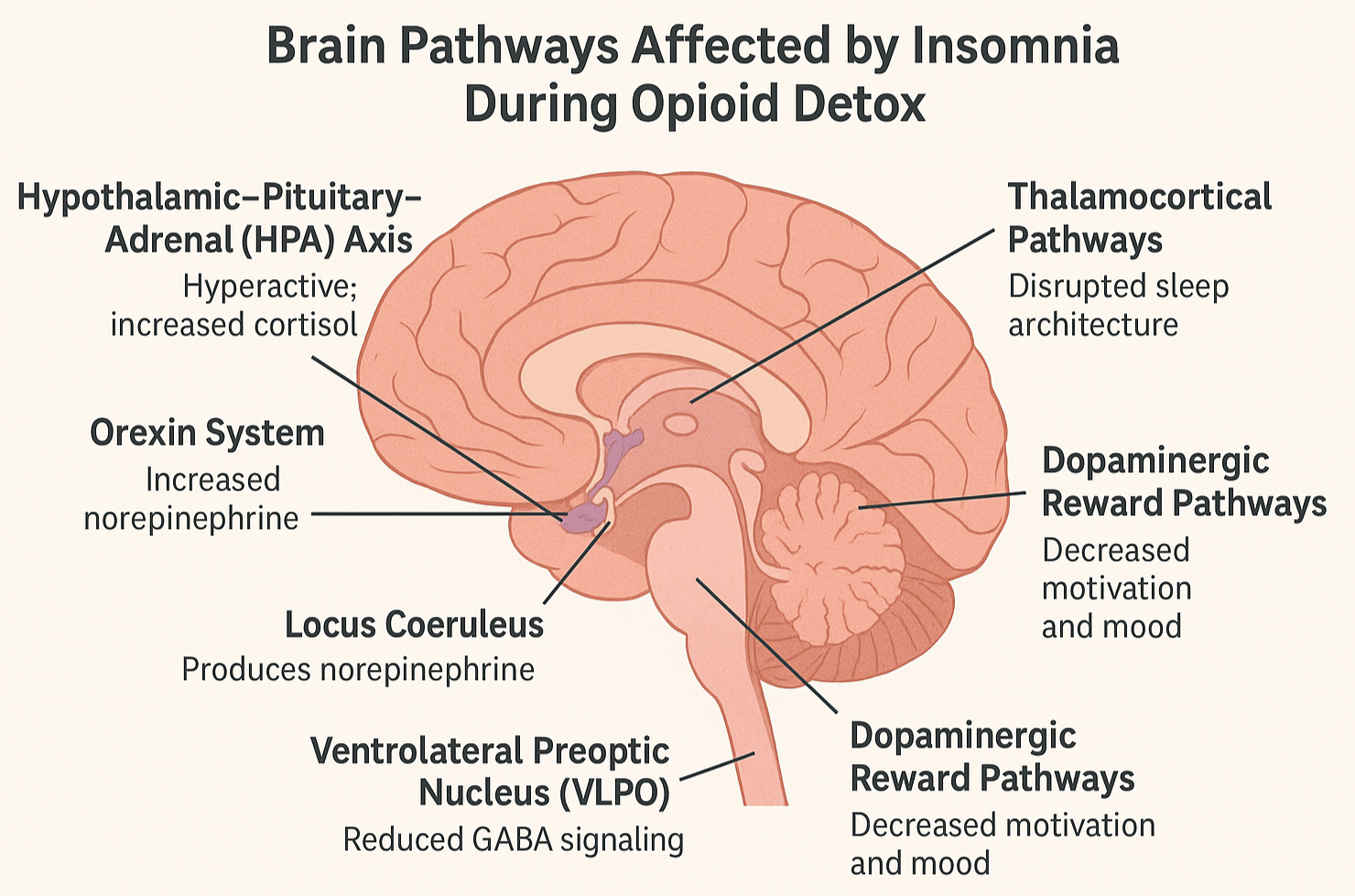
These associations are not just fleeting thoughts. They’re deeply rooted in brain regions responsible for learning, emotional response, and reward: the hippocampus, amygdala, and the mesolimbic dopamine system. Each time a person uses a substance in a specific setting or emotional state, the brain makes a mental note of everything surrounding that experience. Over time, these cues become tightly bound to the memory of the drug’s effects.
Even after long periods of abstinence, encountering one of these cues—walking past a bar, hearing a particular song, feeling stressed—can reignite intense cravings. This is because the brain essentially remembers how good the drug felt and sends signals urging the person to seek it out again. These signals can override logic, intention, and even the strongest will to stay sober.
This phenomenon explains why relapse is not just a failure of willpower—it’s a neurological response to deeply embedded memories—understanding how drug cues work is key to developing better treatments for addiction, including behavioral therapies and medications that weaken or rewire these powerful associations.
By recognizing and managing triggers, people in recovery can better protect themselves from the hidden influence of these lasting drug memories.
The Brain Remembers: How Drug Cues Trigger Cravings and Relapse
One of the most challenging aspects of addiction recovery is how easily cravings can return—even after months or years of sobriety. This isn’t just about habit or temptation. It’s about how the brain stores powerful drug-related memories that familiar cues can reactivate.
When someone uses a drug, their brain forms strong associations between the substance and surrounding elements—such as people, places, emotions, or even physical sensations. These memories are stored in key brain regions, including the hippocampus (which processes memory), the amygdala (which processes emotion), and the mesolimbic dopamine system (which drives reward and motivation).
Later, when a person encounters one of these cues—like seeing an old friend they used to work with, returning to a familiar neighborhood, or feeling a particular emotion—these brain regions light up. The memory of the drug experience resurfaces, triggering powerful cravings. This can happen even after long periods of abstinence, making relapse a constant risk.
These cue-triggered cravings are a significant reason why recovery is so complex. The brain’s learned association between the cue and the drug’s reward can override conscious decisions, support systems, and even the memory of past consequences.
Understanding this brain process helps explain why relapse is not a moral failing, but a neurological reaction to deeply ingrained memories. Treatment approaches that focus on identifying and managing triggers—such as cognitive-behavioral therapy and mindfulness—can help people retrain their responses and reduce the risk of relapse.
Recovery isn’t just about stopping drug use; it’s about rewiring the brain’s relationship with the past.
Taking Control: Self-Management Strategies to Overcome Drug Memory Triggers
One of the most persistent challenges in addiction recovery is the lasting power of drug-related memories. These memories—formed when the brain links people, places, or emotions to the rewarding effects of drug use—can trigger cravings even after long periods of sobriety. Fortunately, several self-management strategies can help reduce the impact of these memories and support long-term recovery.
1. Mindfulness and Meditation
Mindfulness teaches individuals to stay present and observe their thoughts and feelings—especially cravings—without immediately reacting. With regular practice, mindfulness can create space between a triggering memory and the decision to use, empowering individuals to choose a healthier response.
2. Cognitive Behavioral Techniques (CBT)
CBT helps individuals recognize the thought patterns and environmental triggers that bring drug memories to the surface. Through structured exercises, CBT replaces automatic drug-seeking responses with healthier coping strategies, reducing the emotional grip of those memories.
3. Avoidance of Triggers
Sometimes, the best strategy is strategic avoidance. Identifying people, places, or situations that reignite cravings can allow individuals to proactively protect their recovery by steering clear of high-risk environments.
4. Developing Healthy Routines
Daily routines that support physical and mental health—like consistent sleep, nutritious eating, regular exercise, and stress management—help regulate the brain and reduce vulnerability to cravings.
5. Journaling and Reflection
Writing down cravings, emotional reactions, and responses to triggers helps individuals make sense of their experiences. Journaling can create a pattern of self-awareness that loosens the hold drug memories may have over time.
6. Stress Reduction Techniques
Cravings often intensify during stress. Tools such as deep breathing, yoga, progressive muscle relaxation, or guided imagery can help reduce tension and interrupt the cycle in which stress leads to relapse.
Recovery is not about erasing the past but learning to live peacefully with it. By consistently using these strategies, individuals can weaken the power of drug memories and build a stronger foundation for long-term sobriety. Healing the brain takes effort, but with the right tools, lasting change is possible.
How Family Support Helps Break the Power of Drug Memories
When someone is in recovery from addiction, they’re not just battling cravings—they’re battling memories. Permanent drug memories form when the brain links certain people, places, and emotions with the highs of drug use. These memories can be reawakened by familiar cues, triggering intense cravings and risking relapse. While this process is deeply rooted in brain chemistry, family support can make a powerful difference in managing these triggers.
Here are key family strategies that help reduce the influence of drug memories and support lasting recovery:
1. Providing a Stable and Supportive Environment
A calm, safe, and consistent home environment helps reduce stress and emotional volatility. Predictability limits exposure to chaos or triggers that might bring drug memories back to the surface.
2. Encouraging Open Communication
Families who create space for honest, non-judgmental conversations about cravings, triggers, and setbacks provide emotional relief. This openness builds trust and makes the person feel less isolated in their struggle.
3. Learning About Addiction and Triggers
When families take time to understand how addiction works—especially the science of relapse triggers—they can better identify signs of struggle and respond with empathy rather than frustration.
4. Supporting Healthy Habits
Family encouragement around sleep, nutrition, physical activity, and therapy attendance strengthens routines that improve mental clarity and emotional balance—both critical in countering cravings.
5. Helping Avoid Triggers
Loved ones can support relapse prevention by helping the person avoid people, places, and activities tied to past drug use. Even small actions, like choosing new social spaces or routines, can make a big difference.
6. Providing Emotional Encouragement
Recovery is full of emotional highs and lows. Regular, sincere encouragement from family can boost self-worth and strengthen the person’s motivation to stay on track, even when drug memories surface.
Recovery doesn’t happen in isolation. When families actively participate and offer consistent support, they become a protective buffer against the powerful pull of drug memories. Together, healing becomes not just possible—but sustainable.
Harnessing Community Power: Strategies to Manage Drug Memory Triggers and Prevent Relapse
Addiction recovery is not a journey that should be taken alone—especially when battling the lasting impact of permanent drug memories. These powerful memories, encoded in the brain, can be reactivated by everyday triggers, leading to intense cravings and increasing the risk of relapse. Fortunately, community resources offer essential tools and support systems to help individuals manage these challenges and stay on the path to recovery.
Here are key community-based strategies that play a critical role in managing drug memory triggers:
1. Support Groups
Peer support is one of the most effective ways to combat cravings. Groups like Narcotics Anonymous (NA) or SMART Recovery offer safe spaces for individuals to share struggles and solutions. Listening to others’ experiences can normalize cravings, reduce shame, and reinforce the motivation to resist relapse.
2. Counseling and Therapy Services
Access to professional therapy—primarily Cognitive Behavioral Therapy (CBT) and trauma-informed care—helps individuals unpack the root causes of addiction. Therapy teaches practical skills to manage emotional triggers and weaken the grip of drug-related memories.
3. Relapse Prevention Programs
Many community organizations offer structured programs that teach individuals how to recognize, anticipate, and cope with cues that might lead to relapse. These programs often include role-playing scenarios, personalized action plans, and emotional regulation techniques.
4. Sober Living Environments
Transitional housing or sober living homes provide drug-free environments where residents support one another in maintaining recovery. These settings reduce exposure to drug-related triggers and encourage the development of healthy routines and accountability.
5. Educational Workshops
Knowledge is power. Workshops that explain how addiction affects the brain, how cravings work, and how to respond to triggers help individuals and families become more confident in managing relapse risks.
6. Access to Health and Social Services
Unstable housing, unemployment, or untreated health conditions can heighten stress and increase vulnerability to drug memory triggers. Community programs that offer assistance with housing, employment, medical care, and transportation provide vital stability that supports recovery.
By engaging with these community resources, individuals build a strong network of support that enhances their resilience against the pull of drug memories. Recovery becomes more sustainable when individuals are empowered, supported, and connected—not just to services, but to people who care.
Frequently Asked Questions
Here are some common questions:
Question: Provide a self-management toolkit to help manage drug memories.
Answer: A Self-Management Toolkit to Help Manage Drug Memories and Prevent Relapse should include practical tools, techniques, and supportive resources that empower individuals in recovery to understand, cope with, and reduce the influence of drug-related cues. Below is a comprehensive, user-friendly toolkit broken down into core components:
🧠 1. Mental & Emotional Tools
These help manage cravings and the emotional distress triggered by drug memories.
- Mindfulness Exercises
- Guided meditation apps (e.g., Headspace, Insight Timer)
- “Urge Surfing” technique to ride out cravings
- 5-4-3-2-1 grounding exercise
- Cognitive Behavioral Worksheets
- Identify thought → feeling → behavior patterns
- Reframe distorted beliefs (“I can’t cope without using”)
- Challenge triggers and create alternative responses
- Daily Journal Prompts
- “What triggered me today?”
- “How did I respond to cravings?”
- “What can I do differently tomorrow?”
📅 2. Routine & Structure Tools
Consistency helps regulate brain function and reduces emotional volatility.
- Recovery Planner (daily/weekly)
- Schedule for meals, sleep, exercise, meetings, and therapy
- Highlight high-risk times/places to avoid
- Set goals and self-rewards
- Habit Trackers
- Track sleep, hydration, physical activity, and stress levels
- Celebrate consistency (e.g., “10 days of exercise = reward”)
📵 3. Trigger Management Tools
Help avoid or neutralize cues that can activate drug memories.
- Trigger Log Template
- Track specific triggers and your emotional/behavioral response
- Rate the intensity of the craving (0–10 scale)
- Record how you coped (effective or not?)
- Crisis Plan Card
- “If I experience a craving, I will…”
- List three coping techniques, three people to call, and one place to go
- Keep it in your wallet or phone
- Environment Checklist
- Audit your home, phone, social media, and social circles
- Remove or reduce cues linked to past drug use
📞 4. Support & Connection Tools
Social support reduces isolation and increases accountability.
- Support Contact Sheet
- List of trusted friends, sponsor, therapist, support group times
- Crisis helpline numbers (SAMHSA: 1-800-662-HELP)
- “Who can I talk to before I act on a craving?”
- Digital Support Access
- Recovery apps (e.g., SoberTool, I Am Sober, WEconnect)
- Online meeting platforms (NA, SMART Recovery, Reddit groups)
- Affirmation & Encouragement Cards
- “This craving will pass.”
- “My past does not define my future.”
- Personalized cards for quick motivation
🛠️ 5. Stress & Emotion Regulation Tools
Reduce stress to lower the intensity of drug memory triggers.
- Quick Calm Kit
- Deep breathing guide
- Fidget toy, grounding stone, essential oil
- List of calming activities (walk, hot shower, call someone)
- Coping Skills Menu
- 10 healthy alternatives to using (art, journaling, music, stretching)
- Emergency distraction list (games, movies, cleaning tasks)
📘 Optional: Printable Toolkit Binder (or Digital Folder)
Organize all of the above into a personal recovery binder or a digital folder:
Add personalized notes, progress charts, and inspirational quotes
Section dividers for triggers, coping tools, journaling, and goals
Include printed guides or templates
Question: Provide a family support strategies toolkit to help an addict manage drug memories.
Answer: A Family Support Strategies Toolkit designed to help a loved one manage drug memories that can trigger cravings and relapse. This toolkit equips families with practical tools, communication techniques, and emotional support strategies to build a healthy, healing environment around the person in recovery.
🧰 Family Support Toolkit for Managing Drug Memories
🔑 1. Education & Awareness Tools
Purpose: Help family members understand how drug memories work and what relapse triggers look like.
- Quick Guide: How Drug Memories Affect the Brain
- 1-page handout explaining the role of cues and brain pathways (hippocampus, amygdala, dopamine system).
- Include common triggers: people, places, emotions, smells, music.
- Relapse Warning Sign Checklist
- Mood shifts (irritability, depression)
- Avoidance or secrecy
- Reconnecting with old friends or environments
- Recommended Reading/Resources:
- “Beyond Addiction” (FoR Families of People with Addiction)
- SAMHSA Family Support Tools
- NIDA family resource links
💬 2. Healthy Communication Tools
Purpose: Improve trust, openness, and reduce shame or defensiveness when discussing cravings or setbacks.
- Weekly Check-In Prompts
- “How are you managing your triggers this week?”
- “What can I do that feels supportive—not controlling?”
- “Are there any routines or environments that feel unsafe?”
- Do’s and Don’ts of Supporting Recovery
- ✅ Listen without judgment
- ✅ Use “I” statements (“I feel concerned when…”)
- ❌ Don’t accuse, blame, or shame
- ❌ Don’t try to control their recovery
- Conflict De-escalation Script
- “I’m noticing you seem overwhelmed. Would now be a good time to talk or take a break?”
- “I want to support you. Let’s figure this out together.”
🏠 3. Home Environment Support Tools
Purpose: Create a calm, safe, and trigger-free environment that supports healing.
- Trigger-Free Home Checklist
- Remove drug paraphernalia, alcohol, and triggering media
- Avoid conversations that romanticize past drug use
- Introduce soothing items: calming scents, music, and low lighting
- Healthy Routine Chart
- Daily/weekly planner with meals, exercise, recovery meetings, and family activities
- Include goal-setting and shared self-care routines
- “Safe Space” Agreements
- Establish one room or time of day as a “no-pressure zone.”
- No tough conversations unless both parties agree
❤️ 4. Emotional Support Tools
Purpose: Build emotional resilience in both the individual in recovery and the family.
- Encouragement Card Deck (Can be DIY or printable)
- “This craving will pass.”
- “You’re not alone—I’m here with you.”
- “Progress, not perfection.”
- Leave notes in lunch bags, on mirrors, or in journals.
- Gratitude Journal (Shared or Individual)
- Record small wins and shared moments of connection
- Focus on progress, not relapse
- Boundaries & Self-Care Plan (for family)
- Define healthy limits (e.g., “I will not support behavior that endangers your recovery”)
- Include personal support routines, therapy, or support groups for family (Al-Anon, NAMI, etc.)
🤝 5. Community & Support Resources
Purpose: Connect the family to external support and tools for ongoing growth.
- Support Group Directory
- Al-Anon, Nar-Anon, SMART Recovery Family & Friends
- Local family addiction support groups, church ministries, or wellness centers
- Emergency & Crisis Card
- Contacts for sponsor, therapist, local crisis line, SAMHSA (1-800-662-HELP)
- Steps to take if relapse occurs (without panic)
- Local Resource Map
- Highlight nearby therapists, sober events, family education programs, job or housing support
🗂️ Bonus: Printable or Digital Toolkit Binder
Organize these tools into a Family Recovery Binder or Google Drive/Notion folder:
Include shared progress tracker (e.g., days in recovery, therapy attended, family check-ins)
Tabs for: education, communication tools, home environment, journaling, resources
Question: Provide a community resource toolkit to help addicts manage drug memories.
Answer: A comprehensive Community Resource Toolkit designed to help individuals in recovery manage drug memories that can trigger cravings and relapse. This toolkit is built around the idea that healing requires connection, structure, and support, all of which can be provided through accessible community resources.
🧰 Community Resource Toolkit to Help Manage Drug Memories
🔗 1. Peer Support Networks
Purpose: Provide ongoing connection, shared experiences, and accountability.
- Local & Online Support Groups
- Narcotics Anonymous (NA), SMART Recovery, Celebrate Recovery, LifeRing
- Find local meetings: na.org/meetingsearch, smartrecovery.org
- Mobile apps: SoberTool, I Am Sober, WEconnect
- Peer Mentorship Programs
- State or county-run peer specialist programs
- Local recovery community organizations (RCOs)
- Community Recovery Cafés & Drop-in Centers
- Safe spaces for connection, journaling, job prep, group therapy, or creative expression
- Offer a daily structure and peer bonding away from triggers
🧠 2. Counseling & Clinical Services
Purpose: Address trauma, reshape drug-related thought patterns, and build mental health support.
- Free/Low-Cost Therapy Access
- Federally Qualified Health Centers (FQHCs) offering sliding-scale care
- County behavioral health departments
- Cognitive Behavioral Therapy (CBT) & Trauma-Informed Therapy
- Clinics providing evidence-based treatments for addiction-related brain memories
- Look for providers certified in DBT, EMDR, or trauma-focused CBT
- Co-Occurring Disorder Treatment Programs
- For individuals with addiction and mental health needs
- Coordinate support for anxiety, PTSD, or depression, which may intensify cravings
🧭 3. Relapse Prevention & Education Resources
Purpose: Help individuals learn about triggers, develop coping strategies, and understand addiction science.
- Relapse Prevention Workshops
- Local treatment centers or nonprofits offering skill-building sessions
- Topics: managing drug memories, healthy relationships, mindfulness, trigger mapping
- Educational Materials
- Printable handouts on brain pathways of addiction
- Craving management worksheets, urge tracking logs, and recovery calendars
- Recovery Toolkits from National Organizations
- SAMHSA, Shatterproof, Faces & Voices of Recovery, Partnership to End Addiction
🏡 4. Sober Housing & Living Support
Purpose: Provide stable, substance-free environments that reduce trigger exposure.
- Certified Sober Living Homes (SLHs)
- Structured living spaces that promote accountability and community
- Often linked to recovery coaches and support services
- Housing Assistance Programs
- Local housing authorities or nonprofit reentry programs
- Transitional housing with wraparound case management
- Safe Space Locator Map
- Create or provide maps of libraries, community centers, sober cafes, or outdoor areas that can serve as coping-friendly alternatives when memories hit
💼 5. Life Stability & Social Support
Purpose: Reduce life stressors that make individuals more vulnerable to cravings and drug memories.
- Job Training & Employment Resources
- Programs like Goodwill, America Works, or workforce centers
- Second-chance employment programs for those with criminal records
- Healthcare Navigation
- Local clinics offering MAT (Medication-Assisted Treatment) and therapy
- Enrollment help for Medicaid, ACA insurance, or mental health services
- Transportation Assistance
- Transit vouchers, ride-share programs for recovery meetings or appointments
- Food & Clothing Resources
- Food pantries, thrift stores, clothing banks
- Reduces survival stress that often reactivates craving pathways
📘 6. Community Education & Advocacy
Purpose: Help individuals feel empowered and understood while reducing stigma.
- Public Workshops & Events
- Community-based sessions on addiction science, family recovery, and relapse prevention
- Peer storytelling events and recovery fairs
- Stigma Reduction Campaigns
- Participate in or distribute materials from Recovery Month, Shatterproof Stigma Campaign, or local health departments
- Volunteer & Advocacy Opportunities
- Engage in community action (cleanups, speaking, mentoring)
- Builds identity beyond addiction and reframes past drug memories as sources of growth
🗂️ Bonus: Create a Personalized Community Recovery Binder or Digital Toolkit
Include:
Motivational quotes or art
Local meeting schedules
Provider directories (housing, therapy, medical, legal aid)
Emergency contacts
Personal relapse plan + trigger logs
Sober day tracker
Conclusion
Permanent drug memories encoded in key brain pathways play a decisive role in triggering relapse by linking drug cues to intense cravings. Successfully managing these memories requires a combined effort of self-management skills, strong family support, and accessible community resources. By addressing both the neurological and social aspects of addiction, individuals are better equipped to resist triggers and maintain long-term recovery.
Video: Why Drug Memories Are So HARD to Forget