Addictive drugs alter the brain’s reward system, leading to compulsive use, tolerance, and withdrawal. In contrast, antidepressants don’t cause euphoria or cravings but may lead to physical dependence, requiring gradual tapering to avoid withdrawal. However, antidepressants are not considered addictive.
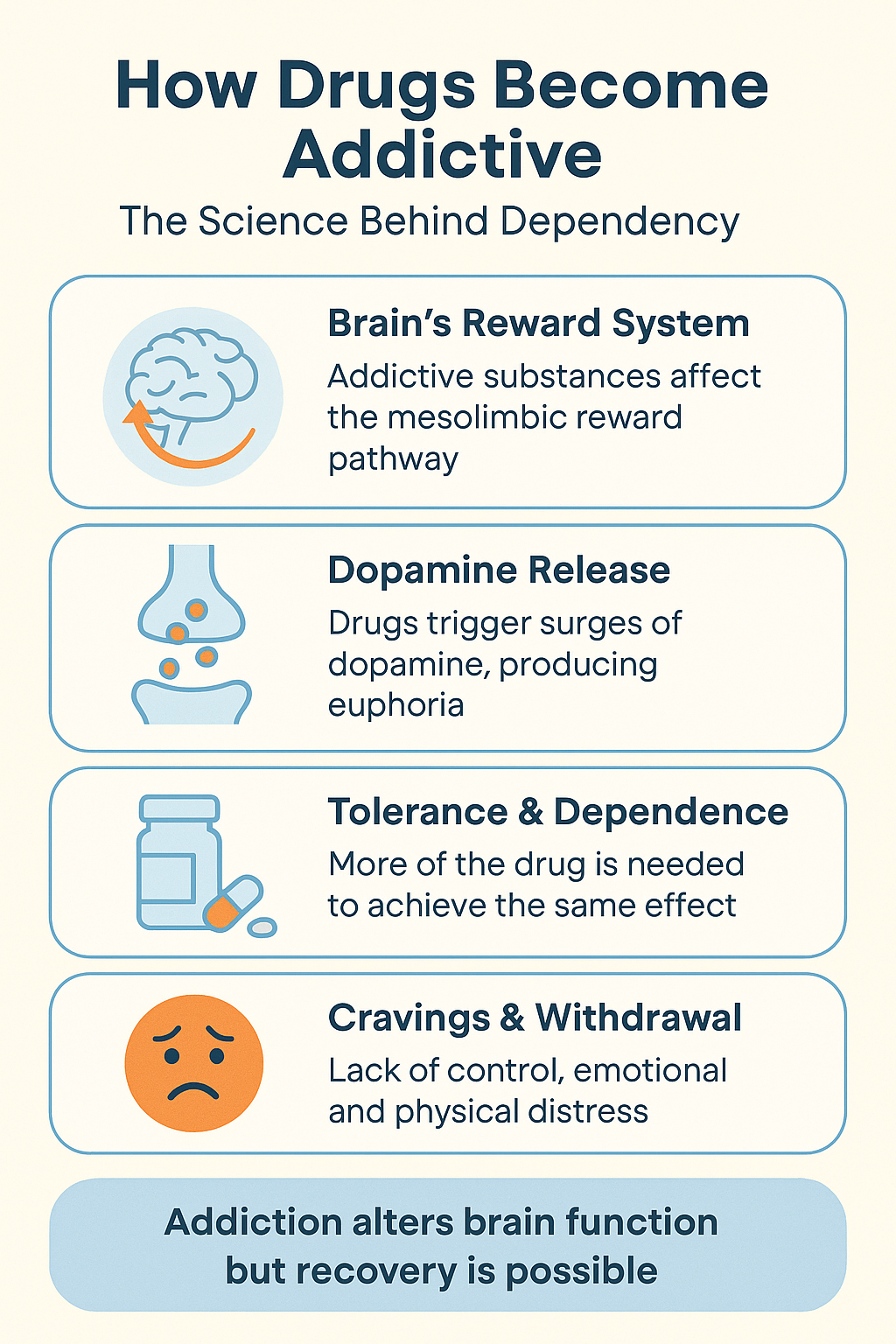
How Drugs Become Addictive: The Science Behind Dependency
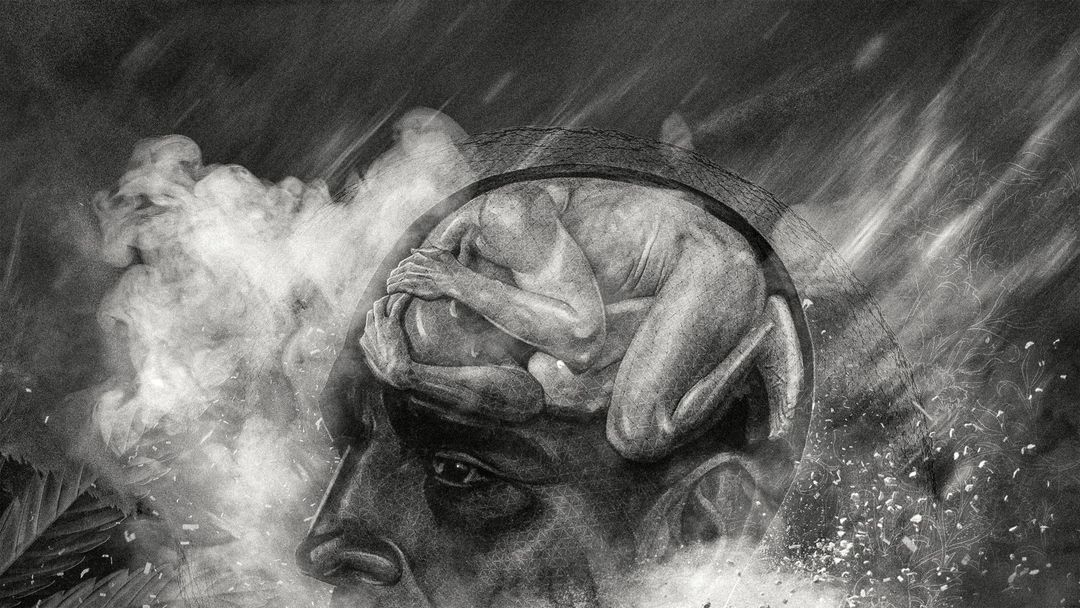
Addiction is a complex condition that develops when a drug alters the brain’s reward system, particularly the dopamine pathways, reinforcing a cycle of repeated use. While many factors contribute to addiction, the key mechanisms involve biological, psychological, and environmental influences that make quitting difficult.
1. Dopamine Release: The Pleasure Trap
Drugs like alcohol, nicotine, and opioids flood the brain with dopamine, the neurotransmitter responsible for pleasure and reinforcement. This surge creates an influential association between drug use and reward, making the user crave repeated experiences.
2. Tolerance: The Need for More
With continuous use, the brain becomes less sensitive to the drug’s effects, requiring larger doses to achieve the same high. This phenomenon, known as tolerance, encourages users to increase their consumption, deepening their dependence.
3. Dependence: The Body’s Reliance on the Drug
Over time, the brain and body adapt to the drug, leading to dependence. If the drug is stopped, withdrawal symptoms—such as anxiety, nausea, or tremors—occur. To avoid discomfort, individuals feel compelled to keep using, further reinforcing the addiction cycle.
4. Psychological Triggers: Emotional and Environmental Cues
Drugs can become a way to cope with stress, trauma, or social situations. Stimulants like cocaine or methamphetamine provide confidence and energy, making them psychologically addictive. Even after physical withdrawal fades, emotional cravings can persist, making relapse likely.
5. Genetic Influence: A Predisposition to Addiction
Genetics plays a role in addiction vulnerability. Variations in dopamine receptors and reward processing can make some individuals more prone to developing substance use disorders, increasing their risk of dependency.
6. Brain Changes: Altered Decision-Making and Control
Long-term drug use rewires brain circuits involved in self-control, decision-making, and reward. These changes make quitting extremely difficult, as the brain increasingly prioritizes drug-seeking behavior over rational choices.
7. Social and Environmental Factors: External Triggers
Stress, peer pressure, and exposure to drug use in social circles or family settings can contribute to addiction. Individuals in environments where substance use is normalized may be more likely to develop dependency.
In summary, addiction develops when a drug hijacks the brain’s reward system, leading to tolerance, dependence, and lasting neurological changes. While biological and psychological factors play a significant role, environmental influences further reinforce drug-seeking behavior. Understanding these mechanisms can help in prevention, treatment, and recovery efforts, highlighting the importance of both medical and psychological support in overcoming addiction.
Recognizing the Physical Signs of Drug Dependence
Physical dependence on a drug develops when the body adapts to its presence and requires it to function normally. When a person dependent on a substance reduces or stops usage, they may experience withdrawal symptoms that range from mild discomfort to severe health risks. Understanding these physical signs is crucial in recognizing dependence and seeking help before it progresses into full-blown addiction.
1. Tolerance: The Body’s Adaptation
One of the earliest signs of dependence is tolerance—when the body becomes accustomed to the drug, requiring higher doses to achieve the same effects. This gradual escalation increases the risk of further dependence.
2. Withdrawal Symptoms: The Body’s Reaction to Absence
Stopping or reducing drug use can trigger withdrawal symptoms, which vary by substance but commonly include:
- Physical symptoms: Sweating, chills, tremors, nausea, vomiting, headaches, muscle pain, fatigue, dizziness, and rapid heartbeat.
- Psychological symptoms: Anxiety, depression, irritability, difficulty concentrating, and intense cravings.
3. Loss of Control Over Drug Use
Individuals may struggle to quit or cut back, not because of a lack of willpower, but due to the discomfort of withdrawal symptoms. The fear of withdrawal can drive continued use.
4. Drug-Seeking Behavior
A person dependent on a drug may go to great lengths to maintain access to it—doctor shopping, forging prescriptions, or obtaining the substance illegally—to avoid withdrawal effects.
5. Continued Use Despite Harm
Even when drug use leads to negative consequences—such as health problems, relationship strain, or trouble at work—an individual may continue using it to prevent withdrawal discomfort.
6. Cravings and Urges
Physical dependence creates strong urges to use the drug, as the body has come to rely on it to maintain normal function. Cravings can become overwhelming, leading to compulsive use.
7. Disruptions in Sleep and Appetite
Many dependent individuals experience changes in their sleep patterns, such as insomnia or excessive drowsiness, as well as fluctuations in appetite, ranging from extreme hunger to complete loss of interest in food.
8. Visible Physical Effects
Signs such as bloodshot eyes, slurred speech, poor coordination, or a noticeable decline in physical health can indicate dependence. Long-term use may lead to more severe health complications.
9. Increasing Dosage Over Time
As tolerance builds, individuals may escalate their drug use, taking larger doses to achieve the same effect. This pattern can reinforce dependence and make withdrawal symptoms even more severe.
Common Drugs That Cause Physical Dependence
Several substances are known for causing dependence, including:
- Opioids (morphine, heroin, prescription painkillers)
- Alcohol
- Benzodiazepines (Xanax, Valium)
- Nicotine
- Stimulants (cocaine, methamphetamine)
- Antidepressants (in some cases, if stopped abruptly)
Physical dependence develops when the body adapts to a drug, leading to withdrawal symptoms and increased tolerance. Recognizing these warning signs early can help individuals seek appropriate treatment before dependence turns into full addiction. Understanding the risks and seeking medical guidance can be essential steps toward recovery.
Antidepressants vs. Addictive Drugs: Understanding the Key Differences
While both antidepressants and addictive drugs influence brain chemistry, they serve distinct purposes and have vastly different effects on behavior, dependency, and long-term health. Understanding these differences is essential for recognizing the role of antidepressants in mental health treatment and the dangers of addictive substances.
1. Purpose and Use
- Antidepressants: Prescribed to treat mental health conditions like depression and anxiety by regulating neurotransmitters over time.
- Addictive Drugs: Often used recreationally for immediate pleasure or stress relief, but can lead to compulsive use and addiction.
2. How They Affect the Brain
- Antidepressants: Gradually balance brain chemicals (e.g., serotonin) to improve mood and emotional stability.
- Addictive Drugs: Stimulate dopamine release, creating a powerful sense of euphoria that reinforces repeated use.
3. Risk of Addiction
- Antidepressants: Do not produce cravings or compulsive use, though sudden discontinuation can cause withdrawal-like symptoms.
- Addictive Drugs: Lead to physical and psychological dependence, with users often experiencing intense cravings and loss of control.
4. Withdrawal Symptoms
- Antidepressants: Discontinuation syndrome can cause temporary discomfort but is not life-threatening.
- Addictive Drugs: Withdrawal can be severe, including physical pain, seizures, and dangerous health risks.
5. Behavioral Impact
- Antidepressants: Help stabilize emotions and improve daily functioning.
- Addictive Drugs: Can lead to erratic, compulsive, or destructive behaviors due to the brain’s focus on the substance.
6. Long-Term Consequences
- Antidepressants: Generally safe for long-term use under medical supervision, though side effects may occur.
- Addictive Drugs: Long-term use can cause irreversible brain damage, organ failure, and severe life consequences.
7. Treatment Approaches
- Antidepressants: Often used alongside therapy to manage mental health conditions.
- Addictive Drugs: Require detox, rehabilitation, therapy, and support groups to overcome addiction.
Antidepressants and addictive drugs differ fundamentally in their purpose, effects, and risks. While antidepressants aid in mental health management without causing addiction, addictive drugs create a cycle of compulsive use and dependence. Understanding these differences can help individuals make informed decisions about medication use and substance-related risks.
Can Antidepressants Be Addictive? Understanding the Difference Between Dependence and Addiction
Antidepressants are commonly prescribed to treat depression and anxiety, but many people wonder whether they can be addictive. While they do not produce the same cravings or compulsive use as addictive substances like opioids or alcohol, they can lead to physical dependence in some cases. Here’s what you need to know:
1. No Euphoria or Immediate Reward
Unlike addictive drugs, antidepressants do not create a euphoric high or an instant sense of pleasure. Instead, they work gradually by balancing neurotransmitters like serotonin to improve mood over time.
2. Dependence vs. Addiction
- Dependence: Long-term use of antidepressants can lead to physical dependence, meaning the body adapts to the drug. Suddenly stopping can cause withdrawal-like symptoms, known as discontinuation syndrome (e.g., dizziness, mood swings, fatigue).
- Addiction: True addiction involves cravings, compulsive drug-seeking behavior, and continued use despite negative consequences. Antidepressants do not trigger these behaviors.
3. The Importance of Gradual Withdrawal
Stopping antidepressants suddenly can lead to uncomfortable withdrawal symptoms. To avoid this, healthcare providers recommend tapering off the medication slowly to allow the brain to adjust.
4. Misuse Potential
While rare, some individuals may misuse antidepressants by taking higher doses in hopes of faster results. However, this is not the same as addiction, as these medications do not create a high or reinforcement cycle.
5. Long-Term Use and Safety
For many individuals with chronic depression or anxiety, long-term use of antidepressants is necessary. When taken as prescribed, they are safe and effective without leading to addiction.
Antidepressants are not addictive in the traditional sense, as they do not cause cravings or compulsive drug-seeking behavior. However, they can lead to physical dependence, making gradual discontinuation important. If considering stopping antidepressants, it’s best to consult a healthcare provider to minimize withdrawal effects.
Frequently Asked Questions
Here are some common questions:
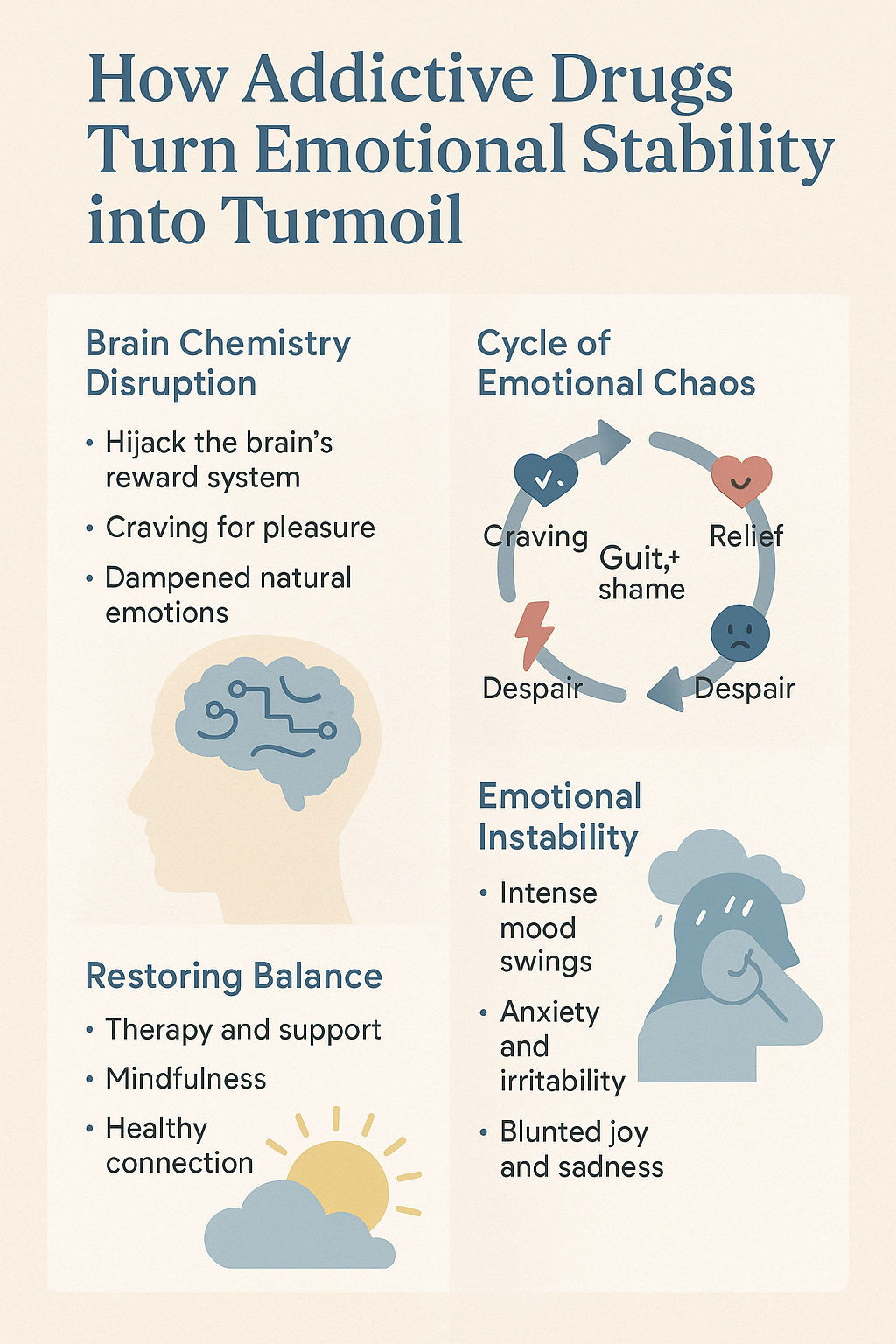
Question: How do the additive properties of the drug turn the emotional state of an addict into turmoil?
Answer: The addictive properties of a drug can severely disrupt an addict’s emotional state, leading to turmoil in several ways. Initially, drugs trigger intense feelings of euphoria or relief by altering the brain’s reward system, particularly by increasing dopamine levels. This creates a “high” that the brain associates with pleasure and relief. However, over time, as the body adapts, tolerance develops, meaning the person needs higher doses to achieve the same effect. This escalating need for the drug can create a sense of emotional instability and dependence.
When the drug’s effects wear off, the emotional state can shift drastically, causing feelings of irritability, anxiety, depression, or emptiness. This is compounded by withdrawal symptoms when the person is unable to access the drug, leading to intense physical and psychological discomfort. The fear of withdrawal can prompt the individual to prioritize the drug above all else, resulting in a constant cycle of seeking relief from emotional distress through the drug, even as it worsens the underlying turmoil. As the addiction deepens, the addict’s emotional world becomes dominated by cravings, guilt, shame, anxiety, and despair, leading to a cycle of turmoil that is hard to break. The inability to regulate emotions without the drug often leaves the addict feeling trapped in a constant state of emotional chaos.
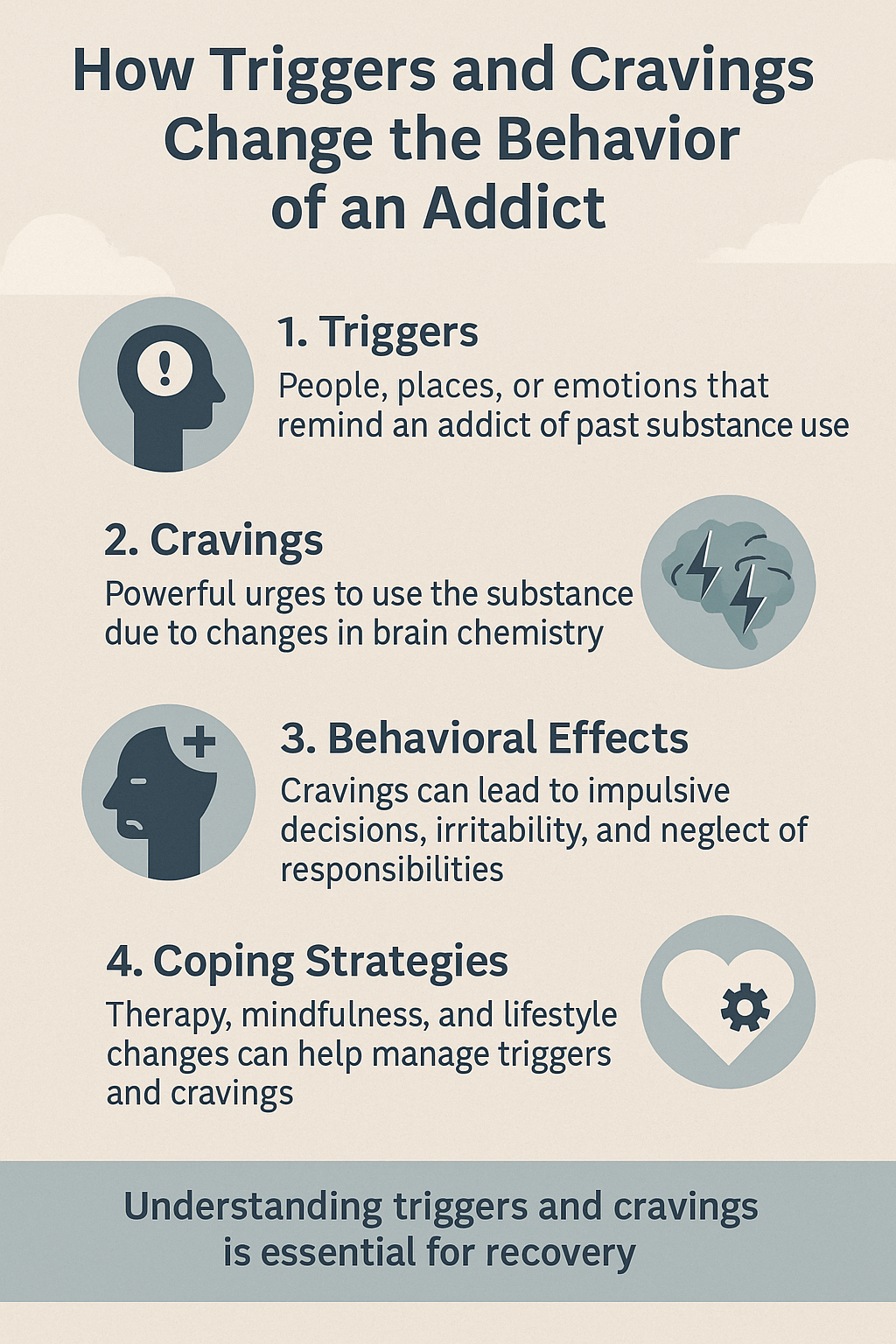
Question: How do the triggers or cravings of the drug change the addict’s behavior?
Answer: Triggers and cravings play a central role in changing an addict’s behavior, often leading them to act in ways that prioritize obtaining and using the drug. These cravings and triggers are robust psychological and physiological responses that reinforce the cycle of addiction.
1. Increased Urges and Compulsive Behavior
- Cravings are intense urges to use the drug, often triggered by external cues (such as people, places, or situations) or internal emotions (such as stress, anxiety, or depression). These cravings hijack the brain’s reward system, leading the individual to seek out the drug to alleviate discomfort or to experience the temporary relief or euphoria it provides.
- This leads to compulsive behavior, where the addict may repeatedly engage in drug-seeking actions, even if they are aware of the negative consequences (e.g., lying, stealing, or neglecting responsibilities).
2. Altered Decision-Making and Prioritization
- When cravings hit, the addict’s decision-making abilities are impaired. The brain’s reward system becomes hyper-focused on the drug, often overriding logical thinking, future planning, or consideration of consequences.
- As a result, the addict might prioritize drug use over relationships, work, or health, leading to neglect of daily responsibilities and social isolation. This can strain relationships with family and friends and impair their ability to function effectively in everyday life.
3. Reinforced Habitual Actions
- The brain’s reward system reinforces the link between specific cues and drug use. For example, a particular location, time of day, or emotional state might trigger an intense craving, causing the individual to repeat the same actions that lead to drug consumption.
- Over time, these behaviors become habitual and automatic, making it even harder for the addict to break free from the cycle. The addict’s brain learns to associate these triggers with relief or pleasure, further cementing the addiction.
4. Increased Tolerance and Escalation of Use
- As cravings intensify, the addict may escalate their drug use to achieve the same effect due to the development of tolerance. The desire to avoid withdrawal or enhance the euphoria associated with drug use drives this increase in consumption, reinforcing destructive patterns of behavior.
5. Emotional and Psychological Effects
- When cravings go unmet, the addict may experience intense emotional distress, including anxiety, irritability, anger, or depression. This emotional discomfort often leads to even greater urgency in seeking out the drug, creating a vicious cycle of craving, using, and emotional instability.
In summary, cravings and triggers cause an addict to act in ways that prioritize obtaining and using the drug, often leading to reckless, compulsive, and self-destructive behaviors. These cravings create a feedback loop, reinforcing the addiction and significantly disrupting the addict’s ability to make rational decisions and maintain a balanced emotional state.
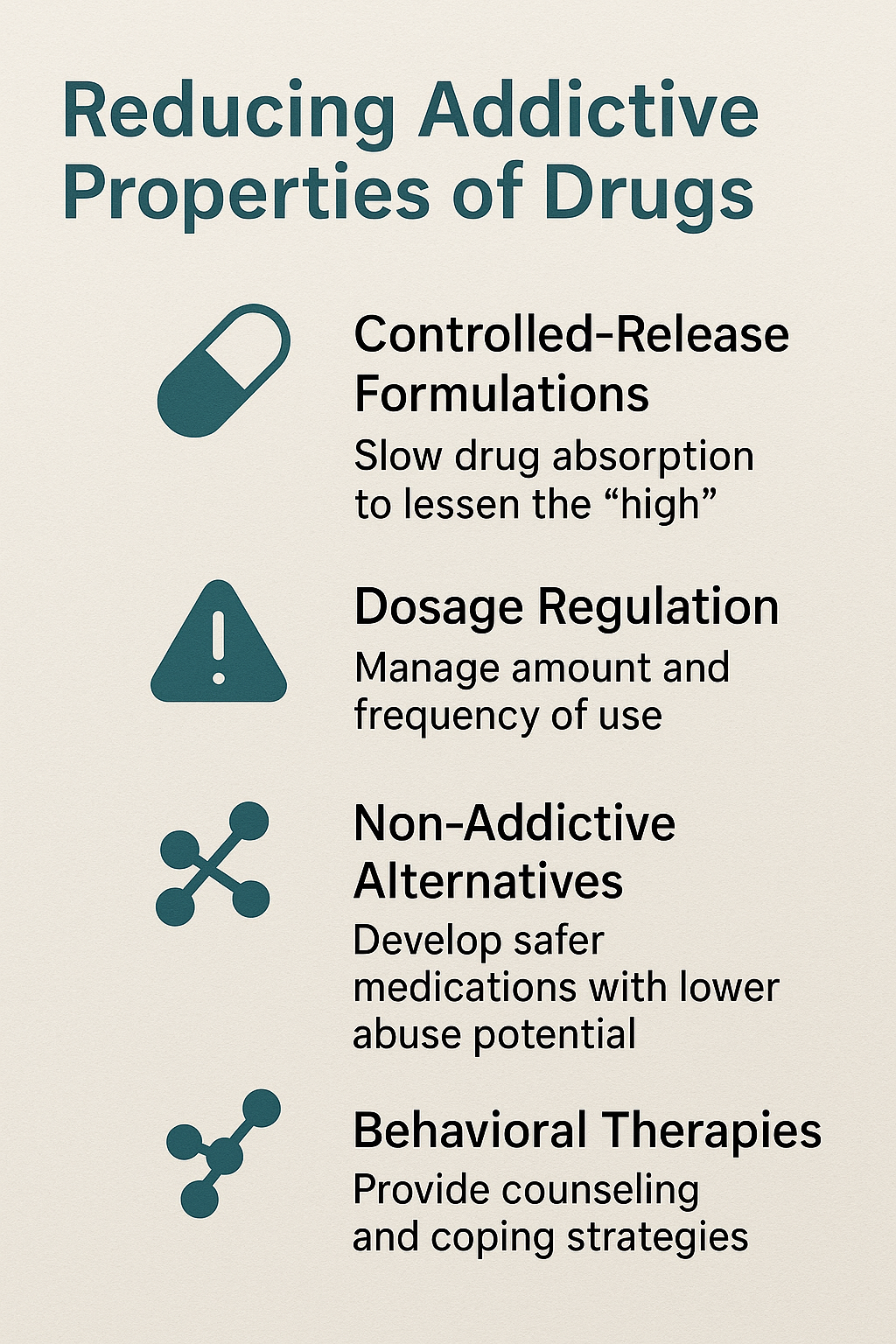
Question: How can the addictive properties of a drug be reduced to avoid dependency?
Answer: Reducing the addictive properties of a drug to prevent dependency involves several strategies, both at the level of drug development and in the way drugs are used and prescribed. Here are some key approaches to minimizing the risk of addiction:
1. Developing Less Addictive Formulations
- Alter Drug Design: Pharmaceutical companies can design drugs that are less likely to induce euphoria or reinforce the brain’s reward system. For example, certain medications can be formulated to have slow-release mechanisms, which reduce the intensity of the drug’s effects and make it less likely to cause a “rush” or intense high.
- Abuse-Deterrent Formulations: Some drugs, especially opioids, can be made with abuse-deterrent properties, such as designs that prevent them from being easily crushed, snorted, or injected. This helps reduce the potential for misuse.
2. Non-Addictive Alternatives
- Switch to Non-Addictive Medications: When possible, doctors can prescribe non-addictive alternatives for managing pain, anxiety, or other conditions. For example, some non-opioid pain relievers or non-benzodiazepine anti-anxiety medications can be used to avoid the risk of addiction associated with specific drug classes.
- Behavioral Therapies: For mental health conditions, combining medications with behavioral therapies (e.g., cognitive-behavioral therapy) can provide patients with coping strategies and reduce the reliance on drugs that may have addictive properties.
3. Proper Prescription and Monitoring
- Use of Medications Only as Prescribed: Limiting prescription duration and ensuring they are taken only as directed can significantly reduce the likelihood of dependence. For example, opioid prescriptions should be kept to the minimum effective dose and for the shortest duration necessary.
- Close Monitoring: Regular check-ins and follow-up appointments allow healthcare providers to monitor for signs of misuse or dependence, ensuring that any early signs of addiction are addressed before they escalate.
4. Tapering and Gradual Reduction
- Gradual Tapering: For drugs that have the potential for dependence (e.g., antidepressants, opioids, benzodiazepines), it’s essential to reduce the dosage rather than stopping abruptly, slowly. This helps the body adjust and prevents withdrawal symptoms, which can drive the desire for continued use.
- Psychiatric Support: For individuals who have been prescribed addictive medications, providing mental health support through therapy can help manage the emotional and psychological triggers that contribute to dependence.
5. Education and Awareness
- Patient Education: Educating patients about the risks of dependence and the importance of following their treatment plans can help them avoid misuse. Awareness of potential side effects and withdrawal symptoms can encourage adherence to the prescribed regimen.
- Public Awareness Campaigns: Widespread campaigns that inform people about the dangers of misuse and addiction can prevent recreational drug use and highlight safer alternatives.
6. Alternative Therapies
- Complementary Therapies: For certain conditions, alternative therapies such as acupuncture, physical therapy, mindfulness, or meditation can offer non-drug-based relief. These can be used alongside or as a substitute for medications that have addictive properties.
- Lifestyle Changes: Encouraging healthier lifestyle changes, such as exercise, proper nutrition, and stress management, can help individuals manage chronic pain, anxiety, or other conditions without relying on potentially addictive substances.
7. Research and Development of Addiction-Resistant Drugs
- Ongoing Research: Continuous research into the neurobiology of addiction and drug development aims to create medications that provide the therapeutic benefits without the addictive risks. For example, partial agonists (such as buprenorphine for opioid use disorder) can activate the same receptors as addictive substances but in a way that reduces the potential for misuse.
To reduce the addictive properties of drugs and prevent dependency, a multifaceted approach is necessary. This includes the development of safer medications, proper prescription and monitoring practices, education, and the use of non-addictive alternatives. By combining these strategies, the risks of addiction can be minimized, helping individuals receive the treatment they need without the danger of developing dependency.
Conclusion
Understanding a drug’s addictive properties is crucial in distinguishing between addiction and dependence. Addictive drugs create euphoria, reinforcing compulsive use, tolerance, and withdrawal. Dependence, marked by withdrawal symptoms, can occur with both addictive substances and antidepressants, though the latter do not cause cravings or compulsive behavior. While antidepressants may require gradual discontinuation to prevent withdrawal symptoms, they lack the reinforcing properties that drive addiction. Recognizing these differences helps in managing medications safely and addressing substance use disorders effectively.
Videos: Can Drugs Really Change Your Emotions Forever?
Why Do Drugs Make You Addicted So Fast?
The SHOCKING Truth About Dependence and Addiction
The Secret To Safer Medicines Revealed!
How Cravings Trick Your Brain Every Time