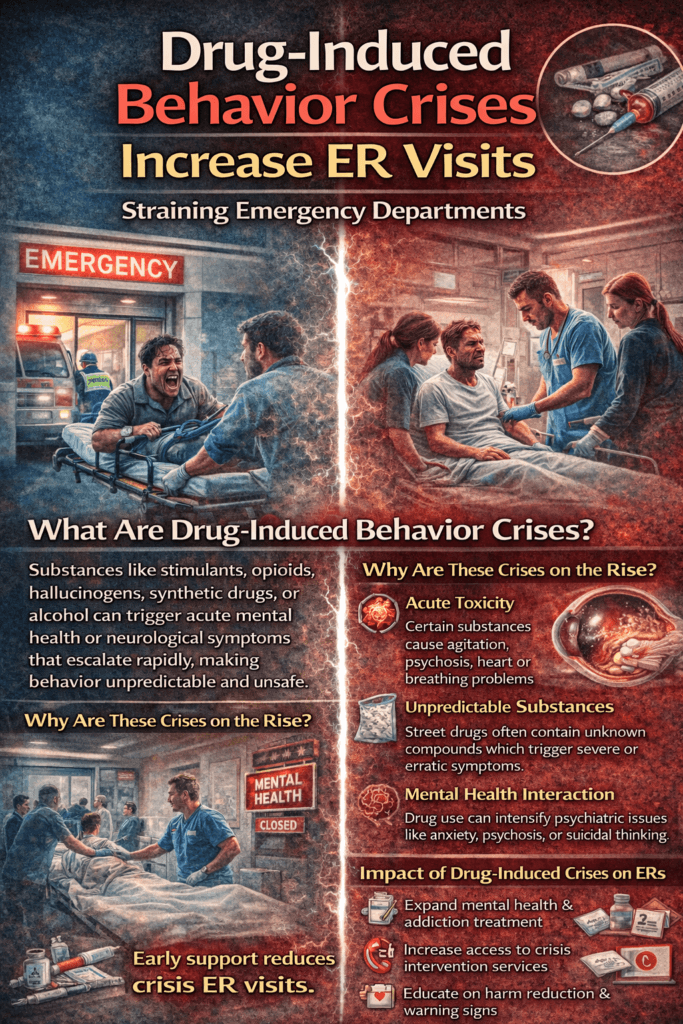
Drug-induced behavioral crises are an increasing cause of emergency room visits, straining patients and healthcare systems. Substances can disrupt brain chemistry and trigger symptoms like agitation, paranoia, hallucinations, panic, or confusion, making behavior unpredictable or unsafe. Limited access to early treatment, mental health care, and substance-use support often allows these issues to escalate into emergencies. Understanding this link is key to improving prevention, early intervention, and patient safety.
Drug-Induced Behavioral Crises and the Rising Burden on Emergency Rooms
Drug-induced behavioral crises are a growing driver of emergency room (ER) visits worldwide. These crises occur when substances—such as stimulants, opioids, hallucinogens, synthetic drugs, or alcohol—trigger acute psychological or neurological reactions that impair judgment, perception, and emotional control. Individuals may present with severe agitation, paranoia, hallucinations, confusion, aggression, or sudden medical instability. Because these symptoms can escalate rapidly and unpredictably, emergency departments often become the first point of care.
One major reason these cases increase ER visits is acute toxicity. Certain drugs overstimulate the brain and nervous system, causing dangerous spikes in heart rate, blood pressure, or body temperature. Others depress breathing or consciousness, leading to overdose or near-fatal respiratory suppression. Behavioral symptoms often accompany these medical emergencies, making them more complex to manage than routine intoxication.
Another contributing factor is drug unpredictability, especially with illicit or synthetic substances. Many street drugs are contaminated or mixed with unknown compounds, meaning users cannot predict potency or effects. This unpredictability raises the likelihood of sudden psychiatric or medical crises requiring urgent intervention. Synthetic stimulants, for example, are strongly associated with panic, psychosis, and violent agitation that necessitate rapid sedation and monitoring in ER settings.
Mental health interactions also play a significant role. People with underlying anxiety, depression, trauma histories, or psychotic disorders may experience intensified symptoms when using substances. Drug use can trigger acute episodes such as panic attacks, suicidal thoughts, or psychosis, prompting emergency evaluation. Even individuals without prior diagnoses can develop temporary drug-induced psychiatric states severe enough to require immediate care.
ER visits also rise because many individuals lack access to preventive or outpatient treatment. Limited addiction services, stigma, cost barriers, and lack of early intervention often delay help until a crisis occurs. When someone reaches a point of behavioral instability or medical danger, emergency departments become the default safety net.
These visits affect not only patients but also healthcare systems. Drug-related behavioral emergencies require intensive staff time, monitoring, and security resources. Patients may need sedation, imaging, toxicology testing, or psychiatric evaluation, which increases length of stay and strains already crowded ER environments.
Prevention strategies focus on early access to treatment, harm-reduction education, mental health support, and community-based crisis services. When individuals receive timely addiction care and psychological support, crises become less frequent and less severe. Expanding outpatient programs, mobile crisis teams, and public education can reduce reliance on emergency departments and improve outcomes.
Ultimately, drug-induced behavioral crises illustrate how substance use affects not only individuals but entire healthcare systems. Addressing root causes—addiction, untreated mental illness, and lack of resources—can lower ER visits, improve patient safety, and shift care from crisis response to prevention and recovery.
Self-Management Strategies to Prevent ER Visits From Drug-Induced Behavioral Crises
Drug-induced behavioral crises—such as severe agitation, panic, confusion, hallucinations, or emotional instability—are a leading reason individuals seek emergency care. These episodes can occur when substances disrupt brain chemistry, intensify underlying mental health symptoms, or interact unpredictably with medications. While emergency treatment is sometimes necessary, many crises can be prevented through intentional self-management strategies that strengthen emotional regulation, reduce risk triggers, and promote stability.
One of the most important strategies is self-awareness of triggers. Individuals benefit from identifying patterns that precede crises, such as specific substances, sleep deprivation, stress, or emotional distress. Tracking mood, substance use, and physical health in a journal or app can reveal early warning signs—like restlessness, racing thoughts, irritability, or paranoia—that remind you that intervention is needed before symptoms escalate.
Substance safety planning is another key step. Avoiding unknown or unregulated substances, not mixing drugs with alcohol or medications, and following prescribed dosing instructions can dramatically lower risk. Many behavioral emergencies occur when substances are combined or taken in higher amounts than intended. Setting personal limits and using accountability supports, such as reminders or trusted check-ins, can help maintain safer boundaries.
Emotional regulation skills provide powerful protection. Techniques like deep breathing, grounding exercises, progressive muscle relaxation, or mindfulness can calm the nervous system during early distress. These methods reduce the chance that anxiety or agitation spirals into a full crisis. Practicing coping strategies daily—not just during stress—builds resilience and makes them more effective when needed.
Maintaining physical stability is often overlooked but essential. Adequate sleep, hydration, nutrition, and regular movement help regulate brain chemistry and emotional balance. Substance-related crises are far more likely when the body is exhausted, dehydrated, or nutritionally depleted. Treating physical health as part of mental health can significantly reduce vulnerability.
Another protective measure is early help-seeking. Contacting a counselor, support line, sponsor, or healthcare provider at the first sign of escalating symptoms can prevent situations from becoming emergencies. Many people wait until distress becomes overwhelming, but early support often prevents crises from requiring hospital care.
Finally, structured daily routines provide stability. Predictable sleep times, meals, work or activity schedules, and relaxation periods reduce impulsivity and emotional volatility. Structure gives the brain consistency, which is especially helpful for individuals prone to mood swings or substance-related reactions.
In summary, preventing ER visits related to drug-induced behavioral crises is not about perfection—it is about preparation. Self-awareness, safer choices, coping skills, physical care, early support, and routine together create a protective framework that lowers risk and promotes stability. When individuals learn to recognize early warning signs and respond proactively, they can shift from crisis management to prevention, improving both safety and quality of life.
Family Support Strategies to Prevent ER Visits From Drug-Induced Behavioral Crises
Drug-induced behavioral crises—such as severe agitation, panic, confusion, hallucinations, or emotional instability—often lead to emergency room visits because symptoms can escalate quickly and feel unmanageable. While medical care is essential during acute episodes, families can play a powerful preventive role. With the right knowledge, communication skills, and supportive structure, relatives can help reduce the likelihood of crises developing in the first place and intervene early when warning signs appear.
One of the most effective family strategies is early recognition of warning signs. Changes such as sleep disruption, sudden mood swings, paranoia, irritability, withdrawal, or unusual behavior may signal that a crisis is building. Families who notice these shifts can intervene sooner—encouraging rest, hydration, or professional support before symptoms intensify. Early action often prevents situations from reaching emergency levels.
Supportive communication is equally important. Individuals experiencing substance-related distress may feel ashamed, fearful, or defensive. Approaching them calmly, without judgment, increases the chance they will accept help. Using statements like “I’m here for you” or “I want to help you stay safe” promotes trust rather than resistance. Avoiding confrontational language reduces emotional escalation, which can otherwise worsen behavioral symptoms.
Families can also create structured and safe environments. Consistent daily routines, predictable sleep schedules, and stable home settings reduce stress and emotional volatility. Encouraging balanced meals, hydration, and time for rest helps regulate the nervous system and decreases susceptibility to substance-related reactions. Structure provides a stabilizing framework that supports mental and physical health.
Another key strategy is planning ahead for crises. Families can work together with their loved one to create a written safety plan outlining early warning signs, coping strategies, emergency contacts, and preferred treatment options. Knowing what to do in advance prevents panic and allows everyone to respond calmly if symptoms begin to escalate. Preparation often prevents situations from becoming emergencies.
Encouraging professional support is also protective. Regular counseling, addiction treatment, medication management, or peer support groups can stabilize symptoms and reduce relapse or crisis risk. Families can assist by scheduling appointments, providing transportation, or reinforcing treatment goals. Practical assistance often removes barriers that might otherwise delay care.
Finally, families should prioritize their own well-being and education. Learning about the effects of substances, behavioral warning signs, and de-escalation techniques strengthens confidence and effectiveness. Support groups or counseling for family members can reduce stress and prevent burnout, allowing them to remain calm and consistent during challenging moments.
In the end, preventing ER visits related to drug-induced behavioral crises is not solely the responsibility of the individual—it is a collaborative effort. Families who combine awareness, empathy, preparation, and support create a protective environment that reduces crisis risk and promotes long-term stability. Their presence can transform moments of vulnerability into opportunities for intervention, healing, and recovery.
Community Resource Strategies to Prevent ER Visits From Drug-Induced Behavioral Crises
Drug-induced behavioral crises—episodes of severe agitation, paranoia, confusion, hallucinations, or emotional instability triggered by substances—are a major contributor to emergency room utilization. These crises often occur when individuals lack access to early support, preventive education, or timely mental health care. While emergency departments provide lifesaving treatment, communities can significantly reduce ER visits by building strong preventive systems that address risk factors before situations escalate.
One of the most effective strategies is developing accessible behavioral health services. Community mental health clinics, urgent psychiatric care centers, and walk-in stabilization units allow individuals to seek help at the first sign of distress rather than waiting until symptoms become emergencies. When care is affordable, nearby, and stigma-free, people are more likely to use it early, thereby reducing crisis severity and preventing ER dependence.
Mobile crisis response teams are another powerful tool. These teams—often composed of clinicians, counselors, or trained peer specialists—respond directly to individuals in distress within the community. Instead of defaulting to emergency departments or law enforcement, mobile teams can assess symptoms, provide de-escalation support, and connect individuals to appropriate services. This approach reduces unnecessary hospital visits while ensuring safety and stabilization.
Communities can also invest in substance use education and harm-reduction programs. Outreach initiatives that teach safer practices, recognize overdose signs, build emotional regulation skills, and identify early warning signs help individuals make informed decisions. Syringe service programs, drug-checking services, and peer education groups not only reduce medical complications but also create trusted entry points into treatment and counseling.
Peer-support networks further strengthen prevention. Recovery groups, mentorship programs, and community-based support circles provide connection, accountability, and shared experience. Isolation is a major risk factor for behavioral crises, while social support is one of the strongest protective factors. When individuals feel understood and supported, they are more likely to seek help before reaching a crisis point.
Another essential component is integrated social support systems. Housing assistance, employment programs, transportation services, and case management address external stressors that often worsen substance-related instability. When basic needs are met, individuals experience less stress and are less likely to enter states of emotional or behavioral crisis.
Finally, collaboration between hospitals, public health agencies, nonprofits, and community organizations creates a coordinated safety net. Shared referral systems, data-informed prevention programs, and cross-trained staff ensure that individuals receive the right level of care at the right time. This coordinated approach shifts the focus from emergency reaction to proactive prevention.
In summary, preventing ER visits caused by drug-induced behavioral crises requires community-level solutions that combine accessible care, education, outreach, peer support, and social services. When communities invest in prevention and early intervention, they reduce healthcare strain, improve individual safety, and promote long-term recovery. Strong community resources transform crisis response into crisis prevention—protecting both individuals and healthcare systems.
Frequently Asked Questions
Here are some common questions:
1. What should the main title say?
Your main title should be clear, concise, and impactful. A strong option is:
“Drug-Induced Behavioral Crises Increase ER Visits.”
Keep it bold and easy to read so viewers instantly understand the topic.
2. What subtitle works best?
Choose a short supporting line that adds context, such as:
“Understanding the Growing Strain on Emergency Care”
Subtitles should clarify the message without overwhelming the design.
3. What colors should be used?
Effective title pages often use contrast to convey urgency and meaning. For this topic:
- Cool blues → medical care, calm, clinical tone
- Reds/oranges → crisis, urgency, danger
A split or gradient background can visually represent the transition from crisis to treatment.
4. What images are appropriate?
Use visuals that communicate the theme without being graphic. Appropriate examples include:
- Emergency room entrance or staff
- Medical professionals assisting a patient
- Abstract medical icons or silhouettes
Avoid imagery that is overly distressing or stigmatizing.
5. What font styles work best?
Use a bold sans-serif font for the main title and a clean sans-serif font for the subtitles. Limit to two font styles to maintain professionalism and readability.
6. How should the layout be structured?
A balanced layout usually works best:
- Top → Title
- Center → Key image or visual concept
- Bottom → Subtitle or tagline
Centered alignment often looks professional and keeps the message focused.
7. Should icons or graphics be added?
Yes, but sparingly. Small icons (medical cross, heartbeat line, warning symbol) can reinforce the theme without cluttering the page.
8. What makes a title page visually engaging?
Strong contrast, a clear text hierarchy, and a single focal-point image help capture attention. Avoid overcrowding the design with too many elements.
9. How do you keep it professional for healthcare or educational use?
Use clean layouts, neutral fonts, realistic imagery, and medically accurate wording. Avoid slang, exaggerated claims, or sensational language.
10. What is the biggest mistake to avoid?
Overloading the page with text or graphics. A title page should introduce the topic—not explain everything. Simplicity makes it more impactful.
Conclusion
Although drug-induced behavioral crises can result in urgent medical situations, many of these ER visits are preventable with earlier support, education, and access to care. Expanding mental health services, substance-use treatment, crisis response programs, and community outreach can help individuals receive assistance before symptoms intensify. When warning signs are recognized early and appropriate resources are available, crises are less likely to reach emergency levels. Addressing the underlying causes—such as untreated addiction, stress, or psychiatric conditions—shifts the focus from reactive emergency care to proactive prevention, benefiting individuals, families, and healthcare systems alike.
Video: