Deprescribing benzodiazepines and oxycodone is a vital strategy to mitigate the risks of long-term use, including dependence and overdose. The benefits include improved cognitive function and overall health, but challenges such as withdrawal symptoms and ethical dilemmas regarding patient autonomy may arise. Community resource strategies are essential in supporting this process and providing education, alternative treatments, and emotional support to facilitate a safe transition. By addressing these aspects, healthcare providers can promote healthier outcomes for individuals undergoing deprescribing.
The Risks of Deprescribing Benzodiazepines and Oxycodone Without Proper Supervision
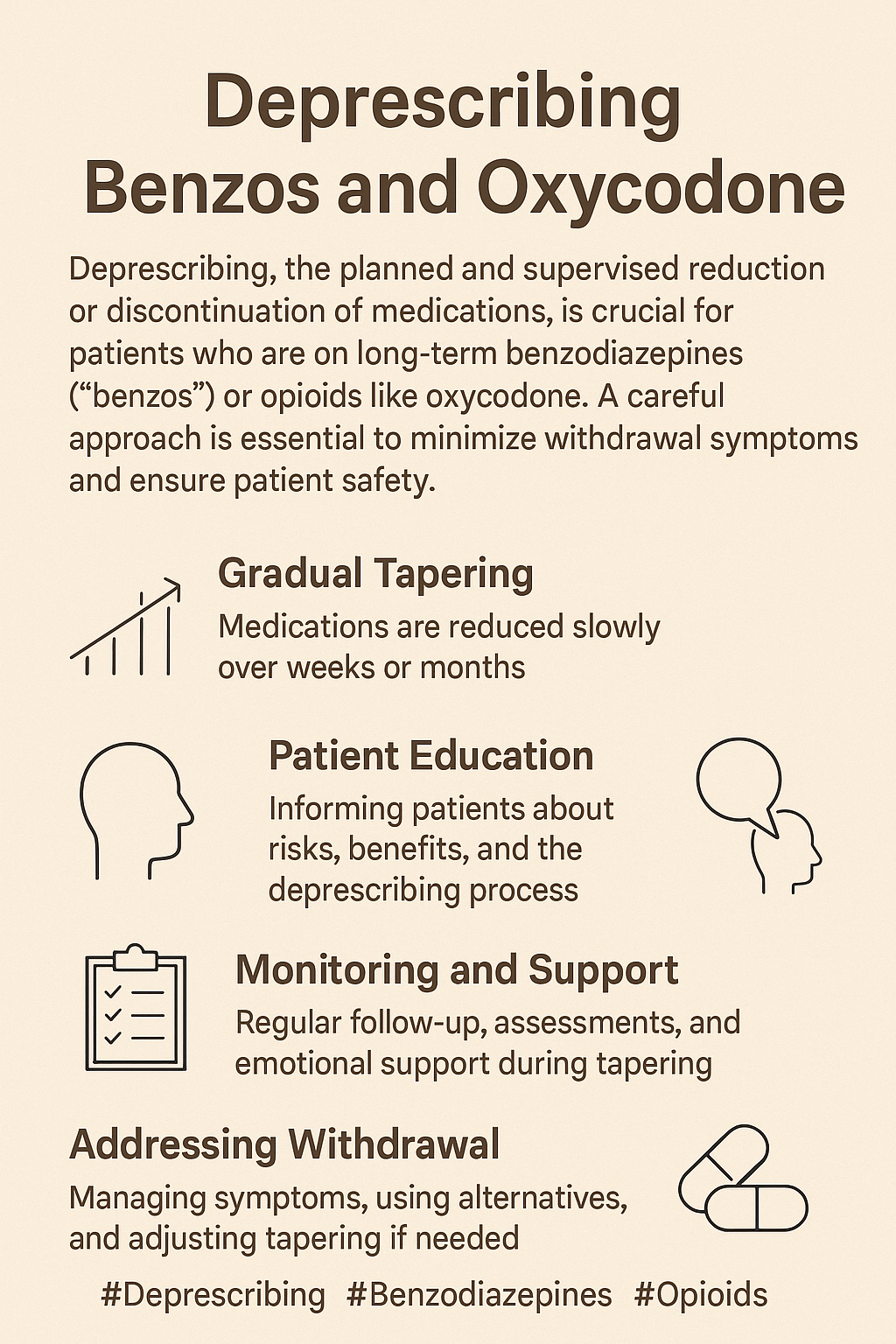
Deprescribing benzodiazepines (like Xanax and Valium) and opioids like oxycodone requires careful medical supervision. Abruptly stopping or quickly reducing these medications can lead to serious health risks, including withdrawal symptoms and, in some cases, even death. Here’s why proper tapering is essential:
1. Physical Dependence
- Why It Matters: Benzodiazepines and opioids create physical dependence, meaning the body adapts to their presence. When these medications are stopped suddenly, the body struggles to adjust, often resulting in intense withdrawal symptoms that can be dangerous if unmanaged.
2. Benzodiazepine Withdrawal Risks
- Seizures: Sudden discontinuation can cause the brain to become hyperactive, leading to seizures, which is the most severe withdrawal risk.
- Rebound Anxiety and Panic Attacks: Often, anxiety returns worse than before, adding significant psychological stress.
- Insomnia and Tremors: Loss of sleep and physical symptoms such as muscle cramps and tremors are common and can be taxing on the nervous system.
- Potential Fatality: In severe cases, abrupt benzodiazepine withdrawal can lead to fatal outcomes, particularly if compounded by other risk factors such as alcohol use.
3. Oxycodone Withdrawal Risks
- Severe Physical Symptoms: Abrupt oxycodone withdrawal often leads to intense pain, vomiting, diarrhea, and dehydration, which can be especially dangerous for the elderly or those with health issues.
- Anxiety, Restlessness, and Insomnia: These symptoms contribute to both physical and mental exhaustion.
- Health Complications: For people with heart or respiratory issues, rapid withdrawal can exacerbate these conditions, raising the risk of severe complications.
4. Increased Risk of Relapse and Overdose
- Tolerance and Relapse Risk: Without gradual tapering, the urge to alleviate withdrawal symptoms can increase the risk of relapse. If individuals resume their previous dosage after a period of abstinence, their lowered tolerance heightens the risk of overdose, which can be fatal.
5. The Importance of Tapering
- Safe, Gradual Reduction: To minimize these risks, benzodiazepines and opioids must be tapered slowly under medical supervision. This controlled reduction helps the body adapt, reducing withdrawal symptoms and the chance of severe complications, including death.
Attempting to deprescribe benzodiazepines and oxycodone without medical guidance can lead to serious health risks. Working with a healthcare provider for a carefully planned tapering process is crucial to ensure safe, effective deprescribing.
The Benefits of Deprescribing Benzodiazepines and Oxycodone for Long-Term Health and Wellness
Gradual, medically supervised deprescribing of benzodiazepines and oxycodone offers numerous advantages that support both physical and mental health. For individuals on long-term benzodiazepine or opioid therapy, tapering off these medications can lead to a better quality of life, enhanced cognitive function, and reduced health risks. Here are the key benefits of deprescribing these medications:
1. Reduced Risk of Dependence and Addiction
- Long-term use of benzodiazepines and opioids significantly raises the risk of physical dependence and addiction. Deprescribing offers a path to break this cycle, giving individuals more control over their health and reducing addiction-related consequences.
2. Improved Cognitive Function
- Prolonged use of benzodiazepines can impair memory, concentration, and cognitive agility. Gradual tapering improves mental clarity, sharper concentration, and restored memory, enhancing daily functioning.
3. Decreased Risk of Overdose
- As tolerance builds with prolonged opioid use, the risk of accidental overdose increases. By tapering off opioids like oxycodone, individuals can significantly reduce this life-threatening risk.
4. Prevention of Long-Term Side Effects
- For Benzodiazepines: Long-term use is linked to an increased risk of falls, fractures, and possibly dementia. Deprescribing helps lower these risks, especially for older adults.
- For Oxycodone: Extended use may lead to constipation, hormonal imbalance, immune suppression, and depression. Deprescribing can alleviate these symptoms, restoring normal bodily functions.
5. Improved Sleep Quality
- Although benzodiazepines are often prescribed for insomnia, long-term use can disrupt natural sleep cycles and cause dependence. Deprescribing supports the body’s return to a healthier, more natural sleep pattern, improving overall sleep quality.
6. Enhanced Emotional Stability
- Both benzodiazepines and opioids can influence mood, often leading to emotional blunting, mood swings, or even depression. Gradual tapering can help restore emotional balance, enhancing resilience and stability.
7. Lowered Risk of Drug Interactions
- Many people on benzodiazepines or opioids also take other medications, increasing the risk of adverse interactions. Deprescribing reduces the risk of harmful drug interactions, contributing to safer medication management.
8. Better Pain Management
- Long-term opioid use can lead to opioid-induced hyperalgesia, where pain sensitivity increases. Deprescribing may help the body recalibrate its natural pain response, leading to more effective pain management over time.
9. Increased Independence and Quality of Life
- By reducing reliance on these medications, many individuals experience greater independence, energy, and engagement in daily activities. Deprescribing can restore a sense of vitality and freedom from sedative side effects.
10. Reduced Health Care Costs
- Tapering off benzodiazepines and opioids lowers the financial burden associated with side effects, complications, and hospital visits linked to prolonged use. Fewer prescriptions mean reduced out-of-pocket costs as well.
11. Improved Mental Health
- Long-term benzodiazepine and opioid use has been associated with mental health challenges like anxiety and depression. Deprescribing, when done safely, often leads to improved mental well-being and a stronger sense of personal resilience.
Safely deprescribing benzodiazepines and oxycodone under healthcare supervision supports improved physical health, cognitive function, emotional well-being, and an overall enhanced quality of life. Gradual tapering is essential to ensure that individuals experience these benefits without risking severe withdrawal symptoms, helping them achieve lasting wellness.
Navigating the Ethical Dilemmas of Deprescribing Benzodiazepines and Oxycodone
Deprescribing benzodiazepines and oxycodone poses numerous ethical dilemmas that challenge healthcare providers in balancing patient autonomy, safety, and their professional responsibilities. Understanding these complexities is essential for delivering compassionate and effective care. Here are some key ethical concerns surrounding the deprescribing process:
1. Patient Autonomy vs. Safety
- Informed Consent: Patients often feel entitled to make informed decisions about their medications. When healthcare providers advocate for deprescribing, they may encounter conflicts between respecting a patient’s autonomy and prioritizing their safety.
- Resistance to Change: Patients may resist the idea of deprescribing due to fears of withdrawal symptoms or the belief that their current medication is critical for maintaining their quality of life. Providers must navigate these concerns while promoting long-term health benefits.
2. Withdrawal and Harm Reduction
- Withdrawal Risks: The potential for severe or life-threatening withdrawal symptoms, particularly with benzodiazepines, raises ethical questions. Providers must carefully consider whether the benefits of stopping the medication outweigh the risks of withdrawal.
- Harm Principle: The ethical obligation not to harm complicates decisions around deprescribing. If the process is likely to cause significant distress or adverse health outcomes, providers must evaluate if it is the appropriate course of action.
3. Informed Decision-Making
- Education and Communication: Patients must be fully informed about the risks and benefits of continuing or discontinuing their medications. Inadequate communication can lead to misunderstandings and ethical concerns regarding informed consent.
4. Provider Responsibility
- Duty to Care: Healthcare providers face the challenge of balancing their duty to alleviate suffering with the responsibility to address the risks associated with long-term use of benzodiazepines and opioids. This dual obligation can create tension in treatment decisions.
- Fear of Legal Repercussions: Concerns about potential legal or professional consequences related to prescribing or deprescribing these medications can influence provider decision-making and ethical obligations to the patient.
5. Socioeconomic Factors
- Access to Alternatives: Patients with limited access to mental health services, counseling, or alternative pain management strategies may struggle more during the deprescribing process. Ethical dilemmas arise when considering how socioeconomic status affects a patient’s ability to cope with discontinuation.
6. Chronic Pain Management
- Balancing Pain Relief and Dependence: For patients who rely on oxycodone for chronic pain management, deprescribing may result in uncontrolled pain. This creates ethical dilemmas about balancing effective pain relief with the risks of dependence and addiction.
7. Equity and Fairness
- Disparities in Care: Certain populations may face greater challenges during the deprescribing process due to existing health disparities. Ethical considerations arise concerning how to ensure equitable access to treatment and support during deprescribing efforts.
8. Impact on Trust
- Patient-Provider Relationship: The decision to deprescribe can strain the trust between patients and healthcare providers. Patients may feel abandoned or betrayed if their medications are suddenly withdrawn, undermining the therapeutic relationship.
9. Crisis Situations
- Withdrawal During a Crisis: In times of personal crisis—such as the loss of a loved one or acute stress—the timing of deprescribing may raise ethical concerns about the appropriateness of making significant changes to medication regimens.
10. Monitoring and Follow-Up
- Continuity of Care: Ethical dilemmas may arise regarding the adequacy of follow-up care and monitoring for patients undergoing deprescribing. Ensuring that patients have access to support during and after the process is crucial to avoid adverse outcomes.
While deprescribing benzodiazepines and oxycodone can be a vital step in promoting long-term health, it also presents significant ethical challenges. Healthcare providers must navigate these dilemmas with sensitivity and care, ensuring that the patient’s well-being remains at the forefront of their decision-making process. Addressing patient autonomy, withdrawal risks, and socioeconomic factors while maintaining a strong patient-provider relationship is essential for ethical and practical deprescribing.
Community Resource Strategies for Safe Deprescribing of Benzodiazepines and Oxycodone
Deprescribing benzodiazepines and oxycodone can be a challenging process for individuals seeking to improve their health and well-being. Community resource strategies play a crucial role in supporting this transition, focusing on education, access to alternative treatments, and ongoing support. These strategies help individuals navigate the deprescribing process safely, minimizing withdrawal symptoms while promoting overall wellness. Here are key community resource strategies to consider:
1. Patient Education Programs
- Workshops and Seminars: Organizing community workshops is essential to educate patients about the risks associated with long-term use of benzodiazepines and opioids. These sessions can also cover the benefits of deprescribing and available alternatives.
- Informational Materials: Distributing brochures, pamphlets, and online resources can help patients understand the deprescribing process, recognize withdrawal symptoms, and learn effective coping strategies.
2. Medication Management Services
- Pharmacist Consultation: Community pharmacies can provide medication management services, allowing pharmacists to review patients’ medication regimens and offer guidance on tapering schedules and potential side effects.
- Comprehensive Medication Reviews: Regular medication reviews with healthcare providers can assess the necessity of ongoing medication use and discuss options for deprescribing.
3. Support Groups and Peer Counseling
- Peer Support Groups: Establishing support groups for individuals transitioning off benzodiazepines and opioids creates a safe space for sharing experiences, challenges, and coping strategies.
- Peer Navigators: Training individuals in recovery to serve as peer navigators can provide valuable guidance and emotional support throughout the deprescribing process.
4. Access to Mental Health Services
- Therapy and Counseling: Promoting access to counseling services can address underlying issues such as anxiety and depression, which can be especially beneficial during the tapering process.
- Cognitive Behavioral Therapy (CBT): Encouraging the use of evidence-based therapies like CBT can help individuals manage anxiety and stress without relying on benzodiazepines.
5. Alternative Pain Management Resources
- Non-Pharmacological Treatments: Providing information about alternative pain management strategies, such as physical therapy, acupuncture, mindfulness, and exercise programs, can help individuals manage pain without opioids.
- Integrative Health Programs: Offering programs that combine conventional and complementary therapies can help patients find effective pain relief methods that do not involve long-term opioid use.
6. Coordinated Care Models
- Interdisciplinary Teams: Fostering collaboration among healthcare providers—including physicians, pharmacists, and mental health professionals—can create comprehensive care plans for patients undergoing deprescribing.
- Case Management Services: Implementing case management programs offers personalized support throughout the deprescribing process, ensuring continuity of care and regular follow-up.
7. Crisis Intervention Resources
- Emergency Support Lines: Establishing hotlines for individuals experiencing severe withdrawal symptoms or crises related to deprescribing ensures immediate access to support and resources.
- Crisis Counseling Services: Providing access to crisis counseling and mental health support can help individuals cope with acute distress during the transition off medications.
8. Community Awareness Campaigns
- Public Health Campaigns: Launching campaigns to raise awareness of the importance of safe deprescribing practices helps reduce stigma around addiction and promotes access to resources.
- Partnerships with Local Organizations: Collaborating with community organizations can broaden the reach of education and support services related to deprescribing.
9. Policy Advocacy
- Advocacy for Resources: Working with local and state policymakers to secure funding and resources for community-based programs focused on deprescribing and addiction recovery is essential for effective implementation.
- Support for Training Programs: Advocating for training healthcare providers on best practices for deprescribing and managing withdrawal ensures they are equipped to support patients effectively.
10. Online Resources and Telehealth Services
- Telehealth Options: Providing telehealth services for consultations and follow-ups makes it easier for individuals to access support without traveling.
- Online Educational Platforms: Developing websites and social media channels that offer resources, videos, and forums can help individuals seeking information about deprescribing.
By implementing these community resource strategies, individuals can receive the necessary support and education to transition safely off benzodiazepines and oxycodone. These efforts help foster a supportive environment that prioritizes health and well-being, ultimately empowering individuals to reclaim their lives without relying on these medications.
Conclusion
Deprescribing benzodiazepines and oxycodone offers significant advantages, including reduced dependence, improved cognitive function, and enhanced overall health. However, the process is not without challenges, such as potential withdrawal symptoms and ethical dilemmas regarding patient autonomy and informed consent. Community resource strategies are vital in supporting individuals through this transition, offering education, alternative treatment options, and emotional support. By addressing these multifaceted issues effectively, healthcare providers can ensure a safer and more successful deprescribing process, ultimately leading to better patient health outcomes.
Video: 4 Risks of Taking Benzos and Oxycodone Long Term