Deep brain stimulation (DBS) is a neurosurgical treatment involving electrode implantation to modulate brain activity. The device offers potential benefits for substance use disorder (SUD), like targeted treatment and long-term relief. However, DBS presents challenges, including invasiveness, high costs, variable effectiveness, and potential side effects, such as cognitive and emotional changes. Ethical concerns also arise regarding informed consent, personal identity, and access to treatment. Balancing these advantages and challenges is critical to effectively utilizing DBS for SUD.
Deep Brain Stimulation: A Potential Breakthrough for Substance Use Disorders
Deep brain stimulation (DBS) is a neurosurgical procedure that uses electrodes in specific brain regions to modulate neural activity. Initially explored for various neurological and psychiatric conditions, DBS is gaining attention as a potential treatment for substance use disorders (Here’s an overview of its mechanism, targets, benefits, challenges, and ongoing research on SUDs.
How DBS Works
- Electrode Implantation: Electrodes are implanted into targeted brain regions, connected to a pulse generator placed in the chest or abdomen, which sends electrical impulses to the brain.
- Modulation of Neural Activity: These electrical impulses regulate neuronal activity, influencing circuits related to mood, reward, and decision-making.
Targets for DBS in SUDs
- Nucleus Accumbens: Critical in the brain’s reward system, modulating this area can affect cravings and compulsive behaviors associated with addiction.
- Subthalamic Nucleus: This target is involved in impulse control and mood regulation and has been studied for its effects on addictive behavior.
- Ventral Capsule/Ventral Striatum: This area is associated with the reward system and has been a focus of DBS research for its role in addiction.
Advantages of DBS for SUDs
- Potential for Long-Term Relief: DBS may offer sustained relief from addiction symptoms and is beneficial for long-term management.
- Reversibility: Unlike other surgical options, DBS is reversible, allowing adjustments based on patient response.
- Reduction in Cravings: Evidence suggests DBS can help lower cravings and improve control over addictive behaviors.
- Complementary Treatment: DBS can be integrated with other therapies, such as medication and psychotherapy, enhancing overall treatment efficacy.
Disadvantages and Challenges
- Invasiveness: DBS requires brain surgery, which carries risks like infection, bleeding, and neurological complications.
- High Cost: The procedure can be expensive and not covered by all insurance plans, limiting access for some.
- Variable Response: Patient responses to DBS can vary and be influenced by individual factors and the specific brain targets targeted.
- Ethical Concerns: There are moral questions about the long-term impact of DBS on personality and autonomy, as well as potential unintended consequences.
- Complex Treatment Management: The complexity of DBS requires specialized medical expertise for monitoring and adjusting stimulation parameters.
Research and Development
Research on DBS for SUDs is ongoing, with some studies yielding promising results. However, more investigation is needed to evaluate its safety, effectiveness, and the best protocols for broader application. Current clinical trials are exploring optimal brain targets, stimulation parameters, and patient selection criteria.
Deep brain stimulation presents a novel approach to treating substance use disorders by modulating the neural circuits involved in addiction. While it shows promise, especially for individuals unresponsive to conventional treatments, challenges such as invasiveness, cost, and ethical concerns must be addressed. Continued research is essential for refining its application and understanding the long-term implications of this innovative treatment.
Ethical Dilemmas in Deep Brain Stimulation for Substance Use Disorder
The use of deep brain stimulation (DBS) in treating substance use disorder (SUD) raises critical ethical dilemmas that warrant careful examination. These concerns touch on the effects on patients, the nature of the treatment itself, and broader societal implications. Here are some critical ethical dilemmas associated with DBS for SUD:
1. Informed Consent
- Complexity of the Procedure: DBS involves a complex surgical procedure and ongoing adjustments to stimulation. It is vital that patients fully understand the associated risks, benefits, and uncertainties, as this complexity can hinder their ability to provide informed consent.
- Vulnerability of Patients: Individuals with SUDs may be in a vulnerable state, potentially compromising their capacity to make fully informed decisions regarding their treatment.
2. Autonomy and Personal Identity
- Impact on Identity: DBS can alter brain function and behavior, raising concerns about how these changes might affect the patient’s sense of self and autonomy. Alterations in personality or motivation can challenge their sense of agency.
- Involuntary Changes: There is a risk that DBS may induce involuntary changes in thoughts or behaviors, further complicating notions of self-control and autonomy.
3. Effectiveness and Uncertainty
- Variable Efficacy: DBS does not yield the same results for everyone, leading to ethical concerns about providing treatment with uncertain outcomes, especially in light of available alternative therapies that are less invasive.
- Long-Term Effects: The long-term effects of DBS on individuals with SUD remain largely unknown. Ethical considerations include monitoring and managing these effects and informing patients about potential unknown future outcomes.
4. Risks and Side Effects
- Surgical Risks: As a surgical intervention, DBS carries risks such as infection, bleeding, and neurological complications, necessitating a careful evaluation of these risks against the potential benefits of the treatment.
- Adverse Effects: DBS can result in cognitive, emotional, or physical side effects. Addressing and managing these side effects is an ethical obligation of healthcare providers.
5. Equity and Access
- Cost and Accessibility: The high cost of DBS may limit access for individuals who cannot afford it or have insufficient insurance coverage, raising ethical concerns about equitable access, particularly for underserved populations.
- Resource Allocation: Ethical considerations extend to how resources are allocated for DBS compared to other treatments, ensuring funds are directed effectively to benefit those in greatest need.
6. Psychological and Social Implications
- Social Stigma: The introduction of DBS may exacerbate social stigma surrounding mental health and addiction, especially if patients are seen as having “surgically altered” behaviors.
- Psychological Impact: The psychological effects of undergoing DBS and the changes that follow need careful management, as patients may struggle to adapt socially and emotionally.
7. Ethical Research Practices
- Clinical Trials: Conducting research on DBS for SUD raises ethical considerations regarding study design, informed consent, risk management, and transparency of results.
- Exploitation Concerns: It is essential to ensure that vulnerable populations are not exploited in research settings and that participation is voluntary and informed.
The ethical dilemmas surrounding deep brain stimulation for substance use disorder involve intricate issues related to informed consent, personal identity, treatment efficacy, risks, equity, and societal implications. Addressing these concerns requires ongoing dialogue among researchers, clinicians, patients, and ethicists to ensure that DBS is utilized responsibly and equitably in treatment settings.
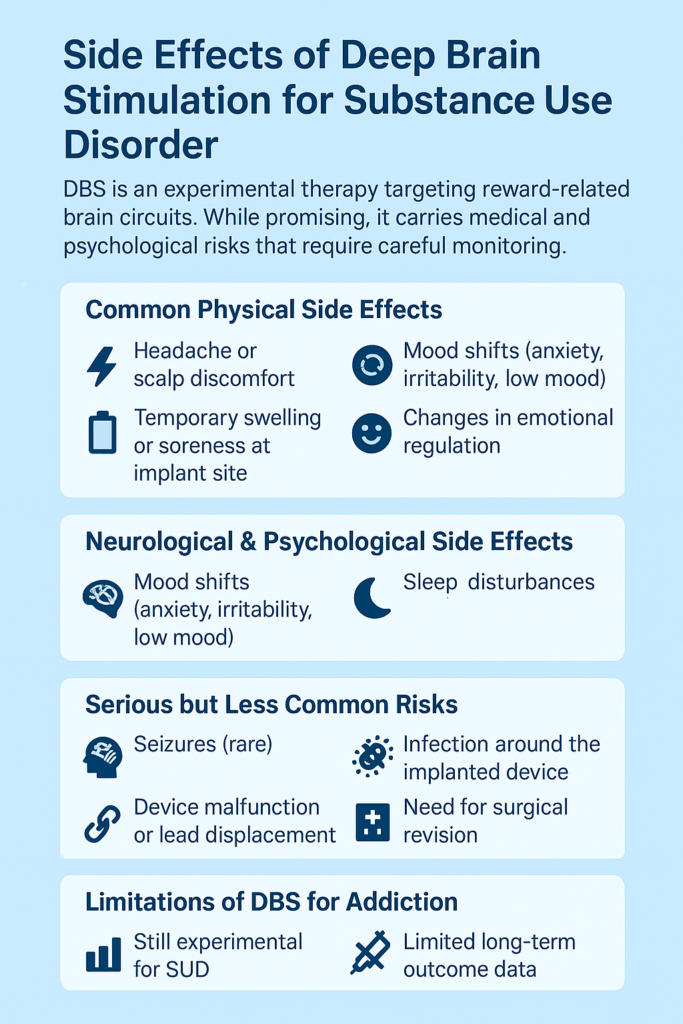
Side Effects of Deep Brain Stimulation for Substance Use Disorder
Deep brain stimulation (DBS) for substance use disorder (SUD) can lead to a variety of side effects, which may be physical, cognitive, emotional, or behavioral. The specific side effects often depend on factors like the targeted brain region, stimulation parameters, and individual patient differences. Here are some common and potential side effects associated with DBS:
1. Physical Side Effects
- Surgical Risks: As with any brain surgery, DBS carries risks such as infection, bleeding, and adverse reactions to anesthesia.
- Post-Surgical Pain: Patients may experience discomfort at the site of the implanted electrodes or pulse generator.
- Hardware Complications: Malfunction or displacement of electrodes can occur, sometimes requiring additional surgical intervention.
2. Cognitive Side Effects
- Memory Problems: Some patients may face difficulties with memory or concentration, though these effects can vary widely.
- Altered Thinking: Changes in cognitive functioning may arise, influenced by the targeted brain region and stimulation settings.
3. Emotional and Psychological Side Effects
- Mood Changes: DBS can result in mood swings, anxiety, or depression, affecting emotional regulation and potentially exacerbating existing mood disorders.
- Personality Changes: There is a risk of changes in personality or behavior due to the modulation of brain circuits involved in these areas.
4. Motor Side Effects
- Tremors or Spasms: Patients may experience involuntary muscle movements or tremors, mainly if motor areas of the brain are targeted.
- Coordination Issues: Changes in motor control and coordination can impact daily functioning.
5. Sensory Side Effects
- Altered Sensation: Depending on the targeted brain region, patients might experience changes in sensory perception, such as numbness or tingling.
6. Behavioral Side Effects
- Impulsivity: DBS may lead to increased impulsivity or compulsive behaviors, which can be concerning, especially in addiction treatment contexts.
- Changes in Reward Processing: Modulating reward-related brain circuits might alter how patients experience pleasure and reward, impacting motivation and behavior.
7. Adjustment and Tuning Issues
- Stimulation Adjustment: Finding the suitable stimulation parameters can be challenging, often requiring trial and error. Incorrect settings may lead to suboptimal results or heightened side effects.
- Adaptation: Patients may need time to adjust to the effects of DBS, with treatment effects potentially changing over time, necessitating ongoing adjustments.
8. Long-Term Effects
- Sustained Impact: The long-term effects of DBS on cognitive, emotional, and behavioral functioning are still under investigation, with potential unforeseen consequences arising from extended stimulation.
Deep brain stimulation for substance use disorder can result in a broad range of side effects, including physical, cognitive, emotional, and behavioral changes. While DBS offers promising treatment potential for SUD, careful management and monitoring are crucial to minimize these side effects and ensure that the benefits outweigh the risks. Ongoing research and personalized treatment adjustments are vital for optimizing patient outcomes and addressing any adverse effects that may arise.
Advantages of Deep Brain Stimulation for Treating Substance Use Disorder
Deep brain stimulation (DBS) presents several potential advantages for treating substance use disorder (SUD), especially for individuals who have not responded effectively to traditional therapies. Here are some key benefits:
1. Targeted Treatment
Precise Modulation: DBS enables accurate modulation of specific brain regions involved in addiction, such as the nucleus accumbens and subthalamic nucleus. This targeted approach can help regulate neural circuits linked to cravings and compulsive behaviors.
2. Potential for Long-Term Relief
Sustained Effectiveness: DBS can provide long-term relief from SUD symptoms by continuously modulating brain activity. This is particularly beneficial for ongoing management in cases where other treatments have been insufficient.
3. Reversibility and Adjustability
Adjustable Parameters: The stimulation parameters can be adjusted non-invasively after implantation, allowing for personalized optimization based on the patient’s response and any side effects. Reversibility: If necessary, the stimulation can be turned off or the device removed, offering flexibility in treatment management.
4. Complementary to Other Therapies
Integrated Approach: DBS can be used alongside other treatment modalities, such as medication, cognitive-behavioral therapy, and support groups, enhancing the overall effectiveness of addiction treatment.
5. Reduction in Cravings and Compulsive Behaviors
Craving Management: DBS can help reduce cravings and compulsive behaviors associated with addiction by modulating the brain’s reward and impulse control systems, supporting patients in achieving and maintaining sobriety.
6. Potential for Improved Quality of Life
Enhanced Functioning: By reducing the severity of addiction symptoms, DBS can improve overall functioning and quality of life, leading to better social interactions, greater employment stability, and enhanced emotional well-being.
7. Research and Evidence-Based Benefits
Promising Results: Preliminary research and clinical trials have shown encouraging results for DBS in managing addiction symptoms, offering a new treatment avenue for individuals with severe or treatment-resistant SUD.
8. Support for Relapse Prevention
Enhanced Control: Targeting brain areas involved in impulse control and reward processing, DBS can help individuals maintain control over their addiction, potentially reducing the risk of relapse.
9. Personalized Treatment
Customizable Approach: DBS treatment can be tailored to an individual’s specific needs and responses, enabling a more personalized approach to managing SUD.
Deep brain stimulation offers significant advantages for treating substance use disorder, including targeted modulation of brain regions involved in addiction, long-term relief, and customizable treatment options. While it can complement other therapies, reduce cravings, and enhance its quality, it’s crucial to consider these benefits alongside potential risks and side effects. DBS should be viewed as part of a comprehensive treatment plan for individuals struggling with SUD.
Challenges and Disadvantages of Deep Brain Stimulation for Substance Use Disorder
While deep brain stimulation (DBS) shows promise for treating substance use disorder (SUD), it also comes with several significant disadvantages and challenges:
1. Invasiveness and Surgical Risks
Surgical Complications: DBS involves brain surgery, which carries risks such as infection, bleeding, and adverse reactions to anesthesia.
Post-Surgical Issues: Patients may experience pain, swelling, or complications related to the implanted electrodes or pulse generator.
2. High Cost
Expensive DBS procedures: Ongoing management can be costly, posing a barrier for many individuals. This includes surgery, the device, and regular follow-up visits.
Insurance and Accessibility: Not all insurance plans cover DBS, limiting access for lower-income patients.
3. Variable Effectiveness
Inconsistent Results: DBS does not work for everyone, and its effectiveness can vary with individual differences and the targeted brain region.
Unpredictable Outcomes: Some patients may not experience significant improvements in their SUD symptoms, leading to frustration.
4. Side Effects and Complications
Physical Side Effects: Adverse effects may include tremors, coordination issues, or changes in sensory perception.
Cognitive and Emotional Impact: DBS can lead to mental issues like memory problems, as well as emotional changes, such as mood swings, anxiety, or depression.
5. Complexity of Treatment
Adjustment and Tuning: Finding optimal stimulation settings requires ongoing adjustments, which can be complex and time-consuming.
Device Management: Regular monitoring and maintenance of the DBS device adds to the treatment’s complexity.
6. Ethical and Psychological Concerns
Impact on Identity: Changes in personality, behavior, or self-perception raise ethical concerns about how DBS affects a person’s sense of self and autonomy.
Informed Consent: Due to the complexity of the procedure, ensuring that patients fully understand the potential risks and benefits can be challenging.
7. Limited Long-Term Data
Ongoing Research: The long-term effects of DBS for SUD are still under investigation, with limited data on the durability of its benefits and potential long-term risks.
Uncertain Future Effects: The potential long-term consequences of DBS on brain function and overall health remain unclear.
8. Social and Behavioral Implications
Social Stigma: The use of DBS may be associated with stigma or misconceptions, an “out “brain modified” ion,” affecting how patients are perceived.
Behavioral Changes: There is a risk of unintended behavioral changes, such as increased impulsivity or alterations in reward processing.
Deep brain stimulation for substance use disorder presents several disadvantages, including the invasiveness of the procedure, high costs, variable effectiveness, and potential side effects. The complexity of treatment and ethical concerns about its impact on identity and autonomy must also be carefully considered. While DBS offers potential benefits, it is essential to weigh these disadvantages against its advantages and to ensure the treatment is integrated into a comprehensive care plan.
Frequently Asked Questions
Here are some common questions:
Is DBS a cure?
No. DBS does not cure underlying conditions. It is a symptom-management tool that can significantly improve quality of life when other treatments have failed.
Who may be a candidate for DBS?
Candidates typically have severe symptoms that have not responded to standard treatments. Careful screening is required, including neurological, psychiatric, and cognitive evaluations.
What are the risks of DBS?
Risks include infection, bleeding, device malfunction, mood changes, cognitive effects, and surgical complications. Ongoing monitoring is essential to manage side effects.
Is DBS reversible?
Yes. DBS is adjustable and reversible. The device can be turned off or removed if needed, which is one advantage over permanent surgical procedures.
Conclusion
Deep brain stimulation (DBS) represents a promising yet complex treatment option for substance use disorder (SUD). Its advantages include targeted brain modulation and the potential for long-term symptom relief, which can significantly aid in addiction management. However, the procedure’s invasiveness, high costs, and the potential for side effects, such as cognitive and emotional changes, present considerable challenges. Additionally, ethical dilemmas surrounding informed consent, personal identity, and equitable access must be carefully addressed. While DBS offers significant potential, its integration into treatment plans requires careful consideration of these factors to ensure its benefits outweigh the risks and that it is used ethically and effectively.
Video: What happens when DBS goes wrong for addicts #MentalHealth #Warning