Cognitive dissonance is the internal conflict that arises when actions contradict personal beliefs or values. In addiction therapy, it can motivate change but also cause guilt, shame, or relapse if not managed well. Ethical concerns include emotional harm and perceived manipulation. To cope, individuals can use self-management skills like self-awareness, emotion regulation, and value clarification to reduce discomfort and stay aligned with recovery goals.
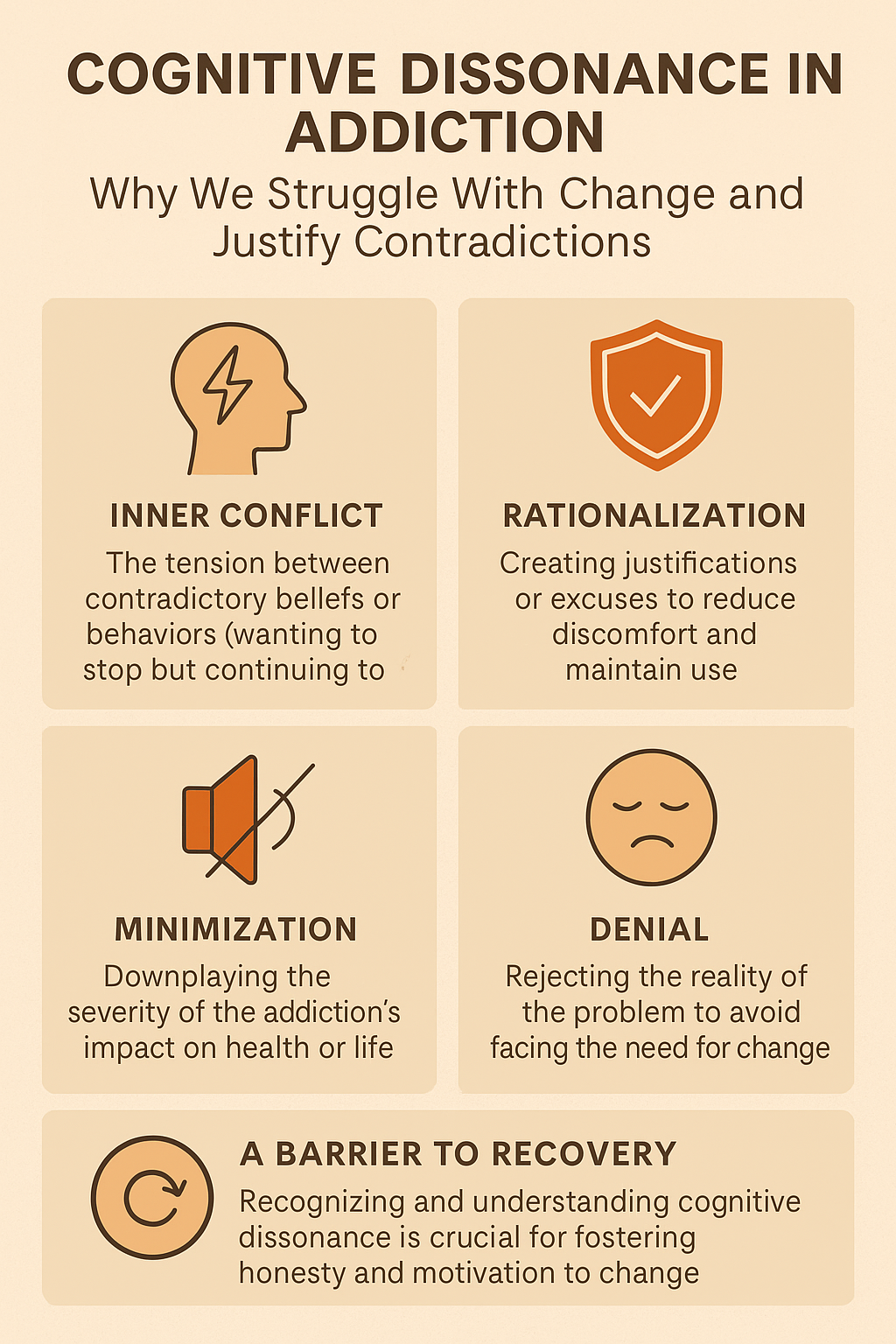
Cognitive Dissonance: Why We Struggle With Change and Justify Contradictions
Have you ever made a choice that felt wrong, even though you did it anyway? That uncomfortable feeling tugging at your mind might be cognitive dissonance—a psychological theory that explains the mental discomfort we feel when our actions contradict our beliefs or values.
🔄 What Is Cognitive Dissonance?
Cognitive dissonance occurs when someone holds two or more conflicting thoughts, especially when their actions clash with their values. This theory, developed by Leon Festinger in the 1950s, helps us understand why people sometimes behave in ways that don’t align with their beliefs.
🔍 Real-Life Example:
Imagine someone who deeply values their health—but smokes cigarettes. The internal conflict between valuing health and smoking creates mental tension. To reduce that discomfort, they might:
- Justify the behavior (“Smoking helps me relax after a stressful day.”)
- Change the behavior (Decide to quit smoking altogether.)
- Downplay the belief (“My grandfather smoked and lived to 90.”)
🧠 Why Cognitive Dissonance Matters
This theory reveals how people rationalize harmful behaviors, resist or embrace change, and defend their choices—even when they’re unsure. It plays a huge role in:
- Therapy and addiction recovery
- Behavior change programs
- Marketing, politics, and social movements
Understanding cognitive dissonance can help you recognize when you’re justifying actions that don’t align with your actual values—and give you tools to change.
In summary, whether you’re trying to break a habit, make a big life decision, or understand someone else’s behavior, cognitive dissonance gives us a window into the human mind. Once you’re aware of it, you can use that discomfort not to stay stuck—but to grow.
Using Cognitive Dissonance in Addiction Therapy: From Barrier to Breakthrough
Cognitive dissonance can play a decisive role in addiction therapy, both as a barrier to change and as a tool for motivation. Understanding and addressing this psychological conflict can significantly enhance treatment outcomes.
🔄 How Cognitive Dissonance Affects Addiction Therapy:
1. Internal Conflict Motivates Change
When individuals recognize that their substance use conflicts with their values (e.g., being a good parent, staying healthy), it creates emotional discomfort—dissonance. Therapists can use this discomfort to motivate behavior change.
- Example: A father who values being a role model may feel intense dissonance about drinking heavily in front of his children. Exploring this conflict can open the door to treatment engagement.
2. Resistance and Denial
To reduce dissonance without changing behavior, clients may:
- Minimize the severity of their use (“I’m not that bad”),
- Justify it (“I need it to cope”),
- Or reject help (“Treatment doesn’t work for me”).
These are defense mechanisms to reduce discomfort without facing change.
3. Enhancing Motivation through Therapy
Motivational Interviewing (MI), a common addiction therapy technique, directly addresses cognitive dissonance. It:
- Helps clients explore their ambivalence,
- Elicits their own reasons for change,
- And increases internal motivation rather than imposing external pressure.
4. Relapse and Guilt
After relapse, individuals may experience intense dissonance: “I said I wanted to quit, but I used again.” This can cause shame, which may either motivate renewed effort or trigger further use as a coping mechanism. How the therapist helps process this dissonance is crucial.
🧠 Therapeutic Implications:
- Encourage honest reflection on values and goals.
- Use dissonance constructively to support behavior change.
- Normalize ambivalence and help clients resolve it rather than avoid it.
The Hidden Risks of Cognitive Dissonance in Addiction Therapy: What Clinicians Need to Know
While cognitive dissonance can be a powerful tool in addiction therapy, it also carries several disadvantages if not approached with care and sensitivity. Without proper support, the internal conflict it creates can do more harm than good. Here’s a breakdown of the main challenges clinicians and clients may face:
❗ Disadvantages of Cognitive Dissonance in Addiction Therapy
1. Emotional Overload
- Feelings of discomfort, guilt, and shame can become emotionally overwhelming.
- Instead of motivating change, this can lead to emotional shutdown, denial, or defensiveness.
Example: A client who relapses may feel so ashamed they avoid returning to therapy altogether.
2. Increased Risk of Relapse
- Some individuals may attempt to escape dissonance by using substances rather than confronting it.
- This can create a destructive loop:
use → guilt → dissonance → more use.
3. Resistance to Therapy
- Clients who feel judged or are forced to confront painful contradictions too early may become resistant.
- In the early stages of recovery, this discomfort can trigger avoidance or even treatment dropout.
4. Self-Stigma and Identity Crisis
- Constant awareness of inner conflict can reinforce negative self-perceptions, such as:
- “I’m a failure.”
- “I’m weak.”
- “I’ll never change.”
- These beliefs can undermine self-efficacy, a key driver of sustained recovery.
5. Maladaptive Coping Mechanisms
- To reduce discomfort, clients might change their beliefs rather than their behavior (e.g., “Maybe my drinking isn’t really a problem”).
- Others may resort to rationalizing harm, shifting blame, or minimizing consequences—all of which reinforce addictive patterns.
6. Therapist Misuse or Overreliance
- Relying too heavily on dissonance without providing emotional scaffolding can backfire.
- Some clients may not be emotionally ready to process their internal conflicts, especially if they have unresolved trauma.
🧠 Best Practice:
To reduce harm and improve outcomes, therapists should:
- Use Motivational Interviewing and trauma-informed approaches.
- Pace interventions to meet the client’s readiness and emotional capacity.
- Provide consistent validation and emotional support.
- Ensure clients feel safe, not judged, when exploring brutal truths.
In summary, cognitive dissonance is a double-edged sword in addiction therapy. When wielded with skill and compassion, it can motivate lasting change. But when used carelessly, it can push clients deeper into shame, resistance, or relapse. The key lies in using it wisely, gently, and with empathy.
Ethical Dilemmas of Using Cognitive Dissonance in Addiction Therapy: Navigating the Fine Line
Cognitive dissonance can be a powerful tool in addiction therapy, helping clients confront contradictions between their values and behaviors. However, its use comes with ethical risks. If mishandled, it can undermine trust, cause emotional harm, or compromise a client’s autonomy. Below are the key ethical dilemmas therapists must consider:
⚖️ Ethical Dilemmas of Using Cognitive Dissonance in Addiction Therapy
1. Manipulation vs. Motivation
- Dilemma: Encouraging awareness of dissonance may empower change—but if pushed too hard, it can feel coercive.
- Risk: Clients may feel pressured to adopt beliefs or behaviors that aren’t truly their own.
- Ethical Principle: Respect for Autonomy
2. Shame and Emotional Harm
- Dilemma: Pointing out discrepancies may inadvertently trigger shame, guilt, or emotional collapse.
- Risk: Instead of motivating recovery, this may lower self-esteem and increase the risk of relapse.
- Ethical Principle: Nonmaleficence (Do No Harm)
3. Cultural and Value Assumptions
- Dilemma: Therapists may unintentionally project their own moral or cultural standards when identifying behavioral “conflicts.”
- Risk: Clients may feel misunderstood, judged, or invalidated—mainly if their values differ from societal norms.
- Ethical Principle: Cultural Humility and Respect for Diversity
4. Premature Confrontation
- Dilemma: Introducing dissonance too early in therapy may overwhelm clients who are still building trust or emotional resilience.
- Risk: Can lead to resistance, shutdown, or withdrawal from therapy.
- Ethical Principle: Beneficence (Act in the Client’s Best Interest)
5. Informed Consent and Transparency
- Dilemma: Clients may not know that their discomfort is being intentionally explored as a strategy for change.
- Risk: If not clearly communicated, this can violate informed consent and damage therapeutic trust.
- Ethical Principle: Fidelity and Informed Consent
✅ Ethical Best Practices for Therapists:
To use cognitive dissonance ethically and effectively in addiction therapy:
- Use a collaborative, client-centered approach (such as Motivational Interviewing).
- Frame dissonance as a curiosity-based exploration, not a confrontation.
- Validate emotions and avoid blame or moral judgment.
- Monitor client distress and adjust the pace of exploration accordingly.
- Be transparent about the therapeutic process and involve clients in understanding how dissonance is used.
In summary, when used with care, cognitive dissonance can be a catalyst for profound transformation. But therapists must remain mindful of its ethical boundaries, using it to empower—not pressure—clients. With empathy, transparency, and cultural awareness, cognitive dissonance becomes not a weapon, but a mirror—reflecting truths clients are ready to face, in their own time.
8 Self-Management Skills to Cope with Cognitive Dissonance in Addiction Recovery
Self-management skills are critical in addiction therapy, especially when clients face cognitive dissonance—the inner tension that arises when behavior doesn’t align with personal values. These tools empower individuals to respond thoughtfully to discomfort, reduce the risk of relapse, and stay aligned with recovery goals.
🧠 Self-Management Skills to Cope with Cognitive Dissonance in Addiction Therapy
1. Self-Awareness
- Recognize early signs of dissonance, such as guilt or inner conflict.
- Use mindful journaling or mood tracking apps to spot behavior-value mismatches and triggers.
2. Cognitive Restructuring
- Challenge harmful self-talk (e.g., “I relapsed, so I’m a failure”).
- Reframe thoughts to support resilience:
“This setback is part of the process—I’m still making progress.”
3. Value Clarification
- Identify core values like health, honesty, or family and bring them into focus.
- Use vision boards, value sort cards, or daily affirmations to stay grounded in what matters most.
4. Emotion Regulation
- Learn to tolerate distress without resorting to substance use through techniques such as:
- Deep breathing
- Grounding exercises
- Progressive muscle relaxation
- Mindfulness or guided meditation apps
5. Problem-Solving
- When dissonance hits, pause and assess:
- What’s the core conflict?
- What choices do I have?
- Which option supports my recovery and values?
6. Self-Compassion
- Be kind to yourself in moments of struggle.
- Replace harsh self-judgments with affirming self-talk:
“I’m learning. I’m trying. I’m human.”
7. Relapse Prevention Planning
- Identify high-risk situations that may create dissonance (e.g., family gatherings, workplace stress).
- Build a coping toolkit with supportive contacts, distraction techniques, and emergency strategies.
8. Accountability Support
- Regularly share progress with a therapist, sponsor, or peer group.
- Use check-ins to reflect on how well your actions align with your values—and gently course-correct when needed.
In summary, cognitive dissonance is a normal and even necessary part of the recovery journey. With self-management skills, individuals can move from emotional conflict to clarity, using discomfort as a catalyst for healing and personal growth. These tools aren’t just for surviving recovery—they’re for thriving in it.
Encourage clients to create a “Dissonance Response Plan”—a personal guide outlining steps they’ll take when they feel conflicted between their actions and values.
Frequently Asked Questions
Here are some common questions:
Question: What is a sample Cognitive Dissonance Exploration Worksheet?
Answer: Cognitive Dissonance Exploration Worksheet designed for use in addiction therapy. It helps clients identify their conflicting beliefs and behaviors, understand their discomfort, and explore paths toward change.
🧠 Cognitive Dissonance Exploration Worksheet
Name: ______________________
Date: ______________________
Therapist: ______________________
1. Identify the Behavior
What behavior or habit are you currently struggling with?
✎ ________________________________________________________________
✎ ________________________________________________________________
2. Identify Your Beliefs or Values
What values or beliefs do you hold that conflict with this behavior?
☐ I want to be a healthy person.
☐ I want to be a good parent/partner/friend.
☐ I believe in being responsible.
☐ I want to be financially stable.
☐ Other: ________________________________________________________
3. Describe the Conflict
In what ways does your behavior conflict with your values or beliefs?
✎ ________________________________________________________________
✎ ________________________________________________________________
4. How Do You Feel About This Conflict?
☐ Anxious
☐ Guilty
☐ Angry
☐ Ashamed
☐ Confused
☐ Motivated
☐ Other: _______________________
5. How Have You Tried to Resolve the Conflict So Far?
☐ Justified the behavior (“I deserve this”)
☐ Ignored it (“It’s not that big of a deal”)
☐ Changed my beliefs
☐ Tried to quit/change the behavior
☐ Other: ________________________
6. What Might You Be Willing to Do Now?
☐ Explore this further in therapy
☐ Try small behavior changes
☐ Learn coping skills or triggers
☐ Reconnect with my values
☐ Set a short-term goal: __________________________________________
7. Reflection
What did you learn about yourself through this exercise?
✎ ________________________________________________________________
✎ ________________________________________________________________
Question: What is a sample Dissonance Response Plan Worksheet?
Answer:
Dissonance Response Plan Worksheet that individuals in addiction therapy can use to recognize and manage cognitive dissonance in a healthy, proactive way. It’s designed to reduce the risk of relapse and reinforce recovery-oriented decision-making.
🧠 Dissonance Response Plan Worksheet
Name: ______________________
Date: ______________________
Therapist or Coach: ______________________
1. Recognize the Conflict
Describe a recent situation where your actions conflicted with your values or recovery goals.
✎ ____________________________________________________________________
✎ ____________________________________________________________________
2. Identify the Dissonant Feelings
What emotions did you experience during or after the conflict?
☐ Guilt
☐ Shame
☐ Anger
☐ Confusion
☐ Anxiety
☐ Other: _____________________
3. What Value Was Violated?
Which of your personal values or goals was this behavior in conflict with?
☐ Health
☐ Family or relationships
☐ Honesty
☐ Sobriety
☐ Responsibility
☐ Other: ______________________
4. Immediate Reactions
How did you respond? (Check all that apply)
☐ I justified the behavior
☐ I ignored or minimized it
☐ I used it again to cope
☐ I talked to someone
☐ I reflected on it
☐ I took a recovery-based action
☐ Other: ______________________
5. Coping Tools to Use Instead
List at least 3 healthy strategies you can use next time dissonance arises.
Examples: Call sponsor, journal, practice breathing exercises, attend a meeting, take a walk, revisit value list
6. Self-Compassion Statement
Write something kind and supportive to say to yourself when dissonance hits.
✎ “”
✎ “”
7. Short-Term Recovery Goal
What small, specific step can you take today to realign with your values?
✎ ____________________________________________________________________
8. Support System
Who can you reach out to when you feel stuck in dissonance?
☐ Sponsor: _____________________
☐ Therapist: ____________________
☐ Family/Friend: ________________
☐ Peer Support Group: ___________
Question: What family support strategies can help an individual with Cognitive dissonance of their addiction?
Answer: Family Support Strategies to Help an Individual Experiencing Cognitive Dissonance in Addiction Recovery
Cognitive dissonance can cause intense emotional discomfort for individuals in addiction recovery—especially when they feel torn between their actions (e.g., substance use) and personal values (e.g., being a good parent or living a healthy life). Families play a critical role in supporting the individual through this inner conflict by fostering safety, trust, and motivation for change. Here are evidence-informed family support strategies:
🧠 1. Create a Nonjudgmental Environment
- Why it helps: Shame increases dissonance and can lead to avoidance or relapse.
- How to do it: Use language that is supportive, not blaming. Focus on behaviors and values, not character flaws. Example: Instead of “You keep messing up,” try “I know this has been hard, and I see you’re trying.”
💬 2. Encourage Open, Honest Conversations
- Why it helps: Cognitive dissonance thrives in secrecy and isolation.
- How to do it: Ask questions with curiosity, not confrontation. Allow them to express their internal conflicts without fear of criticism. Ask: “What parts of your recovery are feeling most difficult right now?”
🎯 3. Gently Reflect Their Values
- Why it helps: Reminding individuals of their own values can increase internal motivation to change.
- How to do it: Acknowledge moments when their actions align—or don’t—with their stated goals, but do so kindly. Example: “You said you wanted to be more present for your kids, and going to that meeting today really showed that.”
🧩 4. Support Emotional Regulation
- Why it helps: Dissonance often accompanies intense emotions such as guilt, anger, or shame.
- How to do it: Help them manage these feelings by suggesting healthy coping strategies, such as going for a walk, talking, or using calming techniques.
👐 5. Normalize the Experience of Dissonance
- Why it helps: Knowing dissonance is common can reduce shame and promote reflection.
- How to do it: Let them know it’s normal to feel conflicted in recovery. Share examples from others (or yourself, if appropriate) about struggling with change.
📘 6. Educate Yourself About Addiction and Recovery
- Why it helps: Understanding addiction as a brain-based, behavior-influencing condition enables you to support more effectively.
- How to do it: Attend family education programs, read reputable resources, or join support groups like Al-Anon or SMART Family & Friends.
💡 7. Avoid Enabling or Extreme Ultimatums
- Why it helps: Overly harsh reactions can increase dissonance but reduce hope and safety.
- How to do it: Set healthy boundaries while keeping communication open and compassionate.
🤝 8. Promote Professional Support
- Why it helps: Therapists trained in techniques like Motivational Interviewing can skillfully navigate cognitive dissonance.
- How to do it: Encourage therapy or support groups in a supportive way—never as punishment or guilt. Try: “Would it help to talk to someone who can help you sort through how you’re feeling?”
🧭 Final Thought:
Family members can’t erase cognitive dissonance, but they can help the person feel safe enough to face it. Supportive families validate the struggle, reinforce positive steps, and stay connected even when recovery is messy. Their role isn’t to fix the dissonance—but to walk beside their loved one as they work through it.
Conclusion
Cognitive dissonance plays a complex but essential role in addiction therapy. While it can encourage positive change by highlighting conflicts between behaviors and values, it also poses risks, including emotional distress, relapse, and ethical concerns, if misused. Addressing these challenges with practical self-management skills—like mindfulness, self-reflection, and emotional regulation—can help individuals navigate dissonance constructively and support long-term recovery. When applied thoughtfully, cognitive dissonance can be a powerful tool for growth rather than a barrier to healing.
Video: Is Cognitive Dissonance Secretly Sabotaging Your Recovery?