As addiction treatment policy shifts under the Trump administration, there is a growing emphasis on state control, reduced federal funding, and a law enforcement-focused approach over public health. These changes may limit access to evidence-based care, especially for vulnerable groups relying on Medicaid or community services. In response, stakeholders must advocate for access to treatment, equitable funding, and harm-reduction strategies to protect recovery pathways amid policy changes.
Shifting Priorities: How Trump-Era Policy Changes Are Reshaping Addiction Treatment in America
The Trump administration has introduced significant changes to addiction treatment policies, drawing both support and concern from across the healthcare landscape. While efforts to reduce overdose deaths are central to the administration’s goals, shifts in agency structure, funding, and Medicaid policy may have far-reaching effects on the accessibility and quality of addiction care.
Key Policy Changes:
1. Agency Restructuring
The Substance Abuse and Mental Health Services Administration (SAMHSA) has been dissolved and absorbed into the newly formed Administration for a Healthy America (AHA). This consolidation aims to streamline public health efforts but has raised alarms about the potential loss of dedicated focus on mental health and substance use disorders.
2. Funding Reductions
Roughly $11 billion in federal funds for addiction and mental health—originally expanded during the COVID-19 crisis—has been slashed. State public health departments and nonprofit organizations are already feeling the impact through limited services and program closures, particularly in underserved areas.
3. Medicaid and Insurance Reforms
Proposed reforms could give states more leeway in defining “essential health benefits”, potentially weakening coverage for addiction treatment services. These changes risk creating coverage gaps for those relying on Medicaid or private insurance to access recovery programs.
4. Policy Priorities
The administration has emphasized reducing overdose deaths—especially those linked to fentanyl—while enhancing treatment options that lead to long-term recovery. It also aims to secure global supply chains to curb drug trafficking.
Implications:
These policy shifts reflect a desire to reduce bureaucratic overhead and focus on overdose prevention. However, stakeholders are concerned about the unintended consequences, particularly for individuals who rely on publicly funded services. The elimination of SAMHSA and reduction in funding may hinder progress made in tackling the opioid epidemic.
To navigate this evolving landscape, policymakers, healthcare providers, and community advocates must stay engaged. Balancing cost efficiency with the need to maintain strong treatment infrastructures will be key. Ongoing dialogue, evaluation, and local-level innovation can help ensure that reforms strengthen—not weaken—the nation’s response to substance use disorders.
Ultimately, the path forward must prioritize access, equity, and evidence-based care—ensuring that all individuals, regardless of where they live or how much they earn, have the support they need to recover.
7 Strategies Healthcare Providers Can Use to Safeguard Addiction Treatment Amid Trump-Era Policy Changes
With recent Trump administration reforms—such as the dismantling of SAMHSA, funding cuts, and Medicaid restructuring—addiction treatment services face increasing uncertainty. Despite these shifts, healthcare providers remain central to preserving access and quality of care for individuals with substance use disorders (SUDs). Here’s how providers can respond and adapt:
✅ 1. Advocate for Patients and Policy Stability
- Participate in advocacy at the local, state, and national levels.
- Join professional groups (like ASAM or AMA) that push for evidence-based addiction policy.
- Educate legislators on the real-world impacts of SUD treatment.
🧠 2. Stay Informed and Adapt Clinical Practices
- Keep current on policy shifts, insurance billing, and clinical guidelines.
- Maintain access to medications for opioid use disorder (MOUD) despite budget constraints.
- Leverage telehealth and mobile services to reach marginalized populations.
🤝 3. Strengthen Community and Referral Networks
- Collaborate with nonprofits, shelters, and community orgs still offering services.
- Ensure warm handoffs and care coordination remain intact.
- Share training and resources across agencies to bridge service gaps.
💡 4. Maximize Use of Available Resources
- Seek state and private grants to offset federal cuts.
- Bill is effectively using CPT and Medicaid codes for treatment services.
- Train peer recovery coaches and support staff to expand care capacity cost-effectively.
🧰 5. Integrate Addiction Care into Primary and Emergency Settings
- Train frontline teams to identify and initiate SUD treatment.
- Set up low-barrier access points for patients needing help.
- Use evidence-based screening tools to intervene early.
🧭 6. Provide Education and Reduce Stigma
- Reinforce the understanding that addiction is a treatable medical condition.
- Promote trauma-informed, nonjudgmental approaches to care.
- Normalize open conversations about addiction and recovery.
🔄 7. Collect Data and Monitor Outcomes
- Track outcomes to prove the effectiveness of addiction services.
- Use data to secure funding and demonstrate community impact.
- Share metrics with local stakeholders to build support and visibility.
While policy changes pose real challenges, healthcare providers are uniquely positioned to protect and evolve addiction treatment systems. Through advocacy, innovation, collaboration, and education, they can help ensure that recovery remains within reach—even during turbulent political times.
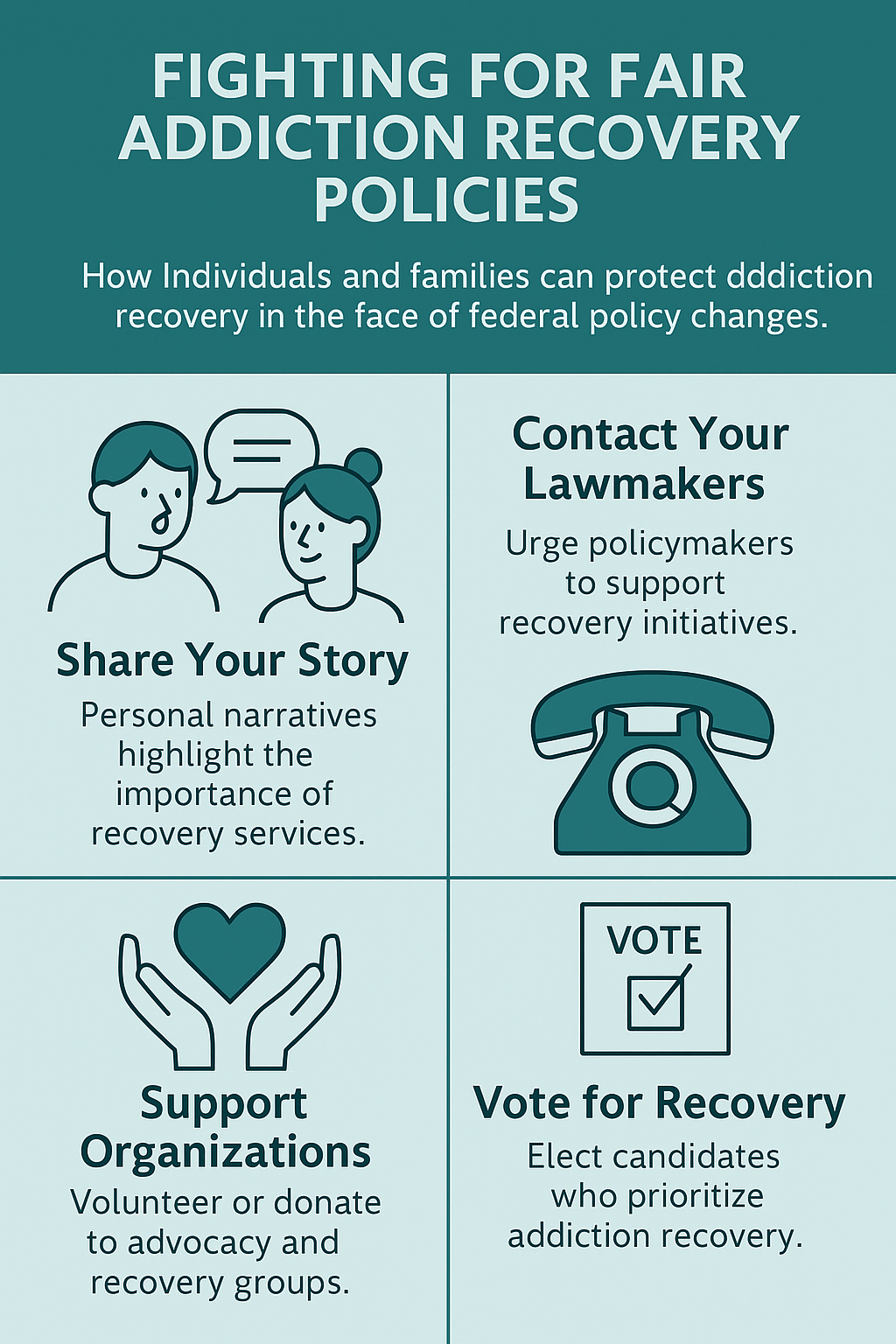
How Individuals and Families Can Protect Addiction Recovery in the Face of Federal Policy Changes
As addiction treatment policies shift under the Trump administration—with reduced federal support, Medicaid changes, and agency restructuring—people with addiction and their families can be powerful agents of change. By advocating, educating, and organizing, families and individuals can help safeguard access to treatment and recovery supports in their communities.
🧭 What People with Addiction and Their Families Can Do
1. 🗣️ Advocate for Access to Care
- Contact lawmakers to demand continued funding for addiction treatment.
- Share personal stories to highlight the human cost of policy cuts.
- Support advocacy organizations like Shatterproof, NAMI, or Faces & Voices of Recovery.
2. 📚 Stay Informed About Rights and Resources
- Learn which services remain covered under Medicaid, private insurance, or state programs.
- Keep track of local support options, including sliding-scale or nonprofit clinics.
- Monitor policy changes related to telehealth, harm reduction, and MOUD.
3. 🤝 Join or Create Mutual Support Networks
- Engage with groups like SMART Recovery, Al-Anon, or AA/NA.
- Build neighborhood coalitions to share resources and coordinate care.
- Connect with peer recovery coaches for navigation and mentorship.
4. 💬 Reduce Stigma Through Education and Dialogue
- Talk openly about addiction as a medical condition, not a personal failure.
- Host or attend educational events in schools, workplaces, and places of worship.
- Promote awareness of medication-assisted treatment (MAT) and recovery science.
5. 🧾 Track and Document Treatment Barriers
- Keep records of denied services, excessive wait times, or unaffordable care.
- Report issues to state ombudsmen, advocacy groups, or legal aid services.
- Use documentation to inform media, policy campaigns, or class actions.
6. 🔄 Plan for Continuity and Crisis
- Identify alternative providers in case of sudden closures or funding loss.
- Create an emergency recovery plan with contact info, meds, and transport options.
- Communicate proactively with doctors and pharmacies to avoid treatment interruptions.
7. 🏛️ Get Involved in Local Health Planning
- Join health boards, advisory councils, or public forums.
- Vote on local initiatives that fund addiction and mental health services.
- Advocate for municipal investment in local recovery infrastructure.
Even amid federal policy rollbacks, families and individuals are not powerless. By organizing at the grassroots level, demanding accountability, and lifting community-based solutions, they can protect hard-won gains in addiction care and help ensure that no one is left behind on the path to recovery.
Community Power: Strategies to Protect Addiction Recovery Amid Federal Policy Changes
As federal addiction treatment policies shift—through funding cuts, agency restructuring, and reduced regulatory protections—communities are stepping up to fill the gaps. Whether you’re a provider, advocate, person in recovery, or concerned neighbor, local action is essential to sustaining recovery pathways when national support becomes unstable.
Here are community-based strategies that can protect and strengthen addiction recovery systems in the face of federal changes:
🏥 1. Expand Local Treatment Access
- Support low-barrier clinics that provide medication-assisted treatment (MAT), harm reduction services, and peer support.
- Leverage mobile health units and telehealth to reach rural or underserved populations.
- Encourage local governments to fund community health centers, especially those serving uninsured or Medicaid populations.
🤝 2. Strengthen Recovery Support Networks
- Invest in peer recovery programs, which are cost-effective and evidence-based.
- Build or promote recovery community organizations (RCOs) that offer sober housing, employment support, and family programming.
- Collaborate with faith-based and cultural groups to offer inclusive recovery environments.
💬 3. Launch Public Education and Anti-Stigma Campaigns
- Host community forums, workshops, and school talks to reframe addiction as a medical condition, not a moral failure.
- Share real recovery stories to build compassion and awareness.
- Partner with media outlets to combat misinformation about MAT, overdose prevention, and harm reduction.
🧭 4. Create Navigation and Referral Systems
- Develop local resource maps that list available services, eligibility criteria, and contact information.
- Train community health workers or peer navigators to guide individuals through the treatment system.
- Set up a 24/7 helpline or drop-in centers to connect people with immediate care.
🏛️ 5. Advocate for Local Policy and Budget Support
- Attend town halls, budget hearings, and city council meetings to push for recovery-focused spending.
- Support ballot measures that fund mental health and addiction services through local taxes or cannabis revenue.
- Encourage law enforcement and public health to adopt diversion programs instead of incarceration for substance use-related offenses.
🧰 6. Partner Across Sectors
- Create coalitions among schools, hospitals, shelters, courts, and treatment centers to coordinate services.
- Engage businesses in hiring people in recovery and offering workplace support programs.
- Involve universities and researchers in evaluating community programs and tracking outcomes.
📊 7. Monitor Needs and Outcomes
- Collect local data on service demand, gaps, overdose rates, and treatment success.
- Use findings to apply for grants or state funding and demonstrate impact to funders.
- Share success stories and lessons learned to inspire replication in other communities.
In times of federal uncertainty, community action becomes the lifeline for addiction recovery. Through collaboration, innovation, and local leadership, we can build systems that are not only resilient but also more responsive and inclusive than ever before. With the right strategies, recovery doesn’t just survive policy shifts—it thrives despite them.
Frequently Asked Questions
Here are some common questions:
Question: Provide a sample of addiction treatment policy response for health care providers.
Answer: A Checklist for Health Care Providers to help respond effectively to recent changes in addiction treatment policy and ensure continued support for patients with substance use disorders (SUDs):
Addiction Treatment Policy Response Checklist for Health Care Providers
🏥 Clinical Practice
- Integrate screening tools (e.g., SBIRT, COWS) into routine care
- Initiate MOUD (buprenorphine, methadone, naltrexone) when appropriate
- Provide overdose prevention education and distribute naloxone kits
- Use trauma-informed care approaches in addiction treatment
- Refer patients to behavioral health or peer recovery support as needed
👩⚕️ Provider Training & Education
- Complete training on MOUD prescribing and management
- Educate staff on addiction as a chronic disease
- Offer anti-stigma training to clinical and non-clinical staff
- Attend webinars or CME courses on changing addiction policies
🔄 Care Coordination
- Establish referral partnerships with outpatient addiction clinics
- Set up warm handoffs to recovery coaches or social workers
- Build or join a community provider network for SUD care continuity
🧾 Billing and Documentation
- Ensure use of correct CPT codes for SUD services (e.g., 99283 + H0031)
- Document MOUD initiation, counseling, and follow-up accurately
- Track outcomes and readmissions to support reimbursement and grants
📢 Advocacy & Policy Engagement
- Join a professional advocacy organization (e.g., ASAM, APA)
- Participate in public comment periods for health policy changes
- Educate local officials about the value of evidence-based treatment
- Support or propose state or local initiatives to fund addiction care
📊 Resource Management
- Apply for state or foundation grants to fill funding gaps
- Use telehealth to expand treatment access in underserved areas
- Leverage peer support specialists to supplement clinical staff
🧠 Patient & Community Engagement
- Offer education sessions for patients and families about treatment options
- Provide culturally competent care and language access resources
- Encourage patient participation in support groups or recovery coaching
Question: Provide a sample checklist for families and individuals in response to addiction policies
Answer: Checklist flyer for individuals with addiction and their families
Checklist for Families and Individuals in Addiction Recovery
Staying Strong During Changes in Treatment Policies
🧠 Stay Informed
- Know your rights to treatment and insurance coverage
- Learn about local programs offering addiction care
- Follow trusted sources for addiction policy news (e.g., SAMHSA, NIDA, advocacy orgs)
📞 Get Connected
- Join a support group (e.g., SMART Recovery, AA/NA, Al-Anon)
- Connect with a peer recovery coach or counselor
- Build a list of local providers still offering services
🗣️ Speak Up for Your Needs
- Contact local and state officials to protect access to care
- Share your story (safely) to raise awareness and reduce stigma
- Join or support addiction advocacy groups
🤝 Build a Support Network
- Create a list of trusted family/friends for emotional support
- Exchange resources with other families in recovery
- Partner with others to attend meetings or appointments
📋 Plan Ahead
- Prepare an emergency recovery plan (medications, contacts, transportation)
- Ask your provider what happens if services are cut or moved
- Keep a personal health record (treatment history, meds, insurance info)
💬 Fight Stigma with Education
- Learn and share the facts: addiction is a medical condition
- Talk to schools, workplaces, or churches about addiction awareness
- Support others in recovery without judgment
🚨 Track Barriers
- Keep a log of denied services, waitlists, or unaffordable care
- Report problems to state ombudsmen or legal advocates
- Use this data for advocacy and awareness
📢 You are not alone.
Recovery is possible, even when the system is changing. Stay connected. Stay informed. Speak up.
Question: Provide a checklist for community leaders to advocate for additional treatment policies
Answer: Checklist for Community Leaders
Community Leader Advocacy Checklist: Addiction Treatment Policy
🔍 Understand the Policy Landscape
- Stay updated on federal changes affecting addiction treatment (e.g., funding cuts, Medicaid reforms, agency restructuring).
- Identify state-level impacts and their effects on local services and access.
- Review existing local ordinances, budgets, and health department plans tied to addiction treatment.
🗣️ Engage in Public Advocacy
- Attend city council, health board, and school board meetings to advocate for addiction and mental health services.
- Schedule meetings or send letters to local, state, and federal lawmakers to express concerns and policy needs.
- Use media platforms (op-eds, interviews, social media) to raise awareness and drive public support.
💬 Educate and Mobilize the Community
- Host or support community forums, town halls, or webinars on addiction issues and available resources.
- Disseminate fact-based materials about addiction treatment, harm reduction, and recovery.
- Encourage storytelling: uplift lived experiences to humanize the impacts of policy.
🤝 Build Local Partnerships
- Form or join a coalition of stakeholders: healthcare providers, schools, law enforcement, nonprofits, and people in recovery.
- Partner with faith groups, recovery organizations, and peer networks to broaden your advocacy base.
- Collaborate with local media to keep addiction issues in the public eye.
💼 Influence Local Funding Decisions
- Advocate for prioritizing addiction treatment in city and county budgets.
- Promote use of opioid settlement funds, cannabis tax revenue, or crisis response allocations for recovery programs.
- Push for funding of low-barrier services (e.g., MAT, peer support, mobile clinics, naloxone distribution).
🧾 Document Community Needs and Gaps
- Collect data and stories about service shortages, waitlists, or insurance barriers.
- Conduct community needs assessments in collaboration with health departments or universities.
- Use findings to apply for state, private, or philanthropic grants to fill funding gaps.
📢 Support Inclusive and Evidence-Based Policies
- Promote adoption of harm reduction strategies (e.g., syringe exchange, naloxone access).
- Encourage diversion programs and alternatives to incarceration for substance use.
- Advocate for anti-stigma campaigns and trauma-informed care in all public services.
📊 Track Progress and Share Results
- Set measurable goals for community advocacy (e.g., new partnerships, budget wins, expanded services).
- Track outcomes from advocacy efforts and share them with stakeholders.
- Celebrate and publicize community wins to build momentum and morale.
Tip:
Keep this checklist visible at coalition meetings, planning sessions, and community briefings. Update it regularly in response to policy changes and local progress.
Conclusion
As the Trump administration reshapes addiction treatment policy, the road ahead presents both challenges and opportunities. While reduced federal oversight and funding cuts may strain access to care, strong advocacy from healthcare providers, individuals in recovery, and their families can help protect vital services and drive community-centered solutions. By staying informed, speaking out, and building networks of support, stakeholders can influence policy, preserve evidence-based treatment, and ensure that those affected by addiction are not left behind. Together, proactive engagement and resilience will be key to managing these policy changes and safeguarding the future of addiction recovery.
Video: SHOCKING Truth About Funding Cuts in Addiction Recovery