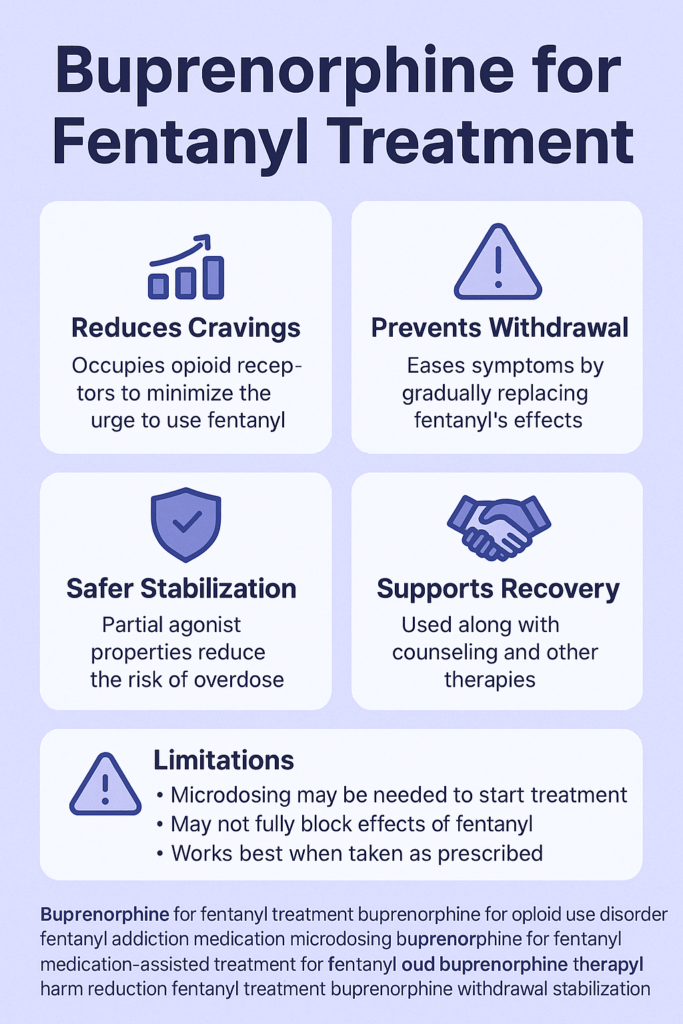
Fentanyl addiction needs higher doses of buprenorphine to treat fentanyl’s potency and manage cravings and withdrawal while reducing overdose risk. Self-management strategies like education, healthy coping, and strong family support for open communication are vital. Community resources, including harm reduction programs and naloxone distribution, promote a safer environment. Together, these efforts form a holistic framework to combat fentanyl addiction and prevent overdose.
Optimizing Buprenorphine Dosing for Preventing Hospitalization in Fentanyl Addiction: A Complex Relationship
In recent years, there has been growing recognition of the challenges posed by fentanyl addiction. As a potent opioid, fentanyl requires a nuanced approach to treatment, particularly when it comes to managing withdrawal symptoms and preventing hospitalization. Emerging research suggests that higher doses of buprenorphine can play a pivotal role in addressing these challenges, but the relationship is complex and influenced by various factors.
1. Buprenorphine Mechanism of Action
Buprenorphine is classified as a partial opioid agonist. Unlike full agonists such as fentanyl, buprenorphine alleviates withdrawal symptoms and cravings without inducing the same level of euphoria or respiratory depression. This unique mechanism helps stabilize individuals in treatment, significantly reducing the risk of relapse and associated complications that could lead to hospitalization.
2. Fentanyl Potency
The potency of fentanyl complicates treatment strategies. Being significantly more potent than traditional opioids, individuals with fentanyl addiction may require higher doses of buprenorphine for effective management. Studies have shown that patients with high levels of opioid use, particularly those dependent on fentanyl, often benefit from doses exceeding 16 mg/day of buprenorphine.
3. Research Findings
Research supports the use of higher doses of buprenorphine. A study published in JAMA Psychiatry indicates that patients on higher doses experience improved retention in treatment and a decrease in overdose and hospitalization rates. This correlation suggests that appropriate dosing can lead to better treatment outcomes for individuals battling opioid use disorder, including those explicitly using fentanyl.
4. Treatment Retention
Improved treatment retention is a critical outcome of higher buprenorphine dosing. Patients who feel their symptoms are well-managed are less likely to discontinue treatment, reducing their risk of relapse and subsequent crises that could necessitate hospitalization. Retention in Medication-Assisted Treatment (MAT) is vital for achieving long-term recovery.
5. Individualized Treatment
It is crucial to individualize buprenorphine dosing based on a patient’s unique circumstances. Factors such as their history of opioid use, addiction severity, co-occurring mental health conditions, and overall health status should be taken into account. Personalizing treatment ensures that individuals receive the appropriate dosage for optimal therapeutic effect.
6. Comprehensive Approach
While higher doses of buprenorphine can reduce hospitalization rates, a comprehensive treatment strategy is essential. Incorporating counseling, psychosocial support, and regular monitoring enhances the likelihood of successful outcomes. Addressing the multifaceted nature of addiction increases the potential for sustained recovery.
7. Potential Risks of High Doses
Despite the benefits, high doses of buprenorphine come with risks. If not appropriately managed, excessively high doses can precipitate withdrawal. Therefore, continuous monitoring and careful dosage adjustments by healthcare providers are imperative to ensure patient safety.
In conclusion, higher doses of buprenorphine can be an effective strategy for preventing hospitalization among individuals with fentanyl addiction. The benefits can be significant when tailored to individual needs and integrated with comprehensive treatment approaches. Ongoing research and clinical practice are essential to refining dosing strategies for buprenorphine, maximizing therapeutic benefits while minimizing risks for those struggling with opioid addiction.
Understanding Buprenorphine: A Complex Mechanism for Managing Cravings and Withdrawal in Opioid Use Disorder
Buprenorphine has emerged as a cornerstone medication for managing cravings and withdrawal symptoms in individuals with opioid use disorder (OUD). Its effectiveness lies in its intricate interactions with the brain’s opioid receptors and various neurochemical pathways. This blog delves into the mechanisms through which buprenorphine alleviates the challenges associated with OUD.
1. Opioid Receptor Interaction
Partial Agonist Activity:
Buprenorphine is classified as a partial agonist at the mu-opioid receptor (MOR). This means it activates these receptors but does so with less intensity than full agonists like morphine or fentanyl. By partially stimulating the MOR, buprenorphine alleviates withdrawal symptoms and cravings while minimizing the euphoric effects that can lead to misuse.
Kappa-Opioid Receptor Antagonism:
Additionally, buprenorphine is a kappa-opioid receptor (KOR) antagonist. Activation of KOR is linked to feelings of dysphoria and anxiety, which can intensify cravings. By blocking KOR, buprenorphine can help stabilize mood and reduce the psychological discomfort that often accompanies opioid withdrawal.
2. Reduction of Withdrawal Symptoms
Stabilization of Neurotransmitter Levels:
Opioid withdrawal results in a marked decrease in endogenous opioid peptides and other key neurotransmitters. By binding to the mu-opioid receptors, buprenorphine helps restore a semblance of balance in neurotransmitter levels. This action alleviates various withdrawal symptoms, including anxiety, irritability, muscle aches, and insomnia.
Gradual Onset of Action:
Buprenorphine has a long half-life, allowing its effects to last longer than many full agonist opioids. This extended duration smooths the withdrawal process, reducing symptoms’ intensity and onset.
3. Craving Reduction
Blocking the Effects of Other Opioids:
When buprenorphine occupies mu-opioid receptors, it can block the euphoric effects of other opioids. This blockage means that if someone relapses and uses another opioid, they are less likely to experience the high, which can help diminish cravings over time.
Increased Dopamine Activity:
Buprenorphine also influences the brain’s reward system by indirectly increasing dopamine levels in regions such as the nucleus accumbens. This modulation of reward pathways can further help reduce cravings and reinforce abstinence by providing a sense of stability and satisfaction without the overdose risks associated with full agonists.
4. Impact on the Stress Response
Regulating the Hypothalamic-Pituitary-Adrenal (HPA) Axis:
Opioid withdrawal can trigger the HPA axis, leading to elevated levels of stress hormones like cortisol. Buprenorphine helps to modulate this response, which can alleviate stress and anxiety related to withdrawal and cravings, further supporting recovery efforts.
5. Neuroplasticity and Long-Term Changes
Facilitating Neuroadaptation:
Chronic opioid use induces neuroadaptive changes within the brain’s circuitry. Buprenorphine can help reverse some of these alterations over time, promoting recovery. This neuroplasticity is vital in assisting individuals to regain control over their cravings and reduce the likelihood of relapse.
Buprenorphine’s efficacy in managing cravings and withdrawal symptoms in individuals with opioid use disorder stems from its complex interactions with opioid receptors, stabilization of neurotransmitter systems, modulation of the brain’s reward pathways, and regulation of the stress response. By partially activating the mu-opioid receptor and blocking the kappa-opioid receptor, buprenorphine offers a multifaceted approach to recovery, aiding individuals on their journey toward sobriety. Understanding these mechanisms can help refine treatment strategies and improve outcomes for those battling opioid addiction.
Navigating Fentanyl Addiction: The Need for Higher Doses of Buprenorphine in Treatment
The rising prevalence of fentanyl addiction poses significant challenges for treatment providers. Due to its high potency and the physiological adaptations that occur with prolonged use, individuals with fentanyl addiction often require higher doses of buprenorphine for effective management. Here’s an in-depth look at the interconnected factors contributing to this need.
1. Potency of Fentanyl
Comparison to Other Opioids:
Fentanyl is estimated to be 50 to 100 times more potent than morphine and approximately 50 times more potent than heroin. This remarkable strength means that individuals using fentanyl often develop a considerable level of opioid tolerance. As a result, a more powerful or more concentrated treatment approach, such as higher doses of buprenorphine, is essential to achieve the desired therapeutic effects.
2. Tolerance Development
Adaptation of the Brain:
Chronic exposure to fentanyl leads to increased tolerance, where the brain and body become accustomed to the drug’s presence. This adaptation necessitates higher doses of any opioid treatment, including buprenorphine, to elicit similar physiological responses and effectively manage withdrawal symptoms.
Withdrawal Severity:
Individuals dependent on fentanyl may experience withdrawal symptoms that are more severe than those associated with less potent opioids. To adequately address these intense symptoms, higher doses of buprenorphine may be required, highlighting the need for a tailored approach to treatment.
3. Pharmacodynamics of Buprenorphine
Partial Agonist Properties:
Buprenorphine acts as a partial agonist at the mu-opioid receptor, meaning it activates the receptor but does not fully replicate the effects of full agonists like fentanyl. Suppose the dose of buprenorphine is not sufficiently high. In that case, individuals may not experience enough relief from cravings and withdrawal symptoms, necessitating higher doses for those accustomed to the more potent effects of fentanyl.
Ceiling Effect:
Buprenorphine has a ceiling effect, whereby increasing the dosage does not lead to a proportional increase in impact after a certain point. For those with high opioid tolerance, this characteristic may result in the requirement for higher doses to counteract the effects of fentanyl effectively.
4. Blocking Opioid Effects
Antagonism of Full Agonists:
An essential goal in treating patients with fentanyl addiction is not just alleviating withdrawal symptoms but also blocking the euphoric effects of fentanyl in the event of relapse. Higher doses of buprenorphine can more effectively occupy mu-opioid receptors, thereby preventing fentanyl from exerting its effects and reducing the likelihood of relapse.
5. Individual Variability
Personalized Treatment Needs:
Responses to buprenorphine can vary significantly among individuals based on factors such as genetics, previous opioid use history, and overall health. Those with a history of fentanyl use may need higher doses to achieve stabilization and symptom relief, underscoring the importance of personalized treatment plans and careful dose titration.
The potency of fentanyl necessitates higher doses of buprenorphine to effectively manage withdrawal symptoms, mitigate cravings, and counteract the potential effects of relapse. The unique properties of buprenorphine as a partial agonist, combined with the development of tolerance in individuals with fentanyl addiction, highlight the critical need for tailored treatment approaches. By personalizing treatment to each patient’s needs, healthcare providers can offer essential support in the recovery journey from fentanyl dependence, enhancing the chances of successful outcomes.
Empowering Self-Management: Strategies for Preventing Fentanyl Addiction and Overdose
Preventing fentanyl addiction and overdose requires a proactive, informed approach. Self-management strategies empower individuals to take charge of their health and make informed choices regarding substance use. Below are effective strategies that can significantly enhance personal safety and well-being.
1. Education and Awareness
Understanding Fentanyl Risks:
Knowledge is power. Please educate yourself about the dangers associated with fentanyl, including its extreme potency and risk of overdose. Understanding that fentanyl is often mixed with other substances can help you make safer decisions.
Recognizing Signs of Overdose:
Familiarize yourself with the signs of a fentanyl overdose, such as slowed or stopped breathing, unresponsiveness, or blue lips and fingernails. This awareness can enable timely intervention during emergencies.
2. Safe Use Practices
Use Medication as Prescribed:
If prescribed opioids, always follow your healthcare provider’s directions precisely. Avoid increasing doses or mixing medications without consulting a medical professional.
Avoid Non-Prescription Use:
Steer clear of using fentanyl or other opioids obtained illegally. Such substances may be contaminated or mixed with other potent drugs, significantly increasing overdose risks.
3. Implementing Harm Reduction Techniques
Carry Naloxone:
Naloxone is a life-saving medication that can reverse opioid overdoses. Always have it on hand if you or someone you know is at risk. Ensure that friends and family know how to use it in an emergency.
Utilize Fentanyl Test Strips:
Fentanyl test strips allow you to check for the presence of fentanyl in drugs before use. This harm reduction strategy can empower individuals to make safer choices about their substance use.
4. Developing Coping Strategies
Healthy Coping Mechanisms:
Explore alternative coping strategies to manage stress, anxiety, and emotional pain. Techniques such as mindfulness, meditation, exercise, and hobbies can provide healthier outlets.
Set Realistic Goals:
Establish achievable goals for reducing substance use or avoiding triggers. Celebrate progress, no matter how small, as each step contributes to overall well-being.
5. Building a Support Network
Connect with Support Groups:
Engage with support groups for individuals in recovery or those affected by substance use disorders. Sharing experiences and strategies can provide encouragement and accountability.
Communicate with Trusted Individuals:
Foster open communication with friends or family members who can offer support and motivation in maintaining sobriety. Having a reliable support system can be instrumental in recovery.
6. Self-monitoring and Reflection
Keep a Journal:
Maintaining a journal can help you track your feelings, substance use patterns, and triggers. This reflection aids in identifying situations that may lead to cravings or relapse.
Identify Triggers:
Recognize personal triggers that prompt cravings for fentanyl or other substances. Develop strategies to cope with or avoid these triggers effectively.
7. Seeking Professional Help
Participate in Counseling:
Engage in individual or group counseling to address underlying issues related to substance use and develop personalized coping strategies.
Consider Medication-Assisted Treatment (MAT):
If struggling with opioid dependence, discuss medication-assisted treatment options with a healthcare provider. MAT can stabilize individuals and reduce cravings for opioids.
8. Implementing Lifestyle Changes
Healthy Lifestyle Choices:
Maintain a healthy lifestyle through balanced nutrition, regular exercise, and adequate sleep. Physical health positively influences mental well-being and can reduce the desire to use substances.
Limit Alcohol and Other Substances:
Be mindful of alcohol and other substance use, as these can increase the risk of opioid overdose and complicate recovery efforts.
9. Emergency Preparedness
Have an Action Plan:
Create an emergency action plan detailing how to respond in case of an overdose, including contacting emergency services and administering naloxone.
Educate Others:
Share your knowledge about overdose prevention and naloxone use with friends, family, or community members. Educating others creates a supportive environment for everyone involved.
Implementing self-management strategies is crucial for preventing fentanyl addiction and overdose among individuals at risk or in recovery. By prioritizing education, safe practices, healthy coping mechanisms, and building a supportive network, individuals can empower themselves to make informed decisions that significantly reduce the likelihood of addiction and overdose. Seeking professional help, maintaining awareness of triggers, and engaging in reflective practices further enhance the effectiveness of these strategies, paving the way for a healthier future.
The Vital Role of Family Support in Preventing Fentanyl Addiction and Overdose
Family support is essential in preventing fentanyl addiction and overdose. By cultivating an informed and supportive atmosphere, families can help their loved ones make healthier choices and build resilience against substance use. Here are several effective strategies that families can implement:
1. Open Communication
Encourage Honest Dialogue:
Establish an environment where family members feel safe discussing their feelings, struggles, and any concerns about substance use. Open communication is crucial for identifying issues early and facilitating collaborative problem-solving.
Discuss Substance Use:
Engage in frank conversations about the dangers of fentanyl and other opioids. Share information about the risks, signs of addiction, and the potential for overdose. Open discussions can demystify the topic and empower family members to speak up.
2. Education and Awareness
Learn About Fentanyl:
Family members should educate themselves about fentanyl’s potency, common forms (like pills and powders), and the risks of mixing it with other substances. This collective knowledge helps everyone in the family better understand the potential dangers.
Recognize Signs of Addiction:
Educate family members about the signs and symptoms of opioid use disorder, including behavioral changes, withdrawal symptoms, and physical indicators. Early identification can lead to timely intervention.
3. Establishing Boundaries
Set Clear Expectations:
Establish family rules regarding substance use, making it clear that illegal drug use is unacceptable. Setting boundaries fosters accountability and helps family members feel secure.
Limit Access:
Securely store or dispose of any prescription medications, particularly opioids, to minimize the risk of misuse. Families should also discuss the importance of not sharing medicines with anyone.
4. Promoting Healthy Coping Mechanisms
Encourage Positive Activities:
Support family members in healthy activities, such as sports, hobbies, volunteering, or creative pursuits. These activities provide alternative coping strategies and foster a sense of belonging.
Model Healthy Behaviors:
Families can lead by example, demonstrating healthy coping strategies for stress and emotional pain. Modeling positive behaviors helps deter substance use and reinforces healthy choices.
5. Building a Supportive Environment
Foster Emotional Support:
Create a supportive home environment where family members feel valued and understood. Encourage expressions of love, support, and validation to strengthen family relationships.
Be Available:
Make time for family members and allow them to share their thoughts and feelings. Active listening helps individuals feel less isolated and more connected to the family.
6. Encouraging Treatment and Resources
Promote Professional Help:
If substance use becomes a concern, encourage family members to seek professional help, such as counseling or therapy. Discussing the benefits of Medication-Assisted Treatment (MAT) can also provide valuable insights.
Connect with Support Groups:
Encourage family involvement in support groups for both those struggling with addiction and their families, such as Nar-Anon or Al-Anon. These groups offer resources and shared experiences that can be instrumental in recovery.
7. Implementing Safety Measures
Carry Naloxone:
If a family member is at risk of opioid overdose, consider obtaining naloxone (Narcan) and educating the entire family on its use. Ensure that everyone knows how to respond effectively in case of an overdose.
Develop an Emergency Plan:
Create a plan outlining steps to take during an overdose or substance use crisis, including whom to contact, such as emergency services. Being prepared can make a significant difference in crises.
8. Promoting Healthy Relationships
Encourage Positive Friendships:
Help family members build connections with positive influences and supportive peers who encourage healthy choices and discourage substance use. A strong social network can be a protective factor against addiction.
Be Involved:
Engage with family members in their social activities to better understand their social circles and provide guidance on choosing supportive friendships.
9. Recognizing and Addressing Underlying Issues
Identify Mental Health Concerns:
Be vigilant about mental health issues that may contribute to substance use, such as depression or anxiety. Addressing these underlying issues can reduce the likelihood of turning to substances as a coping mechanism.
Facilitate Therapy or Counseling:
Encourage family members to engage in therapy if they are struggling with emotional or psychological challenges. Professional support can promote healthier coping strategies.
Family support strategies are crucial for preventing fentanyl addiction and overdose. By fostering open communication, educating family members, establishing boundaries, promoting healthy coping mechanisms, and creating a supportive environment, families can significantly mitigate the risk of addiction. Active involvement and vigilance empower family members to make healthier choices and seek help when needed, laying the groundwork for a healthier and more resilient family dynamic.
Community Strategies for Preventing Fentanyl Addiction and Overdose
Preventing fentanyl addiction and overdose requires a collaborative effort from various community resources. Communities play a crucial role in addressing this critical issue through education, access to treatment, harm reduction programs, and supportive policies. Here are several effective strategies that communities can implement:
1. Education and Awareness Campaigns
Public Awareness Programs:
Develop comprehensive community-wide campaigns to educate residents about the dangers of fentanyl and the risks associated with opioid use. Utilize social media, local news outlets, and community events to disseminate information effectively and reach a broad audience.
School-Based Education:
Implement educational programs in schools to inform students about the risks of substance use, including fentanyl. Engaging students in discussions about addiction, mental health, and coping strategies can foster informed decision-making and resilience.
2. Access to Treatment Services
Expand Treatment Options:
Increase the availability of substance use treatment services, including Medication-Assisted Treatment (MAT) programs, counseling, and support groups. Ensure that these services are accessible, affordable, and tailored to the needs of all community members.
Mobile Treatment Units:
Deploy mobile clinics that provide on-site MAT, counseling, and harm reduction services in underserved areas. This approach helps reach individuals who may not seek help due to transportation or accessibility challenges, making treatment more equitable.
3. Harm Reduction Programs
Syringe Exchange Programs:
Establish syringe exchange programs that provide clean syringes and safe disposal options. These programs reduce the risk of infections and promote safer substance use practices, creating a healthier environment for at-risk people.
Fentanyl Test Strips:
Distribute fentanyl test strips through community organizations, enabling individuals to test their substances for the presence of fentanyl. This harm-reduction strategy empowers people to make safer choices and reduces the likelihood of overdose.
4. Naloxone Distribution and Training
Free Naloxone Distribution:
Provide free access to naloxone (Narcan) through pharmacies, community centers, and health departments. Ensuring that naloxone is available without a prescription increases the community’s capacity to respond to overdoses.
Training Programs:
Offer training sessions for community members on recognizing an overdose and administering naloxone. These programs can empower individuals with the knowledge and skills to act quickly in emergencies.
5. Collaboration with Healthcare Providers
Partnerships with Healthcare Systems:
Collaborate with local healthcare providers to establish protocols for identifying and referring individuals at risk of opioid addiction. Educating healthcare providers about responsible prescribing practices and the importance of MAT can improve outcomes.
Integrating Mental Health Services:
Encourage healthcare facilities to integrate mental health services with addiction treatment. Recognizing the interplay between mental health issues and substance use can lead to more comprehensive and effective care.
6. Support for Families and Caregivers
Family Support Programs:
Create resources and support groups for families affected by addiction. These programs can provide education, coping strategies, and a network of support for those struggling with the impacts of their loved ones’ substance use.
Counseling Services:
Offer counseling and therapy services designed explicitly for families dealing with the challenges of substance use. Helping families navigate these complexities can improve communication and strengthen relationships.
7. Community Engagement and Empowerment
Community Coalitions:
Form coalitions that bring together various stakeholders, including healthcare providers, law enforcement, educators, and community organizations. Collaborating on initiatives allows for a more cohesive and effective response to the opioid crisis.
Engaging Youth:
Involve youth in prevention efforts by providing leadership opportunities and encouraging them to participate in community initiatives aimed at substance use prevention. Empowering young people can create a culture of prevention.
8. Policy Advocacy
Advocate for Policy Changes:
Work with local and state officials to implement policies that enhance access to treatment, support harm reduction strategies, and regulate the prescription of opioids. Strong policies can significantly impact community health.
Funding for Prevention Programs:
Advocate for increased funding for prevention and treatment programs within the community. Ensuring that resources are available is vital for supporting individuals and families affected by fentanyl addiction.
9. Data Collection and Research
Monitor Overdose Trends:
Collect and analyze data on opioid-related overdoses and substance use patterns within the community. This information can inform targeted interventions and help allocate resources effectively.
Research Community Needs:
Conduct community assessments to identify specific needs and barriers to substance use prevention and treatment. Tailored responses can maximize the impact of interventions.
Community resource strategies play a vital role in preventing fentanyl addiction and overdose. By implementing education and awareness campaigns, expanding access to treatment and harm reduction programs, promoting naloxone distribution, and fostering stakeholder collaboration, communities can create supportive environments that empower individuals to make healthier choices. Engaging families, advocating for policy changes, and focusing on data-driven approaches are essential for addressing the complex challenges posed by fentanyl addiction. These strategies can help build stronger, healthier communities, prioritizing prevention and recovery.
Frequently Asked Questions
Here are some common questions:
Does buprenorphine replace one addiction with another?
No. Buprenorphine treats opioid use disorder by stabilizing brain function. It reduces harmful behaviors and improves functioning rather than reinforcing addictive patterns.
How long do people stay on buprenorphine?
Treatment duration varies. Some individuals use buprenorphine short-term, while others benefit from long-term or indefinite treatment. Decisions should be individualized and based on clinical outcomes.
What happens if buprenorphine is stopped too soon?
Stopping buprenorphine prematurely increases the risk of relapse and overdose. Tapering should be gradual and medically supervised.
Can buprenorphine be used during pregnancy?
Yes. Buprenorphine is considered a safe and effective treatment for opioid use disorder during pregnancy and improves outcomes for both parent and baby.
Are there side effects?
Common side effects may include headache, nausea, constipation, or changes in sleep. Most are mild and improve over time.
Conclusion
Addressing fentanyl addiction requires a multifaceted approach that emphasizes the need for higher doses of buprenorphine to counteract the drug’s potency and effectively manage withdrawal symptoms and cravings. Understanding the brain mechanisms involved in opioid addiction is crucial for developing effective treatment strategies. Equally important are self-management techniques that empower individuals to make informed decisions about their recovery. Family support enhances accountability and emotional resilience, while robust community resource strategies—such as harm reduction programs and naloxone distribution—create safer environments for at-risk people. By integrating these elements, we can build a comprehensive framework that not only supports individuals in their recovery journey but also contributes to the broader effort of preventing fentanyl addiction and reducing the incidence of overdose.
Video: Buprenorphine for Fentanyl Addiction Treatment