Bridging therapies for chronic pain offer essential temporary relief, supporting immediate pain management, reducing opioid reliance, and improving patient functionality. However, they come with risks, such as side effects and potential over-reliance. Ethical concerns include balancing patient autonomy with provider responsibility and addressing access disparities. Community resources like education, support services, and integrated care can help mitigate these challenges, emphasizing a comprehensive approach to safe, effective chronic pain management.
Bridging Therapies for Chronic Pain: Temporary Relief for Better Pain Management
Bridging therapies for chronic pain provide temporary relief, helping patients manage pain during transitions between treatments or when primary approaches are being adjusted. These therapies help alleviate pain and improve function until more definitive treatments are available. Here are some standard bridging therapies:
- Medications
- Non-Opioid Analgesics: Over-the-counter options like acetaminophen or NSAIDs can provide immediate relief.
- Adjuvant Medications: Antidepressants like duloxetine or anticonvulsants like gabapentin help manage neuropathic pain and can enhance primary medications.
- Physical Therapy
- Therapeutic Exercises: These strengthen muscles and improve flexibility, supporting pain relief and recovery.
- Manual Therapy: Techniques like massage offer temporary relief and improve mobility.
- Interventional Procedures
- Nerve Blocks: Regional anesthetic injections target specific pain areas for temporary relief.
- Epidural Steroid Injections: These help reduce inflammation and relieve conditions such as sciatica or herniated discs.
- Alternative Therapies
- Acupuncture: This method may reduce pain and improve well-being.
- Chiropractic Care: Manual adjustments relieve musculoskeletal pain and enhance functionality.
- Psychological Interventions
- Cognitive Behavioral Therapy (CBT): CBT equips patients with coping strategies to manage pain-related thoughts and behaviors.
- Mindfulness and Relaxation Techniques: Practices such as meditation and yoga reduce stress and complement pain management.
- Lifestyle Modifications
- Dietary Changes: Anti-inflammatory diets can help reduce pain and support overall health.
- Exercise Programs: Low-impact exercises, like swimming or walking, improve function and help relieve pain.
- Transcutaneous Electrical Nerve Stimulation (TENS)
- TENS Therapy: Electrical impulses disrupt pain signals sent to the brain, providing temporary relief.
- Complementary Therapies
- Massage Therapy: Regular massages alleviate muscle tension and improve circulation.
- Biofeedback: This technique helps patients learn to control physiological responses to pain and stress.
- Pain Management Clinics
- Multidisciplinary Approaches: These clinics provide individualized pain management by combining medical, physical, and psychological therapies.
Bridging therapies are vital tools for chronic pain management. They help patients maintain function and quality of life while awaiting the effects of more lasting treatments.
The Benefits of Bridging Therapies in Chronic Pain Management
Bridging therapies are crucial in chronic pain management, providing support during transitions and enhancing overall well-being. Here are some key benefits these therapies offer:
- Immediate Pain Relief
- Quick Access to Relief: Bridging therapies deliver rapid pain relief, especially valuable during treatment transitions or adjustments.
- Improved Functionality
- Enhanced Daily Activities: These therapies effectively manage pain, helping patients maintain or regain their ability to perform daily tasks, work, and engage socially.
- Reduced Dependence on Opioids
- Minimizing Opioid Use: Bridging therapies offer alternative ways to manage pain, reducing reliance on opioids and lowering the risk of dependence.
- Complementary Approach
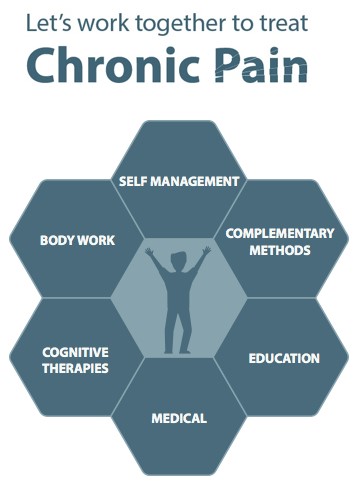
- Holistic Pain Management: Integrating medications, physical therapy, and psychological support provides a multidimensional approach that improves treatment effectiveness.
- Personalized Care
- Tailored Treatment Plans: These therapies are customized to meet individual patient needs, aligning with specific pain conditions, preferences, and responses.
- Support During Treatment Changes
- Smooth Transitions: Bridging therapies help ensure continuity during transitions, such as switching medications, which can help prevent pain flare-ups.
- Psychological Benefits
- Coping Strategies: Psychological interventions such as cognitive-behavioral therapy equip patients with practical coping skills, thereby enhancing emotional resilience.
- Multidisciplinary Collaboration
- Comprehensive Care: Bridging therapies often involve various healthcare professionals working together to deliver coordinated, effective pain management.
- Long-Term Pain Management Skills
- Patient Empowerment: With self-management techniques and lifestyle adjustments, patients gain long-term skills for managing their pain independently.
- Prevention of Chronic Pain Worsening
- Stabilizing Pain Levels: These therapies help maintain stable pain levels, reducing the likelihood of more severe pain conditions developing.
Incorporating bridging therapies into chronic pain management creates a flexible, supportive approach that can improve quality of life and provide essential support for individuals navigating complex treatment plans.
Potential Disadvantages of Bridging Therapies in Chronic Pain Management
While bridging therapies offer valuable support for chronic pain management, they also come with potential drawbacks that patients and healthcare providers should be aware of. Here are some key disadvantages:
- Limited Effectiveness
- Variable Outcomes: The effectiveness of therapies can vary from person to person, and they may not provide relief for every individual or pain type.
- Side Effects
- Adverse Reactions: Medications and interventions in bridging therapies can cause side effects such as nausea or dizziness, which can affect overall quality of life.
- Complexity of Treatment
- Multiple Therapies: Managing various therapies at once can create confusion, making it challenging for patients to follow treatment plans consistently.
- Cost Implications
- Financial Burden: Expenses for medications, therapies, and alternative treatments can add up, and not all are covered by insurance, creating financial strain.
- Time Commitment
- Increased Time Investment: Attending therapy sessions and follow-ups requires significant time, disrupting daily routines and responsibilities.
- Psychological Stress
- Coping with Changes: Switching between treatments can be stressful, leading to anxiety about their effectiveness or potential pain escalation.
- Potential for Misuse
- Risk of Over-Reliance: Immediate relief from some therapies may lead to dependence, which can complicate long-term pain management goals.
- Withdrawal Symptoms
- Transition Issues: Adjusting or discontinuing specific therapies may lead to withdrawal symptoms or pain recurrence, complicating management.
- Inconsistent Quality of Care
- Variable Provider Experience: The quality of bridging therapies can vary with provider expertise, leading to uneven treatment experiences.
- Focus on Symptom Management
- Neglecting Underlying Causes: Bridging therapies often focus on symptom relief rather than addressing the underlying causes of pain, limiting long-term results.
- Potential for Over-Medication
- Dosing Confusion: Managing multiple medications can raise the risk of over-medication or harmful interactions if not closely monitored.
These potential disadvantages underscore the need for a well-rounded, carefully monitored approach to bridging therapies in chronic pain management. Collaborative planning and open communication between patients and healthcare providers are critical to balancing the benefits and limitations of these therapies for effective pain relief.
Ethical Dilemmas in Bridging Therapies for Chronic Pain Management
Bridging therapies can be valuable for managing chronic pain, but they also raise ethical dilemmas for healthcare providers, patients, and the broader community. Here are some key ethical considerations to keep in mind:
- Informed Consent
- Understanding Risks and Benefits: Patients must be thoroughly informed about the potential risks and benefits of bridging therapies. However, explaining complex options can be challenging, especially for patients who feel overwhelmed by their pain.
- Balancing Pain Relief with Risk of Dependence
- Opioid Use: When bridging therapies include opioids, providers face the ethical challenge of balancing effective pain relief with the risk of dependence, highlighting the need to manage addiction risks carefully.
- Patient Autonomy vs. Provider Responsibility
- Respecting Choices: While patients can choose their treatment, providers may feel ethically responsible for limiting therapies they view as potentially harmful or ineffective.
- Equity in Access to Care
- Disparities in Treatment: Unequal access to bridging therapies can exacerbate health disparities, raising ethical concerns about fairness in treatment across populations.
- Short-term vs. Long-term Outcomes
- Focus on Immediate Relief: Prioritizing short-term pain relief can sometimes overshadow long-term management, raising questions about neglecting underlying health issues in pursuit of quick solutions.
- Provider Bias
- Judgment of Pain Experience: Unintentional biases about pain and appropriate treatment may affect provider decisions, leading to disparities in care quality based on subjective rather than objective assessments.
- Integration of Multidisciplinary Approaches
- Collaboration Challenges: Ethical dilemmas can arise when specialists from different fields disagree on the best course of treatment, potentially complicating patient-centered care.
- Potential for Over-treatment
- Risk of Excessive Interventions: Multiple therapies may lead to over-treatment, raising ethical concerns about the appropriateness of care and the potential for harm.
- Quality of Life Considerations
- Impact on Well-being: Decisions about bridging therapies should weigh pain relief and the patient’s quality of life, posing ethical questions about prioritizing health outcomes.
- Withdrawal and Transition Management
- Navigating Changes: Transitioning between therapies poses ethical dilemmas regarding the management of withdrawal symptoms and the maintenance of patient comfort, requiring careful attention to patient welfare.
These ethical considerations emphasize the importance of patient-centered, compassionate care in chronic pain management. Providers should prioritize informed consent, open communication, and collaborative decision-making to effectively address the complexities of bridging therapies.
Enhancing Chronic Pain Management: The Role of Community Resources in Supporting Bridging Therapies
Community resources are essential in supporting bridging therapies for chronic pain, significantly enhancing access to care, education, and support for individuals managing chronic pain. Here are some effective strategies that communities can implement:
- Educational Programs
- Workshops and Seminars: Host community workshops on pain management strategies, including bridging therapies, medication safety, and alternative treatments.
- Resource Guides: Distribute pamphlets and online resources that outline available therapies and local support options.
- Support Groups
- Peer Support Networks: Establish support groups for individuals with chronic pain to share experiences and coping strategies regarding bridging therapies.
- Family Support Programs: These programs provide resources for family members to better understand chronic pain challenges and support their loved ones.
- Access to Healthcare Providers
- Multidisciplinary Clinics: Create community clinics that offer integrated care involving pain specialists, physical therapists, psychologists, and nutritionists to address various aspects of chronic pain.
- Referral Networks: Develop partnerships among local healthcare providers to ensure access to a range of bridging therapy options.
- Alternative and Complementary Therapies
- Community Classes: Offer yoga, tai chi, or mindfulness meditation classes to help manage pain and improve overall well-being.
- Access to Complementary Services: Facilitate access to acupuncture, chiropractic care, and massage therapy as part of a holistic pain management approach.
- Pain Management Resources
- Information Centers: Set up community resource centers where individuals can learn about pain management options, including medications and non-drug therapies.
- Online Platforms: Develop websites or apps that provide information about local resources and support services for chronic pain management.
- Prescription Monitoring Programs (PMPs)
- Community Awareness: Educate providers and patients about the importance of PMPs in preventing misuse and ensuring safe medication management.
- Collaboration with Pharmacies: Partner with local pharmacies to promote safe prescribing practices and responsible medication use.
- Advocacy and Policy Initiatives
- Community Advocacy Groups: Establish groups to advocate for policies that improve access to pain management services and bridging therapies.
- Public Awareness Campaigns: Launch campaigns to raise awareness about chronic pain and effective management strategies, including bridging therapies.
- Research and Collaboration
- Partnerships with Universities: Collaborate with academic institutions to conduct research on effective pain management strategies and evaluate the outcomes of bridging therapies.
- Data Collection and Sharing: Gather and share data on community needs related to chronic pain to inform resource allocation and program development.
- Crisis Intervention Services
- Hotlines and Helplines: Provide access to confidential helplines for individuals seeking support related to chronic pain and bridging therapy options.
- Mobile Outreach Teams: Develop teams offering in-person support and resources for individuals experiencing pain crises.
- Evaluation and Feedback Mechanisms
- Community Surveys: Regularly assess community needs and the effectiveness of available resources to ensure that bridging therapies align with patient needs.
- Feedback Loops: Establish channels for patients and providers to share feedback on the effectiveness of community resources, leading to continuous improvement.
By implementing these community resource strategies, local organizations can create a supportive environment that enhances the effectiveness of bridging therapies for chronic pain. This ultimately leads to improved patient outcomes and quality of life for patients with chronic pain.
Conclusion
Bridging therapies for chronic pain represent a crucial component of pain management, offering immediate relief and reducing reliance on opioids while enhancing overall functionality. Despite their benefits, these therapies have disadvantages, including potential side effects and ethical dilemmas regarding patient autonomy and access to care. Addressing these challenges requires robust community resource strategies that provide education, support, and integrated care options, empowering patients to navigate their pain management effectively. Ultimately, a comprehensive approach that balances the advantages and disadvantages of bridging therapies can lead to improved outcomes and a better quality of life for individuals living with chronic pain.
Video: 5 Simple Ways to Reduce Chronic Pain While Waiting for Treatment