The new treatment paradigm targeting brain circuitry in substance use disorders reflects a shift toward addressing addiction as a brain-based condition. It is driven by the need for more effective, precise interventions amid rising overdoses and the limits of traditional care. While promising, this approach faces challenges, including high costs, limited access, and ethical concerns about consent, identity, and equity. Government compliance through regulation, funding, and oversight is essential to ensure safe, fair, and practical implementation.
Rewiring Recovery: A Brain-Circuit-Based Approach to Substance Use Disorder Treatment
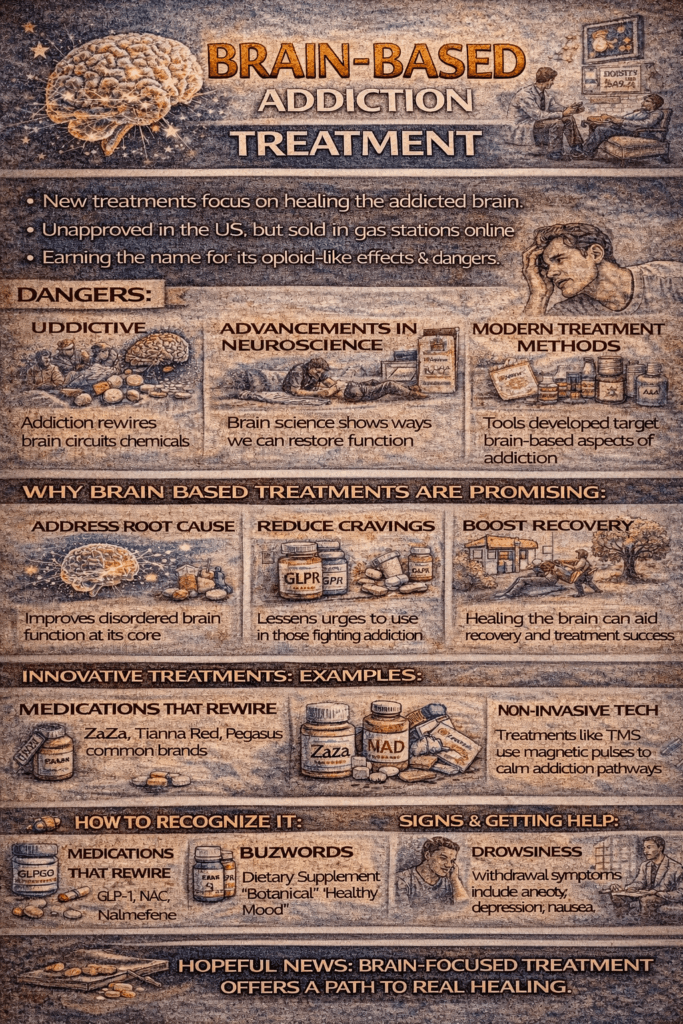
The new treatment paradigm for Substance Use Disorders (SUDs) is moving beyond symptom management to address the root cause—disrupted brain circuitry. This neuroscience-informed model targets specific neural networks involved in reward, motivation, decision-making, and self-regulation. Instead of focusing solely on withdrawal or behavioral symptoms, the goal is to restore healthy brain function. Here are the key components:
🧠 Key Brain Circuits Targeted in SUD Treatment
- Reward Circuitry (Mesolimbic Dopamine Pathway)
- Disrupted by: Drugs that hijack dopamine (e.g., opioids, cocaine)
- Treatment goal: Normalize reward sensitivity and reduce cravings
- Prefrontal Cortex (Executive Control)
- Disrupted by: Impaired decision-making and impulse control
- Treatment goal: Strengthen self-regulation and future planning
- Stress and Emotion Regulation Circuits (Amygdala, HPA Axis)
- Disrupted by: Heightened stress response and emotional triggers
- Treatment goal: Improve stress coping and reduce relapse risk
- Interoception and Craving Awareness (Insula)
- Disrupted by: Poor awareness of internal bodily states
- Treatment goal: Enhance body awareness to curb compulsive use
🧪 Emerging Treatments Based on Brain Circuitry
1️⃣ Neuromodulation Therapies
- Transcranial Magnetic Stimulation (TMS): FDA-cleared for smoking; targets the prefrontal cortex to reduce cravings and improve control
- tDCS and Deep Brain Stimulation (DBS): Experimental approaches modulating reward and impulse-control areas
2️⃣ Pharmacological Innovations
- GLP-1 receptor agonists (e.g., semaglutide): Originally for diabetes, now explored for reducing cravings via dopamine/motivation circuits
- Orexin receptor antagonists: Target arousal and drug-seeking via hypothalamic pathways
- Kappa opioid receptor antagonists: Designed to minimize dysphoria and stress-induced relapse
3️⃣ Cognitive and Mindfulness-Based Therapies
- Cognitive Behavioral Therapy (CBT): Retrains maladaptive thought patterns
- Mindfulness-Based Relapse Prevention (MBRP): Strengthens emotion regulation and body awareness
- Cognitive remediation: Rebuilds attention and flexibility impaired by long-term use
4️⃣ Digital Neurotherapies
- App-based cognitive training and VR environments: Strengthen executive functions, simulate real-life triggers in safe settings
🔄 The Paradigm Shift: From Symptom to Circuit
- Old Model: Treat symptoms (withdrawal, behavior)
- New Model: Target neural circuits using personalized, multi-modal interventions
📈 What This Means for the Future
- More precision treatments tailored to individual brain profiles
- Use of brain imaging and biomarkers to track progress
- Greater integration of behavioral, digital, pharmacologic, and neuromodulatory tools for comprehensive care
This shift offers hope for more effective and enduring recovery by aligning treatment with the neuroscience of addiction. The brain can change—so can the future of recovery.
Challenges of the Brain-Based Approach in Addiction Treatment: What We Must Consider
While the emerging treatment paradigm focused on brain circuitry in Substance Use Disorders (SUDs) offers exciting advancements, it also introduces significant challenges that require thoughtful consideration. As neuroscience continues to shape the future of addiction care, it’s essential to address the barriers, risks, and limitations of this evolving model.
⚠️ 1. Limited Accessibility and High Costs
- Advanced treatments such as Transcranial Magnetic Stimulation (TMS), Deep Brain Stimulation (DBS), or GLP-1 receptor agonists can be prohibitively expensive and are often unavailable in rural or underserved areas.
- Insurance coverage is inconsistent, making it difficult for many patients to access these cutting-edge therapies.
⚠️ 2. Limited Long-Term Research
- Many brain-based interventions remain in the early research phases, especially in addiction applications.
- We still lack solid evidence on their long-term safety, effectiveness, and relapse-prevention outcomes.
⚠️ 3. Not One-Size-Fits-All
- Brain circuitry is highly individualized. A treatment effective for one person may not work for another due to differences in neurobiology, trauma history, substance use patterns, and co-occurring mental health conditions.
- While precision medicine is the goal, the healthcare system currently lacks the infrastructure for truly personalized, neuroscience-informed care.
⚠️ 4. Ethical and Privacy Concerns
- The use of brain imaging and neural biomarkers introduces privacy risks—raising concerns about data misuse, labeling, or discrimination.
- Neuromodulation and brain-targeting drugs present ethical dilemmas, including issues of consent, identity, and personal autonomy. Are we treating a disorder or fundamentally altering the self?
⚠️ 5. Risk of Overmedicalization
- A purely neurobiological approach may neglect the decisive role of social, psychological, and environmental factors—such as trauma, poverty, stigma, and unstable housing.
- There’s a growing concern that we might shift toward tech-centered or pharmaceutical quick-fixes, marginalizing human-centered, community-based, and holistic approaches.
⚠️ 6. Lack of Provider Training
- Most addiction care providers have limited training in brain circuitry and neuroscience-based interventions.
- This can lead to misapplication, overpromising results, or underutilizing valuable tools due to a lack of knowledge or confidence.
In summary, the brain-circuit-based model represents a promising frontier in addiction treatment, but it is not without its limitations and risks. Equity of access, provider training, long-term efficacy, and ethical use must be addressed to ensure these innovations complement rather than replace the vital social, psychological, and community-driven aspects of recovery.
To truly transform addiction care, we must embrace an integrated model—where neuroscience meets compassion, and where cutting-edge technology enhances, not replaces, the human experience of healing.
Ethical Dilemmas in Brain-Based Addiction Treatment: Balancing Innovation with Integrity
The new treatment paradigm targeting brain circuitry in substance use disorders (SUDs) presents several ethical dilemmas, as it shifts focus from behavior and environment to neurological function. While this approach offers new hope, it also raises complex questions about consent, identity, equity, and the role of neuroscience in recovery.
⚖️ Key Ethical Dilemmas
🧠 1. Autonomy and Consent
- Invasive treatments like deep brain stimulation (DBS) or neuromodulation (e.g., TMS) may alter brain activity in ways the individual doesn’t fully understand.
- People with active SUDs may experience impaired decision-making—raising concerns about their capacity to give informed consent for experimental or high-risk treatments.
🧍♂️ 2. Identity and Authenticity
- Interventions that directly affect the brain’s reward or decision-making circuits may raise existential questions:
Is recovery truly “mine” if my brain was rewired to choose it? - There’s concern that brain-targeted treatments could change core aspects of personality or motivation.
⚖️ 3. Equity and Access
- Many emerging treatments (e.g., GLP-1 agonists, neuroimaging-guided care, digital neurotherapies) are expensive and not equitably accessible, potentially increasing health disparities.
- Prioritizing neurobiological models could divert funding and attention away from community-based, culturally informed, and trauma-informed care.
🔍 4. Overmedicalization and Reductionism
- Treating addiction purely as a brain disease may ignore social determinants such as poverty, racism, housing instability, or trauma.
- Risk of over-relying on drugs or devices while underinvesting in human connection, psychotherapy, or recovery support networks.
🧬 5. Use of Brain Data and Privacy
- Brain imaging, biomarkers, and digital cognitive tools can generate sensitive data.
- Raises concerns about data misuse, surveillance, or labeling individuals as “high risk” without consent.
🚨 6. Coercion and Criminal Justice Use
- As neuroscience-informed tools become more widespread, there’s concern they could be used coercively—for example, as a court-ordered treatment or as a condition of parole, without full voluntary participation.
💡 Ethical Oversight Needed
Treatment innovations must be paired with robust ethical guidelines that protect patients’ rights, ensure transparency, and promote equity, autonomy, and dignity in all aspects of care.
Government Compliance in Brain-Based Addiction Treatment: Policies for Ethical and Equitable Integration
As the treatment of Substance Use Disorders (SUDs) evolves to target disrupted brain circuitry, government agencies must adapt their regulatory, funding, ethical, and public health frameworks to support innovation while safeguarding patient rights and ensuring equitable access. Here’s an overview of what’s required—and what’s already underway—to align policy with this neuroscience-driven treatment paradigm.
🏛 1. Regulatory Oversight (FDA & NIH)
- The FDA (U.S. Food and Drug Administration) must review and approve new treatments, such as neuromodulation devices (e.g., TMS, DBS) and medications (e.g., GLP-1 receptor agonists), intended for addiction, not just other medical conditions.
- Example: TMS is FDA-cleared for smoking cessation.
- New compounds for SUDs require Investigational New Drug (IND) applications.
- The NIH (National Institutes of Health)—mainly through NIDA (National Institute on Drug Abuse)—provides scientific guidance and research funding.
- The HEAL Initiative (Helping to End Addiction Long-Term) actively supports the development of circuit-based therapies for addiction.
💼 2. Insurance and Reimbursement Policy
Government programs such as Medicare and Medicaid must adapt policies to cover these emerging treatments. This includes:
- Evaluating whether new interventions are medically necessary and reimbursable
- Updating ICD/DSM coding and aligning with evidence-based practice standards
- Expanding coverage for treatments like GLP-1 agonists, TMS, or digital neurotherapies when used for addiction—not just diabetes or depression
⚖️ 3. Ethical and Legal Safeguards
- All brain-based interventions must comply with informed consent laws, particularly when:
- Altering brain function directly (e.g., via DBS)
- Collecting sensitive neural or cognitive data
- Institutional Review Boards (IRBs) and bioethics committees are essential in reviewing trials and new treatment applications.
- Governments must ensure:
- No coercive use of these treatments (e.g., as court-mandated interventions)
- Respect for patient privacy, autonomy, and choice
🌍 4. Equity and Public Health Mandates
To prevent widening disparities in care, governments should:
- Fund community-based pilot programs to introduce these therapies in underserved and rural areas
- Provide technical assistance and grants to support culturally competent and trauma-informed implementation
- Ensure brain-circuit-based approaches are embedded in public health systems, such as state-funded rehab or harm reduction services
📊 5. Data, Quality Monitoring & Outcome Reporting
Oversight agencies like SAMHSA and CMS must:
- Create clinical quality measures to track the safety and effectiveness of brain-based treatments
- Include neurobiological treatment outcomes in national performance metrics, surveillance systems, and health equity reports
- Standardize data collection for brain-targeted interventions to improve transparency and accountability
In summary, to ensure full government compliance with the emerging brain-based SUD treatment model, policymakers and public agencies must:
- ✅ Approve and regulate innovative therapies via the FDA and NIH
- ✅ Uphold ethical and legal protections for individuals receiving brain-targeted care
- ✅ Ensure coverage through Medicaid, Medicare, and other public insurers
- ✅ Prioritize health equity and culturally informed implementation
- ✅ Develop robust monitoring systems and outcome reporting frameworks
By aligning neuroscience with responsible public policy, governments can ensure that brain-based innovations in addiction care are safe, ethical, and accessible to all—not just the privileged few.
Frequently Asked Questions
Here are some common questions:
Question: What are the potential side effects of using brain-based addiction treatments?
Answer: Brain-based addiction treatments—while promising—can come with a range of potential side effects depending on the type of intervention used. These treatments include neuromodulation (like TMS or DBS), pharmacological agents (such as GLP-1 agonists or orexin antagonists), cognitive therapies, and digital neurotherapies. Below is a breakdown of potential side effects by treatment category:
🧠 1. Neuromodulation Therapies
Examples: Transcranial Magnetic Stimulation (TMS), Deep Brain Stimulation (DBS), transcranial Direct Current Stimulation (tDCS)
Potential Side Effects:
- TMS:
- Headaches (most common)
- Scalp discomfort or tingling
- Dizziness or lightheadedness
- Rare: Seizures, especially in those with epilepsy or neurological vulnerabilities
- DBS (invasive):
- Surgical risks: infection, bleeding, hardware malfunction
- Mood changes (e.g., depression, anxiety, impulsivity)
- Speech or cognitive disturbances
- Personality or behavior alterations
💊 2. Pharmacological Brain-Targeting Agents
Examples:
- GLP-1 receptor agonists (e.g., semaglutide, liraglutide)
- Orexin receptor antagonists
- Kappa opioid receptor antagonists
Potential Side Effects:
- GLP-1 Agonists:
- Nausea, vomiting, constipation
- Appetite suppression (could lead to unhealthy weight loss)
- Pancreatitis (rare)
- Fatigue or dizziness
- Orexin Antagonists:
- Daytime sleepiness or sedation
- Vivid dreams or nightmares
- Possible dependency in long-term use
- Kappa Antagonists:
- Under investigation, but potential effects on mood, emotion regulation, and hormonal balance
🧘 3. Cognitive and Mindfulness-Based Interventions
Examples: CBT (Cognitive Behavioral Therapy), MBRP (Mindfulness-Based Relapse Prevention), cognitive remediation
Potential Side Effects:
- Emotional discomfort when confronting painful memories or trauma
- Increased anxiety or distress early in treatment
- Frustration or fatigue from intensive cognitive retraining
⚠️ While these effects are usually temporary, they can discourage continuation if not managed with proper support.
📱 4. Digital Neurotherapies
Examples: App-based cognitive training, VR simulations, digital CBT platforms
Potential Side Effects:
- Eye strain, motion sickness (especially with VR)
- Overstimulation or fatigue with extended use
- Data privacy concerns (not a physical side effect but a significant risk)
- Emotional discomfort when exposed to triggering simulations
🧩 Cross-Cutting Risks
- Over-reliance on brain-based tools may unintentionally:
- Displace essential social or psychological supports
- Minimize patient agency or identity
- Ethical risks: Misuse of sensitive brain data, coercive use (e.g., in criminal justice settings), or using treatments without proper informed consent
✅ Conclusion
Brain-based addiction treatments show great potential—but must be administered with care. Individual risk varies depending on:
- Type of treatment
- Co-occurring conditions
- Medical history
- Support systems are in place
A comprehensive, person-centered approach that combines neuroscience with psychological, social, and ethical considerations can help minimize risks and enhance safety.
Question: What is the cost of the brain-based addiction medication?
Answer: The cost of brain-based addiction medications can vary widely depending on the type of drug, insurance coverage, country, and indication for use. Many of these medications are still being studied for substance use disorders (SUDs), so off-label use can further complicate pricing and coverage. Below is a breakdown of typical costs (U.S.-based estimates unless otherwise noted) for some of the key medications currently being explored in this space:
💊 1. GLP-1 Receptor Agonists
Examples: Semaglutide (Ozempic, Wegovy), Liraglutide (Saxenda, Victoza)
- Retail Price (without insurance):
- Semaglutide (Ozempic/Wegovy): $900–$1,400/month
- Liraglutide (Saxenda): ~$1,350/month
- Notes:
- These are FDA-approved for diabetes or obesity, not yet for addiction.
- If prescribed off-label for addiction, insurance is unlikely to cover it.
- Generic versions are not yet available (as of 2025).
🧠 2. Orexin Receptor Antagonists
Examples: Suvorexant (Belsomra), Lemborexant (Dayvigo)
- Retail Price:
- Suvorexant: ~$300–$400/month
- Lemborexant: ~$300/month
- Notes:
- Currently approved for insomnia, with off-label investigation for addiction.
- Insurance may cover it if prescribed for sleep, but not for SUDs.
😔 3. Kappa Opioid Receptor Antagonists (Experimental)
Examples: Aticaprant, CERC-501 (not yet approved for public use)
- Retail Price:
- Not available commercially yet (still in clinical trials)
- Notes:
- Maybe free for trial participants
- Commercial costs will depend on the manufacturer and the FDA indication, if approved
🧩 4. Older Medications With Brain-Circuit Targets
Sometimes considered in brain-based models of care
| Medication | Used For | Typical Cost (Uninsured) |
|---|---|---|
| Bupropion (Wellbutrin) | Nicotine, depression | ~$30–$150/month (generic available) |
| Naltrexone (oral) | Alcohol, opioids | ~$100–$300/month |
| Naltrexone (Vivitrol, injectable) | Monthly injection | ~$1,300–$1,600/month |
- Insurance Coverage:
- Often covered when used for FDA-approved addiction indications
- Injectable forms are much more expensive and less likely to be covered for off-label use
🔍 Factors That Influence Cost:
- Insurance status (private, Medicaid, Medicare)
- Indication (FDA-approved vs. off-label)
- Pharmacy discounts (GoodRx, discount cards)
- Patient assistance programs from pharmaceutical companies
- Access to clinical trials or low-cost public health pilots
✅ Summary Table: Brain-Based Addiction Medications (U.S. Prices)
| Drug Category | Examples | Est. Monthly Cost | FDA-Approved for Addiction? |
|---|---|---|---|
| GLP-1 Receptor Agonists | Ozempic, Wegovy, Saxenda | $900–$1,400+ | ❌ (under investigation) |
| Orexin Receptor Antagonists | Belsomra, Dayvigo | ~$300–$400 | ❌ (off-label) |
| Kappa Opioid Antagonists | Aticaprant, CERC-501 | Not available | ❌ (clinical trials) |
| Traditional SUD Medications | Naltrexone, Bupropion | $30–$300+ | ✅ |
Question: How can the medications be equally available to all individuals with addiction?
Answer: Making brain-based addiction medications equally available to all individuals—regardless of income, race, location, or insurance status—requires a multi-level approach involving policy reform, funding, public health equity efforts, and clinical system change. Here are key strategies to achieve equitable access:
🔑 1. Expand Public Insurance Coverage
- Mandate Medicaid & Medicare coverage for evidence-based addiction medications, including emerging brain-targeted drugs like GLP-1 agonists when supported by research.
- Ensure private insurers comply with mental health and substance use parity laws (e.g., the MHPAEA).
- Reimburse off-label use when supported by clinical trial data or expert consensus (e.g., GLP-1 for addiction).
✅ Why it matters: Medicaid covers a large portion of low-income individuals with SUDs. Consistent coverage helps eliminate financial barriers.
💰 2. Create Sliding-Scale and Free Medication Programs
- Establish federal or state-funded voucher programs for low-income or uninsured individuals.
- Require pharmaceutical companies to offer discounted or donated medications through patient assistance programs (PAPs) and community health centers.
- Integrate medication access into opioid settlement fund spending or HEAL Initiative grants.
✅ Why it matters: Many newer treatments are prohibitively expensive without insurance, especially injectables or specialty drugs.
🏥 3. Increase Access in Underserved Communities
- Fund and equip community-based clinics, tribal health centers, and rural health systems to offer brain-based treatments.
- Offer telehealth prescribing for medications that don’t require in-person administration (e.g., GLP-1 injections).
- Expand mobile health units and street medicine models to deliver medications to people who are unhoused or in remote areas.
✅ Why it matters: Geographic isolation or lack of local specialists should not block access to life-saving care.
🧑🏽⚕️ 4. Train More Providers in Neuroscience-Based Addiction Care
- Offer incentives for providers (e.g., loan forgiveness, continuing education credits) to become trained in prescribing and managing brain-targeting medications.
- Integrate this training into nursing, medical, pharmacy, and behavioral health education.
- Promote interdisciplinary teams that include addiction specialists, primary care, psychiatrists, and community workers.
✅ Why it matters: Many clinicians aren’t trained in these new medications, which limits patient access even when drugs are available.
⚖️ 5. Address Racial and Social Inequities in Access
- Fund equity audits and collect disaggregated data to monitor racial, ethnic, and income-based disparities in medication access and outcomes.
- Require culturally competent care and eliminate referral practices that exclude specific populations (e.g., based on housing status, criminal record, or sobriety requirements).
- Include people with lived experience in the design and evaluation of new treatment programs.
✅ Why it matters: Black, Indigenous, and people of color (BIPOC) often face greater barriers to treatment despite equal or higher need.
📊 6. Build Accountability into Public Health Systems
- Require states and treatment programs receiving public funding to report on equitable access to medications.
- Include medication access metrics in the SAMHSA block grant performance requirements.
- Use outcome-based funding models that reward retention and engagement, not just abstinence.
✅ Why it matters: Systems tend to change what they are measured on and funded to improve.
🌍 7. Global Perspective (If Applicable)
For low- and middle-income countries:
- Support international public-private partnerships (e.g., GAVI or Global Fund models) to improve access to addiction medication.
- Ensure intellectual property reform or generic licensing to lower the costs of newer brain-based medications.
✅ In Summary: How to Make Brain-Based Addiction Medications Equally Available
| Strategy | Impact |
|---|---|
| Expand Medicaid/insurance coverage | Reduces cost barriers |
| Subsidize through PAPs and vouchers | Increases affordability |
| Build access in rural/underserved areas | Reaches isolated populations |
| Train providers in neuroscience-informed care | Improves prescribing rates |
| Address racial and social disparities | Promotes fairness |
| Monitor equity in health systems | Ensures accountability |
Conclusion
Targeting brain circuitry in the treatment of substance use disorders offers a promising path toward more effective and personalized care. This paradigm responds to the urgent need for solutions that address the neurological roots of addiction, especially as traditional approaches often fall short. However, its implementation brings challenges, including cost, access, ethical dilemmas, and the risk of overmedicalization. To ensure these innovations benefit all individuals fairly and safely, strong government oversight, ethical safeguards, and equitable access must be built into every stage of development and delivery.
Video: How Treatment Actually Fixes Your Addicted Brain #neuroscience #healing