Opioid overdoses are life-threatening, but understanding how antidotes work can make a crucial difference. This guide explains which antidotes to use, when to administer them, and how to access them quickly, empowering you to respond effectively and protect the lives of loved ones and your community.
What Is the Antidote for Opioid Overdoses?
The main antidote for opioid overdoses is a medication called naloxone. Most people know it by brand names like Narcan or Kloxxado. Naloxone works by blocking the effects of opioids, basically “reversing” the dangerous slowdown in breathing that overdose causes. It’s fast-acting and doesn’t require special training, which is handy in emergencies.
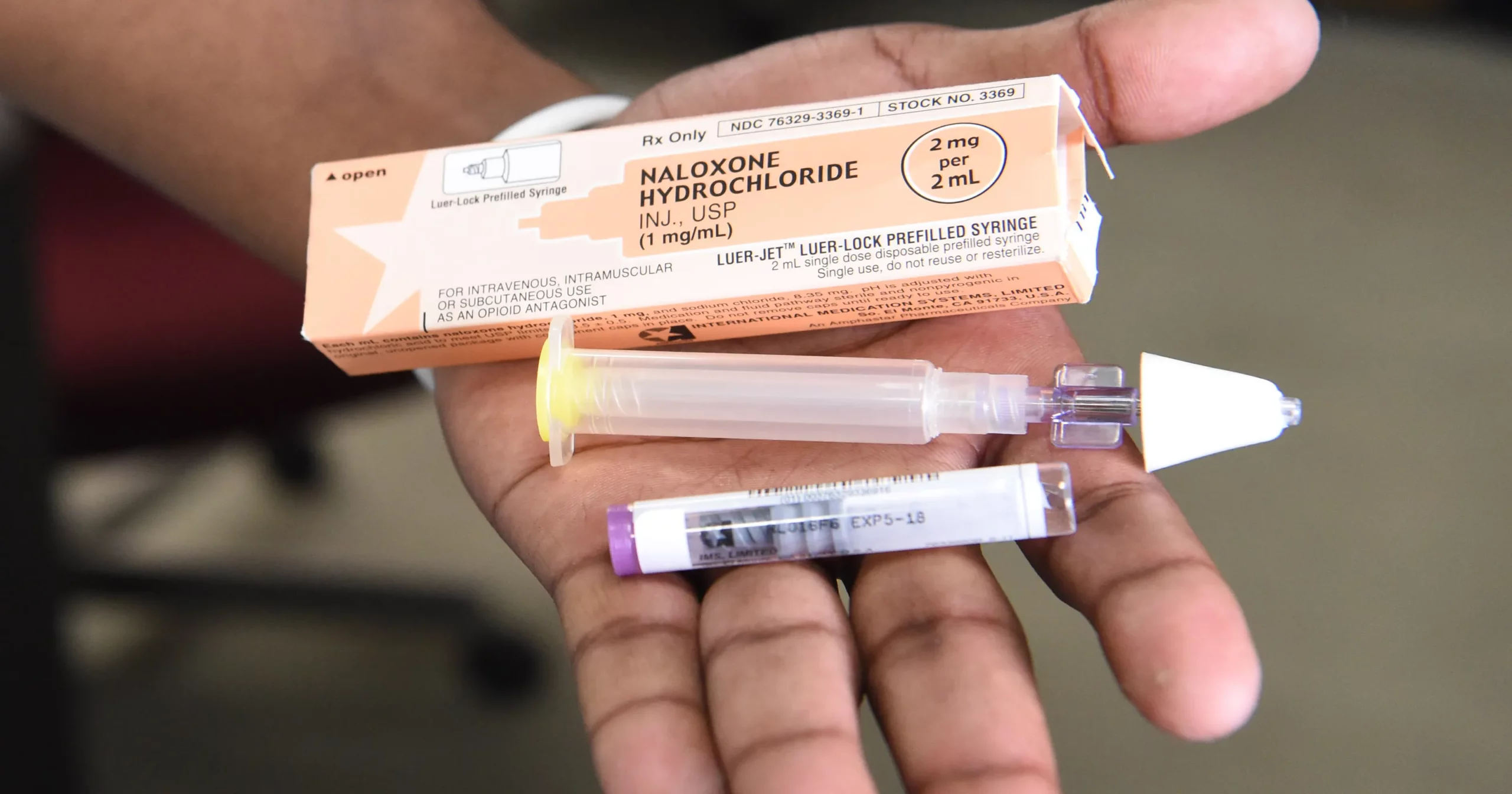
I’ve found that naloxone can come as either a nasal spray or an injection (autoinjector), both designed for quick and easy use, even for folks who aren’t medical professionals. The nasal spray is especially popular because you spray it up the nose—no needles needed, making it accessible and less intimidating.
According to the Centers for Disease Control and Prevention (CDC), naloxone can revive someone within minutes, buying precious time for professional help.
Getting Started: Recognizing and Responding to an Opioid Overdose
Spotting an opioid overdose early is really important. Common signs to watch for include slow, shallow breathing, lips or fingernails turning blue or gray, pinpoint pupils (tiny black dots for pupils), a very limp body, and being unresponsive or unconscious.
If I ever see someone showing these signs and suspect an opioid overdose, I know my first move should be to call 911. Emergency services are trained for these situations. While waiting, using naloxone can stop things from getting worse.
- Check for responsiveness: Try to wake them by shouting or rubbing the breastbone.
- Call for help: Dial 911, even if naloxone is nearby—medical backup is super important.
- Administer naloxone: Use the nasal spray or autoinjector according to the package instructions.
- Support their breathing: If you know how, provide rescue breaths or CPR while you wait for help.
- Stay with the person: They might stop breathing again after the first dose, so hang tight and give more naloxone if there’s no improvement in a few minutes.
How Naloxone Works and Why It Matters
Naloxone latches onto the same brain receptors that opioids target but kicks the opioids off, basically waking the person back up and getting their breathing going again. The effect starts within two to three minutes. Still, it doesn’t last long (usually 30 to 90 minutes). Sometimes, if the opioid overdose is severe or involves more potent drugs like fentanyl, more than one naloxone dose might be needed.
The thing I find most reassuring is that naloxone is very safe. If someone accidentally gets a dose and they aren’t experiencing an opioid overdose, there’s no harmful effect. You can’t get high from naloxone, and it’s not addictive. That’s a big deal as it means anyone can carry and use it without worrying about worsening things.
The National Harm Reduction Coalition has a brilliant breakdown if you want to nerd out on the science of how naloxone works in the brain.
Naloxone Accessibility: Who Needs It and Where to Get It
Naloxone is recommended for anyone who uses opioids or lives with someone who does. This isn’t just for people with a prescription for painkillers; it’s relevant for anyone at risk of overdose, whether from prescription drugs or street opioids like heroin or fentanyl.
A ton of community programs now distribute naloxone kits for free. Pharmacies in many areas also offer it without a prescription. I’ve heard of some states that let you buy naloxone right over the counter, just like allergy meds. Some insurance plans even cover the cost.
- Pharmacies: Ask the pharmacist if they stock Narcan or other naloxone products. Some places keep it behind the counter but will hand it to anyone who checks in.
- Community groups: Organizations focused on harm reduction or public health often hold naloxone training sessions and give away kits.
- Healthcare providers: Many doctors now write naloxone prescriptions for patients who use opioids, and some include it with opioid painkiller prescriptions as a precaution.
Carrying naloxone doesn’t mean you expect an overdose; it just means you’re prepared. It’s sort of like holding a first aid kit or an EpiPen.
Essential Things to Consider Before Using Naloxone
Even though naloxone is easy to use, there are a few things I always keep in mind:
- Shelf Life: Naloxone works best when it’s in date. Check expiration dates regularly and swap out old kits.
- Storage: Store naloxone in a cool, dry place. Extreme heat or cold can make it less effective.
- Side Effects: When naloxone kicks in, some people might get thrown into withdrawal symptoms fast, which can be rough. Nausea, vomiting, sweating, and agitation happen. It’s uncomfortable, but way better than not breathing!
- Aftercare: Even if someone wakes up after naloxone, they still need medical care. Opioids can outlast naloxone in the body so that symptoms can come back.
- Legal Protection: Most states have “Good Samaritan” laws that protect people who use naloxone in an emergency from legal trouble. For local laws, check out Safe Project or your state health department’s site.
Shelf Life and Storage
Naloxone doesn’t need refrigeration, but it hates direct sunlight or being left in a hot car. I check my kit every few months and replace expired doses. Some community programs offer reminders or swaps for expired kits, so it’s worth checking around.
Withdrawal Symptoms
When naloxone works, a person might feel instant withdrawal. That’s unpleasant, but it’s a sign it’s doing its job. Most withdrawal symptoms are short-lived and less dangerous than not getting enough oxygen.
Going Further: Advanced Naloxone Tips and Harm Reduction Strategies
Once you’ve got the basics of naloxone down, there are simple ways to keep building your readiness. Here’s how I go beyond just carrying a kit:
Practice the steps: Try a training session or watch a demo video to reduce your nerves if the real thing happens.
Let people know: Tell friends, family, and roommates where you keep your kit. In an emergency, you might not be the one giving it.
Reduce overdose risk: Learn about mixing drugs, like taking opioids and benzodiazepines together, which raises the risk of overdose. If this applies to you or someone you know, being extra careful matters.
Stay with the person: After giving naloxone, watch out and give another dose if there’s no improvement in a few minutes. Breathing can stop again because opioids can linger longer in the body than naloxone does.
Community groups often offer free classes, which I found helpful for practicing what to do and building confidence. Sites like NEXT Distro make it easy to get information and even supply mail-order naloxone in some locations.
Another important tip is to keep a checklist or card in your wallet with step-by-step naloxone instructions. In an emergency, things move quickly, and clear written steps can make you feel more confident. Also, encouraging open conversations about opioid safety and naloxone in your circles can help reduce stigma and spark more preparedness where you live.
Naloxone in Everyday Life: Real World Uses and Stories
Naloxone isn’t just for clinics or EMTs. These days, I see it in schools, workplaces, libraries, and other big public spaces. Community members, teachers, and even local business owners often get trained and carry it. It’s become one of those things people have, ready in an emergency.
I know of parents who keep a kit handy, even if no one in their family takes prescription pain meds, just to be safe. Libraries in some states keep naloxone on site because public overdoses do happen, and quick action can save lives. The more common it becomes, the more we help reduce fear and stigma around asking for help.
- Public spaces: Schools, parks, and businesses keep naloxone handy.
- Families: Parents and caretakers find peace of mind having a kit nearby.
- Travel: Folks don’t leave home without it if opioids are in their home.
Frequently Asked Questions About Opioid Overdose Antidotes
Here are some questions people often ask me or search for online:
Question: Can anyone use naloxone in an emergency?
Answer: Yes. You don’t need to be a health professional. Kits come with simple instructions, and 911 operators often walk you through the steps.
Question: Is it legal for me to carry naloxone even if I don’t use opioids?
Answer: Definitely! In almost all states, anyone can purchase, carry, and use naloxone in an emergency. Most places even have Good Samaritan protections for users or people helping out in overdoses.
Question: Does naloxone work on all drug overdoses?
Answer: No. Naloxone only reverses opioid overdoses (things like heroin, fentanyl, oxycodone, and morphine). It won’t reverse overdoses from other drugs like benzodiazepines, cocaine, or alcohol.
Question: Can you use naloxone on children and pets if they’ve been exposed to opioids?
Answer: Yes. Emergency services may use naloxone in children or even pets who have been exposed to or overdosed on opioids, but it’s still smart to call 911 or a vet right away.
Key Takeaways for Staying Prepared
Naloxone can turn a frightening emergency into a survivable situation and is becoming much easier to get and use than ever before. If you or someone you know takes opioids, having naloxone around and learning how to use it is a practical step, kind of like carrying a spare tire or a fire extinguisher.
Learning how to spot an overdose, how to use naloxone, and how to find community resources can help keep you and the people around you a lot safer. It’s a small effort for some pretty tremendous peace of mind.
Video: Opiate Overdose Antidote