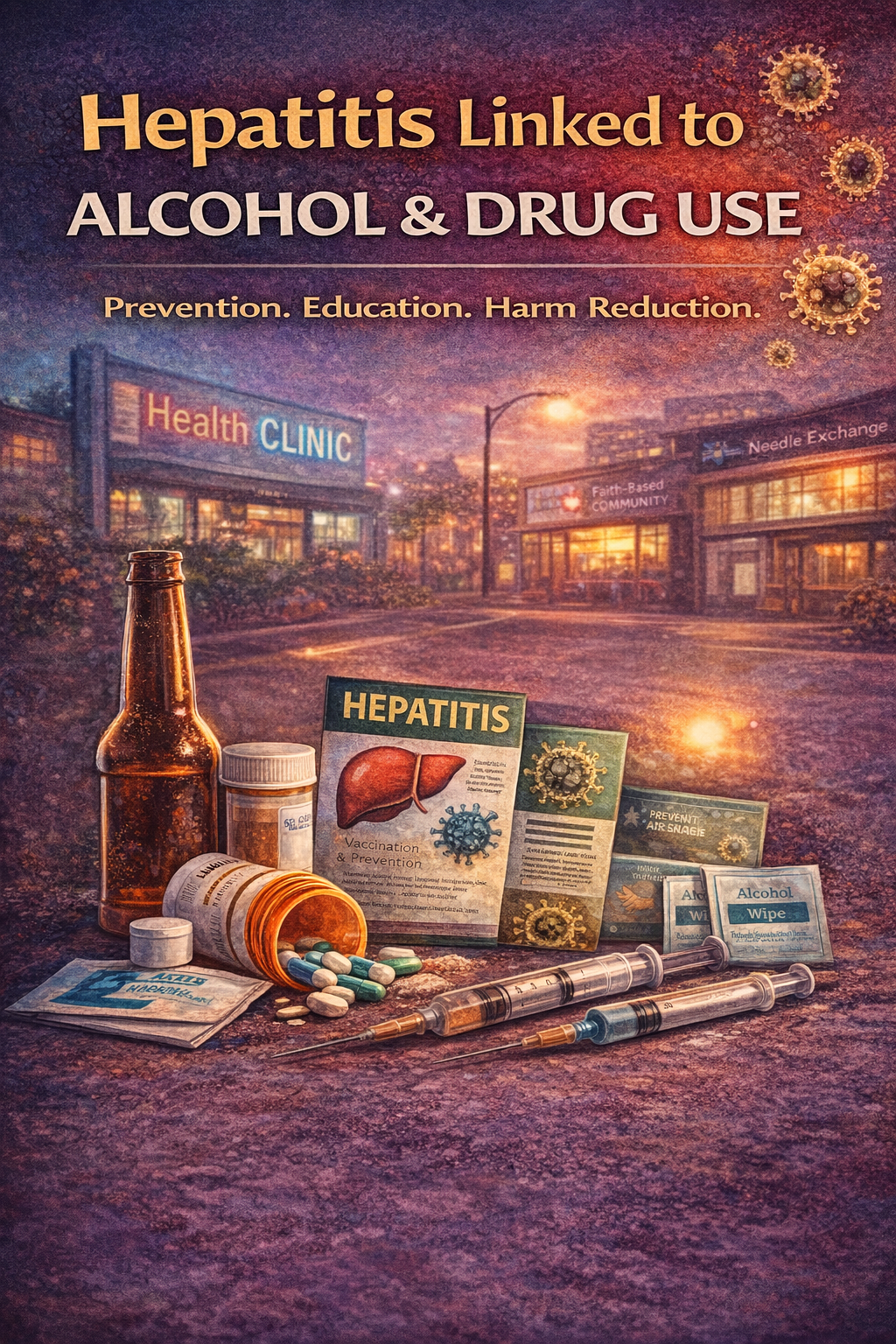
Hepatitis, an inflammation of the liver, is closely linked to alcohol and drug addiction due to behaviors and substances that damage or infect the liver. Chronic alcohol use directly causes liver inflammation and scarring, while injection drug use increases the risk of transmitting viral hepatitis—particularly Hepatitis B and C—through shared needles or unsterile equipment. The combination of substance misuse and hepatitis can severely compromise physical health and recovery outcomes. Preventing hepatitis in this context requires a comprehensive approach: self-management through sobriety, vaccination, and healthy lifestyle choices; family support to encourage medical care, open communication, and harm-reduction awareness; and community resources that provide access to education, screening, and clean-use programs. Together, these layers of support protect liver health, reduce stigma, and strengthen recovery efforts.
Hepatitis and Addiction: How Alcohol and Drug Use Impact Liver Health
Hepatitis—particularly types A, B, and C—is a serious inflammation of the liver that is closely linked to alcohol and drug use behaviors. Long-term or excessive alcohol consumption directly damages liver cells, accelerating inflammation and leading to alcoholic hepatitis, cirrhosis, and even liver failure. Likewise, drug addiction, especially injection drug use, greatly increases the risk of viral hepatitis transmission through shared or contaminated equipment. Hepatitis C is most commonly spread this way. When addiction and hepatitis occur together, they create a dangerous cycle—liver disease worsens substance effects, and declining health increases vulnerability to relapse.
How Addiction Contributes to Hepatitis
Alcohol Use
- Chronic alcohol use inflames and scars liver tissue.
- Alcohol weakens immune function, increasing vulnerability to hepatitis infections.
Injection Drug Use
- Sharing needles, syringes, or preparation equipment transmits blood-borne viruses, especially hepatitis B and C.
- Even non-injection drug use, such as sharing straws or pipes, can spread infection through microscopic skin or nasal tears.
Polydrug Use
- Combining alcohol with prescription or illicit drugs multiplies liver strain and accelerates hepatitis progression.
Symptoms and Complications
- Fatigue, nausea, jaundice, dark urine, abdominal discomfort, and appetite loss.
- Advanced complications include cirrhosis, liver cancer, and liver failure.
- Co-occurring substance use disorders often delay diagnosis and treatment.
Treatment and Prevention Approaches
Medical Treatment
Antiviral medications for hepatitis B and C, along with medical management and abstinence-based care for alcoholic hepatitis.
Integrated Addiction Treatment
Programs that combine medication-assisted therapy (MAT) with routine hepatitis testing and liver health monitoring.
Harm Reduction
Needle-exchange services, safe-use education, vaccination programs, and guidance to avoid alcohol during liver recovery.
Community Outreach
Public health initiatives that connect individuals to both addiction recovery services and liver health care.
Conclusion
Hepatitis and addiction are deeply intertwined public health challenges—each intensifying the impact of the other. Alcohol directly damages the liver, while injection drug use spreads viral hepatitis, leading to lifelong health consequences. Addressing both conditions requires a comprehensive, stigma-free approach that integrates medical care, addiction treatment, harm-reduction strategies, and community support. When liver health becomes part of recovery planning, individuals can heal from addiction while protecting long-term physical well-being—building a healthier and more sustainable life in recovery.
Self-Management Strategies to Prevent Hepatitis Related to Alcohol and Drug Use
Hepatitis related to alcohol and drug use is preventable when individuals take active steps to protect their liver health and reduce infection risk. Excessive alcohol damages liver tissue, while unsafe drug practices—especially injection use—raise the risk of viral hepatitis transmission. Through self-management strategies focused on health awareness, harm reduction, and recovery support, individuals can significantly lower their risk while strengthening long-term wellness.
🧠 1. Commit to Sobriety or Reduced Use
Alcohol and certain drugs strain the liver and weaken immune defenses, making hepatitis more likely to develop or worsen.
Strategies:
- Set a personal goal for abstinence or harm reduction supported by counseling or recovery programs.
- Replace substance-use triggers with healthy coping tools such as exercise, journaling, or mindfulness.
- Work with healthcare providers to manage cravings through Medication-Assisted Treatment (MAT) when appropriate.
Goal: Protect liver health and reduce conditions that accelerate hepatitis progression.
💉 2. Avoid Needle Sharing and Unsafe Drug Practices
Injection drug use remains the leading cause of Hepatitis B and C transmission.
Strategies:
- Never share needles, syringes, or preparation equipment.
- Use sterile supplies from needle exchange or harm reduction programs.
- When possible, transition to non-injection methods under medical supervision.
Goal: Prevent blood-to-blood transmission of hepatitis viruses.
💪 3. Get Vaccinated and Screened Regularly
Vaccination and early detection are powerful prevention tools.
Strategies:
- Receive Hepatitis A and B vaccinations.
- Request routine liver function and hepatitis screening if you have a history of alcohol or drug use.
- Follow medical treatment plans if hepatitis is diagnosed.
Goal: Build immunity and detect infections early for better treatment outcomes.
🥗 4. Maintain Liver-Friendly Nutrition and Hydration
A healthy diet supports liver repair and reduces inflammation.
Strategies:
- Eat a balanced diet rich in fruits, vegetables, and lean proteins.
- Drink adequate water daily.
- Avoid unnecessary medications that strain the liver, such as excessive acetaminophen.
Goal: Strengthen liver function and reduce further damage.
🧘 5. Manage Stress and Emotional Triggers
Stress increases the risk of relapse and weakens immune function.
Strategies:
- Practice mindfulness, breathing exercises, or yoga.
- Maintain daily routines that include rest and reflection.
- Seek therapy or peer support groups to manage cravings and emotional strain.
Goal: Build emotional resilience that supports both recovery and physical health.
🤝 6. Stay Connected with Health and Support Services
Consistent care ensures prevention efforts remain strong.
Strategies:
- Enroll in integrated programs addressing both addiction recovery and liver health.
- Communicate openly with healthcare providers about substance-use history.
- Participate in community harm-reduction and wellness services.
Goal: Combine medical care and recovery support into one sustainable health plan.
✅ Summary
Preventing hepatitis linked to alcohol and drug use requires a holistic self-management approach that protects both body and mind. By practicing sobriety or harm reduction, using safe health behaviors, staying up to date on vaccinations and screening, maintaining a healthy diet, and managing stress, individuals can significantly lower their risk of liver disease. When personal responsibility is combined with medical care and community support, long-term healing and recovery become achievable and sustainable.
Family Support Strategies to Prevent Hepatitis Related to Alcohol and Drug Use
Hepatitis related to alcohol and drug use is both a medical and behavioral health concern. Excessive alcohol consumption damages liver tissue, while unsafe drug practices—especially injection use—increase the risk of viral hepatitis transmission. Families play a powerful role in prevention by promoting healthy choices, reducing infection risk, and supporting long-term recovery through education, communication, and coordinated care.
When families provide informed, compassionate support, they become a protective force against both substance-related harm and liver disease.
🏠 1. Encourage Open and Nonjudgmental Communication
Honest conversation reduces secrecy and risky behavior.
Strategies:
- Talk about hepatitis and substance use in a health-focused, non-blaming way.
- Use “I” statements such as, “I care about your health and want you to be safe.”
- Stay available for ongoing discussions about stress, cravings, or relapse fears.
Goal: Build trust so your loved one feels supported rather than shamed when discussing sensitive topics.
💉 2. Promote Safe Practices and Harm Reduction
Practical safety steps lower the risk of hepatitis transmission.
Strategies:
- Encourage participation in harm-reduction services, such as needle exchange programs or safe-use education.
- Help locate vaccination clinics for Hepatitis A and B.
- Keep personal hygiene items (razors, toothbrushes) separate if a family member has hepatitis.
Goal: Reduce infection risk while still supporting recovery progress.
👩⚕️ 3. Support Regular Medical Care and Screening
Consistency in healthcare prevents silent disease progression.
Strategies:
- Offer transportation or reminders for medical appointments and liver screenings.
- Encourage honest communication with healthcare providers about substance-use history.
- Celebrate milestones such as completing vaccinations or improved liver test results.
Goal: Reinforce health accountability through positive family involvement.
❤️ 4. Encourage Recovery and Healthy Lifestyle Choices
Healthy family routines strengthen recovery stability.
Strategies:
- Share wellness activities such as home-cooked meals, walks, or relaxation time.
- Reduce alcohol presence in the household.
- Support participation in counseling or recovery groups addressing both addiction and health.
Goal: Create a home environment that supports healing and balance.
🧠 5. Educate the Whole Family About Hepatitis
Knowledge reduces stigma and misinformation.
Strategies:
- Attend family education sessions through health departments or recovery centers.
- Learn how hepatitis spreads, how it’s treated, and how to prevent it.
- Discuss vaccination, safe sexual practices, and avoidance of shared drug equipment.
Goal: Build informed empathy and shared responsibility for prevention.
🤝 6. Connect with Family and Community Support Networks
Families stay stronger with external guidance.
Strategies:
- Join family support groups such as Al-Anon, Nar-Anon, or hepatitis-focused networks.
- Connect with community health programs offering education and prevention services.
- Advocate for integrated care that addresses addiction and liver health together.
Goal: Strengthen family resilience through shared knowledge and community resources.
✅ Summary
Preventing hepatitis in families affected by alcohol or drug use begins with education, empathy, and connection. By fostering open communication, supporting medical care, encouraging harm reduction, and modeling healthy lifestyles, families become essential partners in protecting liver health and sustaining recovery. When guided by compassion and informed action, families can help loved ones heal safely, reduce infection risk, and build healthier futures together.
Community Resource Strategies to Prevent Hepatitis Linked to Alcohol and Drug Use
Hepatitis linked to alcohol and drug use remains a major public health concern, particularly among individuals facing substance use disorders. Excessive alcohol consumption accelerates liver damage, while unsafe drug-use practices—especially injection use—raise the risk of viral hepatitis transmission. Communities play a vital role in prevention by providing harm-reduction services, accessible healthcare, education, and integrated recovery support. When community systems work together, they form a bridge between prevention, early detection, and long-term healing.
🏥 1. Expand Access to Harm Reduction Services
Harm reduction programs are among the most effective tools for preventing hepatitis transmission.
Strategies:
- Establish and expand needle and syringe exchange programs to ensure access to sterile equipment.
- Provide supervised consumption or safe-use spaces to reduce infection and overdose risk.
- Distribute harm-reduction kits containing sterile supplies and hepatitis-prevention education.
- Use mobile outreach units to reach rural or underserved populations.
Goal: Reduce Hepatitis B and C transmission through direct prevention and safer-use education.
💉 2. Increase Vaccination and Screening Programs
Community health centers are essential for early detection and immunity building.
Strategies:
- Offer free or low-cost Hepatitis A and B vaccinations through clinics and community events.
- Host routine hepatitis testing days alongside addiction treatment or health fairs.
- Train community health workers and peer educators to promote screening and vaccination.
Goal: Detect infections early and prevent community-wide transmission.
📚 3. Deliver Education and Public Awareness Campaigns
Knowledge reduces stigma and encourages prevention.
Strategies:
- Launch public campaigns connecting liver health with addiction recovery.
- Integrate hepatitis education into schools, workplaces, shelters, and faith-based programs.
- Use social media, local radio, and clinic posters to share prevention information.
Goal: Normalize hepatitis prevention as part of responsible health and recovery.
🤝 4. Build Cross-Sector Partnerships
Successful prevention requires coordinated systems of care.
Strategies:
- Partner with public health departments, addiction treatment centers, and hospitals for integrated services.
- Collaborate with housing, justice, and social-service programs to reach high-risk populations.
- Secure federal and state funding to sustain prevention initiatives.
Goal: Create a unified network connecting healthcare, recovery services, and outreach.
🧠 5. Offer Peer Support and Recovery-Based Outreach
Lived experience strengthens trust and engagement.
Strategies:
- Train peer recovery coaches to provide education on hepatitis prevention and healthcare navigation.
- Include liver-health check-ins in recovery meetings.
- Support peer-led anti-stigma campaigns.
Goal: Empower individuals to sustain prevention behaviors through peer connection.
🌍 6. Address Stigma and Promote Inclusive Care
Stigma remains a major barrier to testing and treatment.
Strategies:
- Train healthcare providers in trauma-informed, nonjudgmental care.
- Offer confidential or anonymous testing services.
- Promote messaging that hepatitis and addiction are medical conditions, not moral failures.
Goal: Encourage help-seeking by creating safe, respectful care environments.
✅ Summary
Preventing hepatitis linked to alcohol and drug use requires community-wide commitment to harm reduction, accessible healthcare, education, and compassion. By integrating vaccination, screening, outreach, and recovery support, communities can lower infection rates, improve early treatment, and rebuild trust in healthcare systems. When prevention and recovery services work side by side, individuals are empowered not only to overcome addiction—but to protect and restore lifelong liver health.
Frequently Asked Questions
Here are some common questions:
1. What is hepatitis?
Hepatitis is inflammation of the liver. It can be caused by viruses (like Hepatitis A, B, or C), excessive alcohol use, certain drugs, or toxins. If untreated, it can lead to liver damage, cirrhosis, or liver failure.
2. How is alcohol linked to hepatitis?
Heavy or long-term alcohol use directly damages liver cells and causes alcoholic hepatitis. Over time, this can progress to permanent scarring (cirrhosis) and liver failure.
3. How does drug use increase hepatitis risk?
Injection drug use is the leading cause of Hepatitis C transmission. Sharing needles or other equipment can spread viruses through infected blood. Even snorting drugs with shared tools can cause small nasal cuts that transmit infection.
4. Can someone have hepatitis without knowing it?
Yes. Many people have no symptoms for years. This is why screening is important, especially for individuals with a history of alcohol misuse or drug use.
5. Which types of hepatitis are most connected to drug use?
Hepatitis B and C are most strongly linked to injection drug use. Hepatitis C is especially common among people who share needles.
6. Is there a vaccine for hepatitis?
Yes. Vaccines exist for Hepatitis A and B. There is currently no vaccine for Hepatitis C, but it is curable with antiviral medication.
7. Can hepatitis be cured?
• Hepatitis C can usually be cured with modern antiviral treatment.
• Hepatitis B can be managed but not always fully cured.
• Alcoholic hepatitis improves with sobriety and medical care.
8. Can people in addiction recovery still get hepatitis treatment?
Yes. Many programs now offer integrated care, treating addiction and hepatitis at the same time for better outcomes.
9. Does quitting alcohol or drugs help the liver heal?
Absolutely. Stopping alcohol use allows liver cells to recover. Treating hepatitis early, plus sobriety, greatly reduces long-term damage.
10. Can hepatitis spread within families?
Hepatitis B and C spread through blood or bodily fluids — not casual contact. Families should avoid sharing razors, toothbrushes, or needles and follow vaccination guidance.
11. Are harm-reduction programs really effective?
Yes. Needle exchange programs, safe-use education, and vaccination clinics significantly reduce hepatitis transmission in communities.
12. What are common symptoms of hepatitis?
Fatigue, nausea, yellowing of skin or eyes (jaundice), dark urine, abdominal pain, and loss of appetite. Many people have no symptoms early on.
13. Why is hepatitis more dangerous when combined with addiction?
Substances strain the liver while hepatitis attacks it. Together, they accelerate damage and increase health risks.
14. How can someone know if they are at risk?
Risk increases with injection drug use, heavy alcohol use, past blood transfusions before 1992, or unprotected sex with infected partners. Testing is the only way to know.
15. What is the best way to prevent hepatitis?
Vaccination, avoiding needle sharing, practicing safe sex, reducing alcohol use, and getting regular medical screening.
Conclusion
Hepatitis prevention in the setting of alcohol and drug addiction depends on coordinated action at individual, family, and community levels. Self-management empowers individuals to make safer health decisions through consistent medical care, vaccination, and stress management. Family involvement reinforces accountability and compassion, helping loved ones stay engaged in treatment and avoid risky behaviors. Meanwhile, community resources—such as needle exchanges, vaccination drives, and public health education—extend protection to broader populations and reduce transmission. When these strategies unite, they not only prevent hepatitis but also promote holistic healing from addiction—supporting long-term recovery, liver health, and overall well-being.
Video: