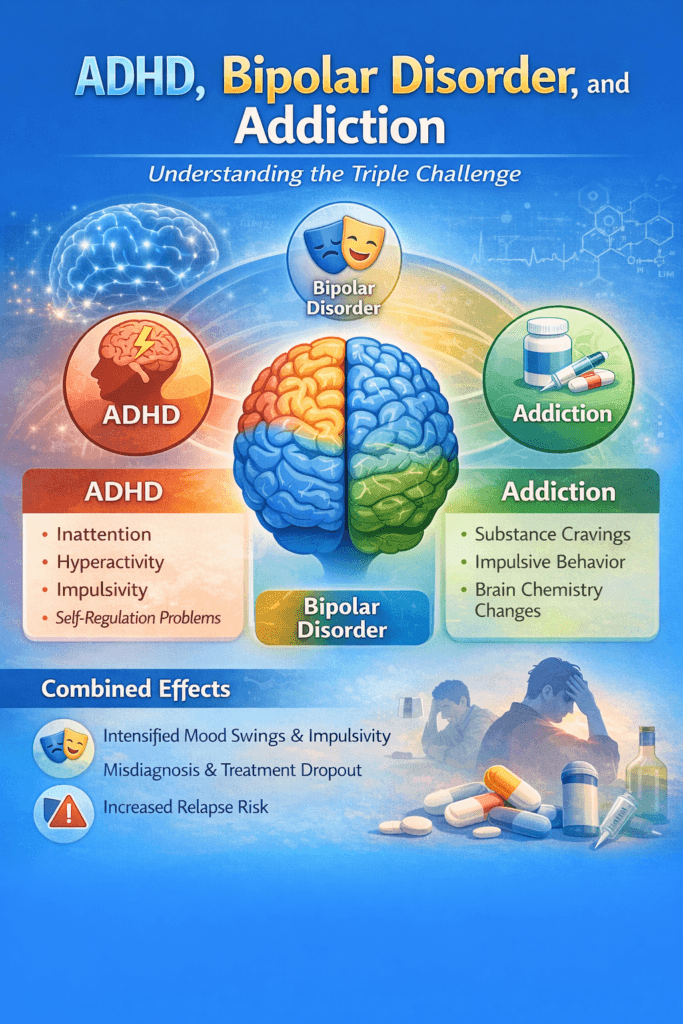
ADHD, bipolar disorder, and addiction form a powerful and often overwhelming combination of co-occurring conditions. ADHD affects attention, impulsivity, and self-regulation, while bipolar disorder brings cycles of depression and mania that destabilize mood and behavior. When addiction enters this picture, substance use can become a way to self-medicate distress, intensify impulsive actions, and disrupt brain chemistry even further. This intertwined relationship makes daily functioning challenging and increases the risk of relapse, misdiagnosis, and treatment dropout. Understanding how these conditions interact is the first step toward building effective, integrated care and long-term recovery.
ADHD, Bipolar Disorder, and Addiction: Understanding the Triple Challenge
Co-occurring mental health disorders significantly increase vulnerability to substance use disorders. Among the most complex combinations is Attention-Deficit/Hyperactivity Disorder (ADHD) alongside Bipolar Disorder, which together create powerful emotional, cognitive, and behavioral instability. When addiction is added to this mix, individuals often experience intense mood swings, impulsivity, attention difficulties, and substance cravings that reinforce one another. Understanding how these conditions interact is essential for developing effective, integrated treatment strategies that support long-term recovery.
How ADHD and Bipolar Disorder Interact
ADHD is characterized by inattention, hyperactivity, impulsivity, and difficulty with self-regulation. Bipolar disorder involves cycles of depression and mania or hypomania. When both occur together, individuals may experience rapid mood shifts, poor decision-making, emotional reactivity, and difficulty maintaining routines. During manic phases, impulsivity and risk-taking behaviors increase, while depressive phases can trigger hopelessness and self-medication. These overlapping symptoms often obscure one another, delaying accurate diagnosis and treatment.
Why Addiction Risk Is Higher
Substance use often begins as an attempt to manage uncomfortable symptoms. Stimulants or alcohol may be used to control restlessness or mood swings. Sedatives or opioids may be used to escape emotional pain or insomnia. Unfortunately, self-medication disrupts brain chemistry further, worsens mood instability, and strengthens addiction pathways. Individuals with ADHD and bipolar disorder are statistically more likely to develop substance use disorders and experience earlier relapse without integrated care.
Treatment Challenges
Treating one condition while ignoring the others rarely succeeds. ADHD medications can influence mood stability. Bipolar medications may affect focus and energy. Addiction treatment must consider both. Without careful coordination, medication interactions, untreated symptoms, or inconsistent routines can undermine progress. This complexity makes integrated, multidisciplinary treatment essential.
Integrated Recovery Strategies
Effective care combines mood stabilization, ADHD symptom management, and addiction treatment simultaneously. Common strategies include mood stabilizers or atypical antipsychotics for bipolar disorder, carefully monitored ADHD medications when appropriate, and evidence-based addiction therapies such as cognitive behavioral therapy, dialectical behavioral therapy, and peer recovery support. Structured daily routines, sleep regulation, and stress-management skills help stabilize brain function across all three conditions. Family education and community support further strengthen recovery outcomes.
The Importance of Accurate Diagnosis
Many individuals receive treatment for only one disorder for years before the full picture is recognized. A comprehensive psychiatric evaluation ensures that ADHD, bipolar disorder, and addiction are addressed together rather than in isolation. Accurate diagnosis reduces the risk of relapse, improves medication effectiveness, and increases quality of life.
Conclusion
ADHD, bipolar disorder, and addiction form a challenging but treatable combination. When care addresses all three conditions together, individuals can achieve emotional stability, improved focus, reduced substance cravings, and meaningful long-term recovery. Integrated treatment, compassionate support, and consistent self-management transform complexity into resilience — proving that even the most difficult co-occurring disorders can heal with the right approach.
Self-Management Strategies for ADHD, Bipolar Disorder, and Addiction
Living with ADHD, bipolar disorder, and addiction creates a unique and demanding recovery journey. Each condition affects brain chemistry, emotional regulation, and decision-making, often amplifying the symptoms of the others. While professional treatment is essential, self-management strategies play a powerful role in stabilizing daily life, preventing relapse, and building long-term resilience. When individuals learn practical skills to manage focus, mood, and cravings together, recovery becomes more sustainable and self-directed.
Establishing Structured Daily Routines
Consistency is grounding for brains affected by ADHD and bipolar disorder. Regular wake times, meal schedules, medication routines, therapy appointments, and sleep habits reduce chaos and impulsive decision-making. Visual planners, phone reminders, and habit-tracking apps help maintain structure and minimize forgetfulness.
Mood and Symptom Tracking
Monitoring mood swings, energy levels, attention changes, and cravings helps identify early warning signs of relapse or manic or depressive episodes. Simple daily logs or tracking apps provide valuable information to adjust medications and develop coping strategies before symptoms escalate.
Medication Adherence and Safety
Taking medications exactly as prescribed is critical when treating co-occurring disorders. Skipping doses, doubling medication, or mixing substances can quickly destabilize mood and increase relapse risk. Pill organizers, alarms, and trusted support persons can reinforce adherence and accountability.
Developing Healthy Coping Skills
Because impulsivity and emotional intensity are common, building non-substance coping tools is essential. Mindfulness, breathing exercises, physical activity, creative hobbies, and grounding techniques help regulate stress and attention without relying on substances.
Managing Impulsivity and Cravings
Delaying action during emotional surges reduces the risk of impulsive decisions. Techniques such as the ten-minute pause rule, distraction strategies, or calling a peer supporter can help urges pass safely. Removing access to substances and limiting high-risk environments further protects recovery.
Sleep and Energy Regulation
Sleep disruption triggers both bipolar mood episodes and ADHD symptom worsening. Maintaining consistent sleep schedules, limiting nighttime screen time, and using relaxation routines help stabilize energy and emotional balance.
Building Support Networks
Peer recovery groups, ADHD or bipolar support communities, sponsors, and family members provide encouragement and accountability. Connection reduces isolation and reinforces commitment to treatment goals.
Knowing When to Ask for Help
Recognizing early signs of mania, depression, medication side effects, or rising cravings allows individuals to seek professional help promptly. Early intervention prevents setbacks from becoming full relapses.
Conclusion
Managing ADHD, bipolar disorder, and addiction requires daily commitment, but effective self-management makes stability achievable. Through structured routines, medication adherence, symptom tracking, healthy coping skills, and strong support systems, individuals can regulate focus, mood, and cravings simultaneously. Empowered self-management transforms crisis recovery into sustainable, confident living.
Family Support Strategies for ADHD, Bipolar Disorder, and Addiction
When a loved one lives with ADHD, bipolar disorder, and addiction, the entire family feels the impact. Mood swings, impulsivity, attention difficulties, and substance use can strain trust, communication, and daily stability. Yet families also hold tremendous power to strengthen recovery. With education, patience, and structured support, families can become steady anchors that reinforce treatment engagement, emotional safety, and long-term healing.
Understanding the Triple Diagnosis
Families benefit from learning how ADHD affects focus and impulse control, how bipolar disorder influences mood cycles, and how addiction alters reward pathways. Recognizing that these behaviors are symptoms — not character flaws — reduces blame and increases compassion. Informed families respond with support rather than frustration.
Creating Predictable Home Routines
Consistent daily schedules help stabilize all three conditions. Families can support regular sleep times, shared meals, medication routines, and appointment reminders. Visual calendars, alarms, and shared planners reduce confusion and prevent missed responsibilities.
Encouraging Treatment Adherence
Families play an important role in reinforcing medication adherence and therapy participation. Gentle reminders, transportation to appointments, and celebrating follow-through promote accountability without control or criticism.
Promoting Healthy Communication
Open, nonjudgmental conversations help loved ones express emotions safely. Families can practice listening without immediately fixing problems, which reduces conflict and emotional escalation.
Monitoring Warning Signs
Families often notice early mood shifts, increased impulsivity, sleep disruption, isolation, or secretive behavior before crises emerge. Sharing concerns calmly and involving providers early can prevent relapse or hospitalization.
Reducing Environmental Triggers
Removing alcohol or drugs from the home, limiting exposure to stressful environments, and encouraging healthy activities reduce temptation and overstimulation.
Supporting Non-Medication Coping Skills
Families can participate in exercise, hobbies, mindfulness practices, or outdoor activities together. Shared positive routines strengthen connection and emotional regulation.
Using Professional and Peer Resources
Family therapy, bipolar and ADHD support groups, and addiction family programs teach skills for boundary-setting, crisis response, and emotional resilience. Support for family members prevents burnout and resentment.
Practicing Boundaries with Compassion
Effective support balances empathy with clear limits. Families can encourage responsibility while avoiding enabling behaviors. Boundaries protect both recovery progress and family well-being.
Conclusion
ADHD, bipolar disorder, and addiction create complex challenges, but family support can transform recovery outcomes. Through education, structured routines, healthy communication, early intervention, and compassionate boundaries, families become powerful partners in healing. When families and treatment teams work together, long-term stability becomes not only possible but also achievable.
Community Resource Strategies for ADHD, Bipolar Disorder, and Addiction
Recovery from co-occurring ADHD, bipolar disorder, and addiction requires more than individual effort or clinical treatment alone. These overlapping conditions affect attention, mood stability, impulse control, and substance cravings — challenges that extend into daily community life. Access to strong community-based resources provides essential structure, connection, and continuity of care. When medical treatment is reinforced by community support systems, individuals gain the tools needed to maintain stability and long-term recovery.
Integrated Community Mental Health Centers
Community mental health clinics that provide coordinated psychiatric care, addiction treatment, and counseling in one location are vital for individuals with complex co-occurring disorders. These centers support medication management, therapy, crisis intervention, and case management, reducing gaps in care that often lead to relapse or hospitalization.
Peer Support and Recovery Organizations
Peer-led recovery groups and mental health support programs offer shared experience, mentorship, and encouragement. Connecting with others who manage ADHD, bipolar disorder, and addiction reduces isolation and strengthens motivation. Peer specialists also help individuals navigate treatment systems, set goals, and build confidence in daily recovery practices.
Specialized Support Groups
Community-based ADHD and bipolar disorder support groups provide education on symptom management, coping strategies, and emotional regulation. When paired with addiction recovery groups, individuals receive comprehensive peer reinforcement across all conditions rather than treating each challenge separately.
Supported Housing and Structured Living
Stable housing environments with recovery-oriented rules and accountability help minimize exposure to triggers. Recovery residences, transitional housing, and supportive living programs provide daily structure, medication oversight, and peer encouragement essential for stabilizing mood and behavior.
Vocational and Educational Programs
Community job-training services, employment assistance, and educational workshops improve financial stability and self-esteem. Meaningful work and learning opportunities reduce idle time, stress, and vulnerability to relapse.
Transportation and Access Services
Reliable transportation to therapy appointments, support meetings, and medical visits prevents missed care. Community transit vouchers or ride services remove logistical barriers to consistent participation in treatment.
Family and Community Education Programs
Public workshops on mental health, addiction, and co-occurring disorders help reduce stigma and improve family and community understanding. Informed communities are more likely to support recovery rather than reinforce shame.
Crisis and Emergency Support Resources
Hotlines, mobile crisis teams, and walk-in crisis centers provide rapid assistance during manic episodes, depressive crashes, or substance relapse risk. Immediate access to help prevents escalation into emergencies.
Conclusion
ADHD, bipolar disorder, and addiction create complex daily challenges, but community resources transform isolation into support and instability into structure. Integrated care centers, peer networks, housing programs, vocational services, and crisis supports form a recovery ecosystem that strengthens treatment outcomes. When communities invest in accessible, compassionate resources, individuals facing co-occurring disorders gain real opportunities for lasting stability and meaningful life in recovery.
Frequently Asked Questions
Here are some common questions:
What does it mean to have ADHD, bipolar disorder, and addiction together?
It means an individual experiences attention and impulse-control difficulties from ADHD, mood instability from bipolar disorder, and compulsive substance use from addiction. These conditions interact and intensify one another, thereby complicating daily functioning and recovery.
Why do these three conditions commonly occur together?
All three involve dysregulation of brain neurotransmitters related to reward, mood, and self-control. Genetics, trauma, and early life stress also increase vulnerability to developing multiple co-occurring disorders.
Does ADHD increase the risk of addiction?
Yes. ADHD-related impulsivity, restlessness, and difficulty delaying gratification increase the likelihood of experimenting with substances and developing dependence.
Does bipolar disorder increase addiction risk?
Yes. Manic episodes may lead to risky substance use, while depressive episodes may lead to self-medication with drugs or alcohol to escape emotional pain.
Why is diagnosis often delayed?
Symptoms overlap. Mood swings, attention problems, and substance effects can mask each other, leading to misdiagnosis or treatment of only one condition.
Can addiction treatment work without treating ADHD and bipolar disorder?
Usually not effectively. Untreated mood or attention symptoms often trigger relapse. Integrated treatment addressing all conditions simultaneously leads to better outcomes.
Are medications safe when treating all three conditions?
Yes, when managed by experienced clinicians. Mood stabilizers, ADHD medications, and addiction medications can be safely combined with careful monitoring.
Can stimulant ADHD medications worsen bipolar disorder?
They can if the mood is not stabilized first. Providers usually treat bipolar disorder first, then cautiously introduce ADHD medication if appropriate.
What therapies help most with this combination?
Cognitive behavioral therapy, dialectical behavioral therapy, trauma-informed counseling, and peer recovery support are commonly effective.
What are the warning signs of relapse or mood episode?
Increased impulsivity, reduced sleep, rapid speech, irritability, isolation, sudden energy surges, or return to substance use are key warning signs.
How can families help?
By learning about the disorders, encouraging treatment adherence, maintaining structured routines, and offering calm, nonjudgmental support.
How important is routine for recovery?
Very important. Regular sleep, meals, medication schedules, and planned activities help stabilize mood and reduce impulsive behaviors.
Can people recover successfully with all three conditions?
Absolutely. With integrated care, consistent self-management, and strong support systems, individuals can achieve long-term stability and meaningful recovery.
What should someone do if they feel overwhelmed by symptoms?
They should contact their healthcare provider, therapist, or crisis support services immediately. Early intervention prevents escalation.
Is long-term recovery possible?
Yes. Although the combination is challenging, coordinated medical care, therapy, peer support, and lifestyle structure make sustained recovery achievable.
Conclusion
Although ADHD, bipolar disorder, and addiction create complex challenges, recovery is absolutely possible with coordinated treatment and consistent support. When mood stabilization, attention management, and addiction care are addressed together, individuals gain greater emotional balance, improved focus, and stronger control over cravings. Therapy, medication management, structured routines, and supportive relationships work collectively to restore stability and confidence. With the right combination of professional care and personal commitment, individuals can move beyond survival mode and build meaningful, sustainable lives in recovery.
Video: How ADHD and bipolar made me an addict 😭 #mentalhealth #dualdiagnosis #recovery