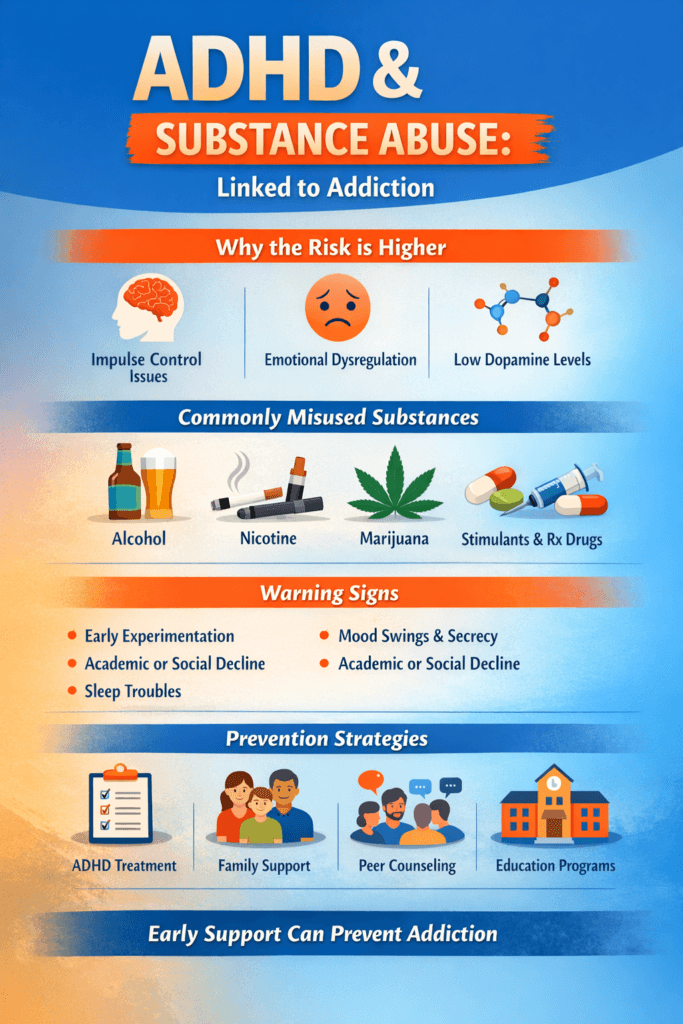
ADHD and substance abuse are closely linked to addiction through shared challenges in impulse control, emotional regulation, and brain reward functioning. Individuals with ADHD are more likely to experiment with substances early, use them to self-medicate symptoms, or struggle with managing stress and boredom, all of which increase addiction risk. Preventing this progression requires a comprehensive support system that extends beyond medical treatment alone. Effective self-management strategies help individuals regulate symptoms and develop healthy coping skills. Family support provides structure, encouragement, and early recognition of risk behaviors. At the community level, accessible mental health care, peer programs, educational services, and substance-use prevention resources create protective environments. Together, these strategies reduce vulnerability to addiction and promote long-term stability.
How ADHD and Substance Abuse Are Linked to Addiction
Attention-Deficit/Hyperactivity Disorder (ADHD) and substance use disorders are strongly connected. Research consistently shows that individuals with ADHD are at a higher risk of developing addiction compared to the general population. This link is not due to poor character or lack of willpower—it is rooted in brain chemistry, impulsivity, challenges in emotional regulation, and coping behaviors. Understanding how ADHD and substance abuse intersect helps families, clinicians, and individuals take early steps to prevent addiction and support long-term recovery.
ADHD and the Brain’s Reward System
ADHD is associated with differences in dopamine activity in the brain. Dopamine plays a key role in motivation, focus, and pleasure. When dopamine levels are lower or irregular, individuals may seek external stimulation to feel balanced or energized. Alcohol, nicotine, cannabis, and other drugs temporarily increase dopamine, which can feel relieving at first. This makes people with ADHD more vulnerable to repeated substance use and eventual addiction.
Impulsivity and Risk-Taking Behaviors
Impulsivity is a core symptom of ADHD. Difficulty pausing, thinking ahead, or weighing consequences can lead to experimenting with substances earlier and more frequently. Early experimentation is one of the strongest predictors of later addiction, placing individuals with ADHD at greater risk.
Self-Medication of ADHD Symptoms
Many people with untreated or under-treated ADHD turn to substances to cope with:
- Restlessness
- Difficulty focusing
- Anxiety or frustration
- Sleep problems
- Low self-esteem
For example, nicotine may feel calming, alcohol may reduce social anxiety, and stimulants may briefly improve focus. While these effects are temporary, they reinforce continued use and increase addiction risk.
Emotional Dysregulation and Stress
ADHD often involves intense emotional reactions, frustration, and sensitivity to rejection. Substances may become a quick way to numb uncomfortable emotions. Over time, this pattern strengthens dependence and makes quitting more difficult.
Untreated ADHD Increases Addiction Risk
Studies show that individuals with untreated ADHD have significantly higher rates of alcohol use disorder, nicotine dependence, cannabis misuse, and stimulant addiction. In contrast, proper ADHD treatment with medication, therapy, and skill-building strategies greatly reduces the likelihood of substance abuse.
ADHD Can Complicate Addiction Recovery
When ADHD is not addressed during addiction treatment, recovery becomes harder. Symptoms such as distractibility, forgetfulness, and impulsivity can interfere with therapy participation, appointment attendance, and relapse prevention plans. Treating both ADHD and addiction together leads to better recovery outcomes.
Shared Genetic and Environmental Factors
ADHD and addiction share overlapping risk factors, including family history, trauma exposure, academic struggles, and co-occurring anxiety or depression. These shared influences further strengthen the connection between the two conditions.
Summary
ADHD and substance abuse are closely linked through brain reward pathways, impulsivity, emotional regulation difficulties, and self-medication behaviors. Without proper support, these factors can lead to addiction. However, early ADHD diagnosis, consistent treatment, strong coping skills, and supportive environments significantly reduce substance misuse risk. When ADHD is managed effectively, individuals are far more likely to avoid addiction and achieve long-term stability and well-being.
Self-Management Strategies to Prevent Addiction in ADHD Patients
Attention-Deficit/Hyperactivity Disorder (ADHD) is closely linked to a higher risk of substance misuse due to impulsivity, emotional dysregulation, difficulty with self-control, and the tendency to seek stimulation. Some individuals with ADHD may turn to alcohol or drugs to cope with stress, boredom, anxiety, or low self-esteem. However, addiction is not inevitable. With effective self-management strategies, individuals with ADHD can regulate symptoms, strengthen coping skills, and reduce the risk of developing substance use disorders. The following strategies focus on building structure, emotional awareness, and healthy habits that support long-term well-being.
Follow a Consistent ADHD Treatment Plan
Taking prescribed medications correctly and attending regular medical or therapy appointments helps stabilize attention, impulse control, and emotional regulation. When ADHD symptoms are well managed, the urge to self-medicate with substances decreases significantly.
Build Structured Daily Routines
Creating predictable schedules for sleep, meals, work, exercise, and relaxation reduces chaos and overwhelm. Structure helps ADHD brains stay organized and lowers stress-triggered impulsive decisions, including risky substance use.
Practice Impulse-Control Techniques
Simple strategies such as pausing before acting, using countdown methods, or stepping away from triggering situations help manage impulsivity. Learning to delay reactions reduces the likelihood of experimenting with substances in the moment.
Develop Healthy Sources of Stimulation
ADHD brains seek dopamine and excitement. Engaging in exercise, music, art, hobbies, sports, or creative projects provides healthy stimulation that replaces the urge to seek thrills through alcohol or drugs.
Strengthen Emotional Regulation Skills
Mindfulness, deep breathing, journaling, grounding exercises, or talking through feelings help manage emotional intensity. When emotions feel manageable, substances are less likely to become a coping tool.
Identify and Avoid Triggers
Recognizing situations that increase risk—such as boredom, stress, social pressure, or certain peer groups—allows individuals to plan healthier responses and avoid environments where substances are present.
Improve Organization and Time Management
Using planners, reminder apps, checklists, and visual schedules reduces frustration and stress. Better organization lowers feelings of failure or overwhelm that can drive substance use.
Prioritize Healthy Sleep and Nutrition
Adequate sleep and balanced meals stabilize mood, attention, and energy levels. Poor sleep and irregular eating patterns worsen ADHD symptoms and increase vulnerability to impulsive behaviors.
Build a Supportive Social Network
Surrounding oneself with friends who respect healthy choices reduces exposure to substance use. Support groups or ADHD peer communities also provide encouragement and accountability.
Practice Early Help-Seeking
If curiosity or early substance use appears, reaching out to a therapist, doctor, coach, or support group early prevents progression to addiction. Early action leads to better long-term outcomes.
Summary
Preventing addiction in ADHD patients requires daily self-awareness, structured routines, emotional regulation, healthy stimulation, and consistent treatment engagement. When individuals with ADHD practice strong self-management strategies, they gain control over impulsivity, reduce stress, and build resilience against substance misuse. With the right tools and habits, ADHD patients can thrive, maintain balance, and protect their long-term health without relying on addictive substances.
Family Support Strategies to Prevent Addiction in ADHD Patients
Individuals with Attention-Deficit/Hyperactivity Disorder (ADHD) are at greater risk of developing substance use disorders due to impulsivity, emotional dysregulation, and difficulty managing stress. Without proper guidance, some may turn to alcohol or drugs to cope with restlessness, low self-esteem, or academic and social challenges. Family support plays a critical role in reducing this risk. When families provide structure, emotional understanding, and early intervention, individuals with ADHD are far less likely to engage in substance misuse and more likely to develop healthy coping skills.
Encourage Consistent ADHD Treatment
Families can support regular medical follow-ups, medication adherence, and therapy participation. Properly treated ADHD reduces impulsivity and improves emotional regulation, which significantly lowers the risk of self-medicating with substances.
Create a Structured and Predictable Home Environment
Establishing consistent routines for sleep, meals, homework, and recreation helps ADHD patients feel organized and less overwhelmed. Structure reduces stress and boredom—two major triggers for substance experimentation.
Promote Open and Non-Judgmental Communication
Encouraging honest conversations about emotions, struggles, and peer pressure builds trust. When individuals feel safe discussing challenges, they are less likely to hide substance use or risky behaviors.
Teach and Model Healthy Coping Skills
Families can demonstrate positive stress management through exercise, mindfulness, problem-solving, and calm communication. ADHD patients often mirror family coping styles, making role modeling essential.
Monitor for Early Warning Signs
Families should watch for sudden mood changes, secrecy, academic decline, new peer groups, or unexplained spending. Recognizing early signs of substance use allows intervention before addiction develops.
Encourage Healthy Social Connections
Supporting involvement in sports, clubs, music, or community activities helps ADHD individuals meet peers in positive environments. Healthy social networks reduce exposure to substance-using peer groups.
Limit Access to Substances at Home
Keeping alcohol, medications, and other substances secured or out of sight reduces impulsive experimentation, which is especially important for ADHD-related impulsivity.
Reinforce Positive Efforts and Progress
Praising effort rather than perfection boosts self-esteem. When ADHD patients feel capable and supported, they are less likely to seek confidence or relief through substances.
Support Emotional Regulation
Helping individuals label emotions, take breaks, and use calming techniques reduces emotional outbursts and stress-driven substance use.
Encourage Early Help-Seeking
If concerns arise, families can arrange counseling, school support, or medical assessments. Early professional involvement prevents experimentation from developing into addiction.
Summary
Family involvement is one of the strongest protective factors against addiction in ADHD patients. Through structured routines, supportive communication, healthy role modeling, and early intervention, families help individuals manage ADHD symptoms effectively and build resilience against substance misuse. With consistent family support, ADHD patients can develop confidence, stability, and lifelong healthy coping skills without relying on substances.
Community Support Resources to Prevent Addiction in ADHD Patients
Individuals with Attention-Deficit/Hyperactivity Disorder (ADHD) face a higher risk of developing substance use disorders due to impulsivity, emotional dysregulation, and a tendency to seek stimulation. Without proper support, some may turn to alcohol or drugs to self-medicate symptoms such as restlessness, anxiety, or difficulty focusing. Fortunately, strong community-based resources can play a major role in preventing addiction in ADHD patients. When communities provide accessible mental health care, structured programs, peer support, and educational services, individuals with ADHD are better equipped to manage their symptoms in healthy ways and avoid substance misuse.
Accessible Mental Health and ADHD Treatment Services
Community clinics that offer affordable ADHD evaluations, medication management, and behavioral therapy help individuals receive proper treatment early. When ADHD symptoms are well-managed, the likelihood of self-medicating with substances significantly decreases. Telehealth services also improve access for those in rural or underserved areas.
Behavioral Therapy and Skill-Building Programs
Community-based therapy programs teaching coping skills, emotional regulation, time management, and impulse control are essential. Cognitive Behavioral Therapy (CBT), ADHD coaching, and executive-function training help individuals develop structure and confidence, reducing vulnerability to risky behaviors.
Youth and School-Based Support Programs
Schools and youth centers can provide early screening for ADHD, counseling services, academic accommodations, and mentoring programs. Early identification and support during childhood and adolescence prevent later substance-use experimentation and addiction risk.
Peer Support and Social Connection
Peer groups for individuals with ADHD offer shared understanding, encouragement, and accountability. Supportive social environments reduce isolation and provide healthy stimulation that replaces risky behaviors associated with substance use.
Recreational and Skill-Based Community Programs
ADHD brains seek stimulation. Communities that offer sports leagues, art programs, music groups, gaming clubs, or outdoor activities provide safe and healthy outlets for energy and creativity, lowering the drive to seek stimulation through substances.
Family Education and Support Services
Community workshops and family counseling programs educate parents and caregivers about ADHD and addiction risk. When families understand how to support structure and emotional regulation at home, long-term outcomes improve.
Substance-Use Prevention Education
Community prevention campaigns that address ADHD-specific addiction risks help individuals recognize early warning signs and understand how to seek help before substance use becomes a problem.
Crisis and Mental Health Hotlines
Hotlines and community behavioral health crisis services provide immediate support during moments of emotional distress or impulsive urges, preventing sudden decisions that may lead to substance misuse.
Integrated Care Programs
Some communities offer integrated care where ADHD treatment, mental health services, and substance-use prevention are provided under one system. This coordinated approach ensures continuous support and reduces care gaps.
Summary
Preventing addiction in ADHD patients requires more than individual effort—it depends on strong community support systems. Accessible healthcare, therapy, peer groups, educational services, recreational programs, and family support resources help individuals manage ADHD symptoms effectively and avoid self-medication with substances. When communities invest in early intervention and supportive environments, individuals with ADHD gain the tools they need to thrive without addiction and build healthier, more stable lives.
Frequently Asked Questions
Here are some common questions:
1. Why are people with ADHD at higher risk for addiction?
ADHD affects impulse control, emotional regulation, and dopamine activity in the brain. These differences increase risk-taking behavior and make substances feel more rewarding, raising vulnerability to addiction.
2. Does ADHD cause substance abuse?
ADHD does not directly cause substance abuse, but untreated or poorly managed ADHD significantly increases the likelihood of experimenting with and misusing substances.
3. What substances are commonly misused by individuals with ADHD?
Alcohol, nicotine, cannabis, stimulants (such as cocaine or methamphetamine), and misused prescription medications are commonly reported among individuals with ADHD.
4. Do people with ADHD use substances to self-medicate?
Yes. Many individuals use substances to cope with restlessness, anxiety, poor focus, emotional distress, or sleep difficulties. This self-medication pattern can lead to dependence.
5. Can treating ADHD reduce addiction risk?
Yes. Proper ADHD treatment, including medication and behavioral therapy, improves impulse control and emotional regulation, greatly lowering the risk of substance misuse.
6. Does ADHD affect addiction recovery?
Untreated ADHD can make recovery harder due to distractibility, impulsivity, and difficulty following treatment plans. Treating both ADHD and addiction together improves success rates.
7. At what age does substance misuse usually begin in ADHD patients?
Individuals with ADHD often begin experimenting with substances earlier than their peers, which increases the likelihood of long-term addiction if not addressed early.
8. Can stimulant medications for ADHD cause addiction?
When taken as prescribed and medically monitored, ADHD stimulant medications do not increase addiction risk and may actually protect against substance misuse.
9. How can families help prevent addiction in ADHD patients?
Families can provide structure, encourage treatment adherence, model healthy coping behaviors, monitor for warning signs, and promote open communication about substance risks.
10. What self-management strategies help ADHD patients avoid substance use?
Building routines, practicing impulse control, managing stress, engaging in healthy stimulation, and seeking early help when cravings or curiosity arise are highly effective.
11. What community resources support prevention?
Community mental health clinics, ADHD coaching programs, school support services, peer groups, recreation programs, and substance-use prevention education all reduce risk.
12. Are ADHD and addiction genetically linked?
Yes. Both conditions share genetic and environmental risk factors, including family history and exposure to trauma or chronic stress.
13. Does emotional dysregulation contribute to substance use?
Yes. Difficulty managing frustration, rejection, or anxiety often leads individuals with ADHD to seek relief through substances.
14. Can children with ADHD be protected from future addiction?
Yes. Early diagnosis, consistent treatment, family involvement, school support, and positive social activities greatly reduce future addiction risk.
15. Is long-term recovery possible for individuals with ADHD and addiction?
Absolutely. With integrated treatment for both ADHD and substance use, along with strong support systems, long-term recovery and healthy functioning are very achievable.
Conclusion
Although ADHD increases the risk of substance misuse and addiction, early intervention and strong support systems can significantly change outcomes. When individuals practice self-management techniques to control impulsivity, regulate emotions, and consistently seek treatment, they strengthen their ability to make healthy choices. Families reinforce this progress by offering understanding, structure, and timely intervention. Meanwhile, community resources ensure access to therapy, skill-building programs, peer support, and prevention services that reduce isolation and risk. Through the combined efforts of personal responsibility, family involvement, and community support, individuals with ADHD can effectively manage their symptoms, avoid substance dependence, and build healthy, fulfilling lives.
Video: ADHD and Substance Abuse. The Connection #adhd