The Role of Institutional Support and Government Intervention
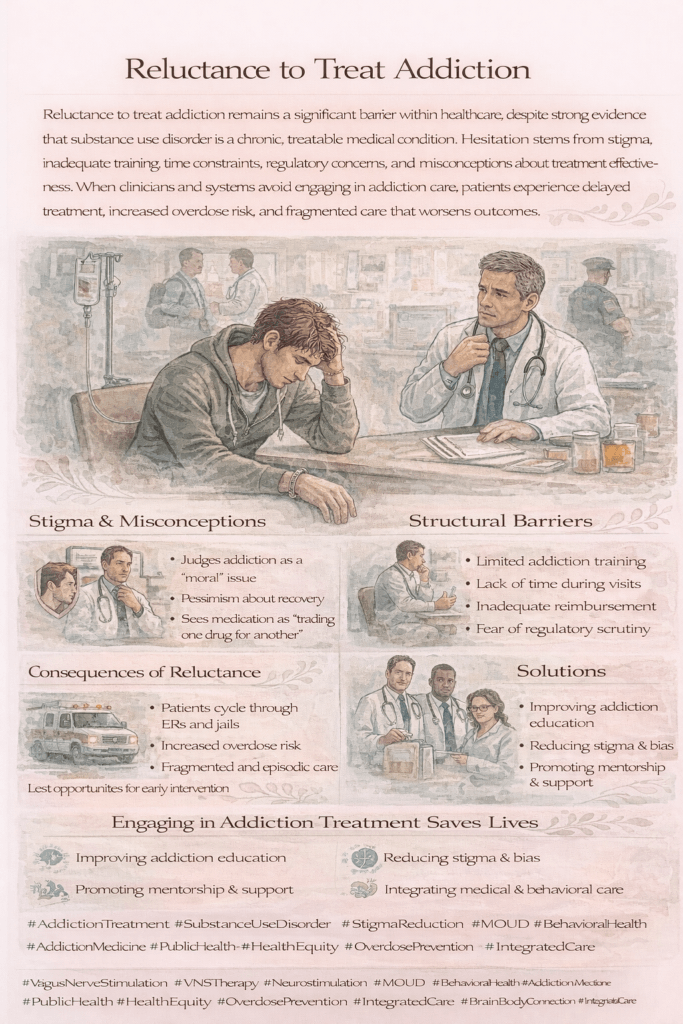
Doctors’ reluctance to treat addiction is a significant barrier to effective addiction care, often stemming from a lack of institutional support. This reluctance is multifaceted, influenced by insufficient training in addiction medicine, a shortage of resources, and the stigma that surrounds addiction treatment.
Bridging the Gap: Addressing the Lack of Addiction Training in Healthcare
In today’s healthcare landscape, addiction continues to be a significant public health crisis. However, many healthcare providers find themselves feeling ill-equipped to manage patients with substance use disorders (SUDs). Despite the complexity and prevalence of addiction, medical education programs often provide minimal coverage of addiction medicine, leaving doctors unprepared to tackle this critical issue.
Medical training typically emphasizes other areas of medicine, giving limited focus to the biological, psychological, and social components of addiction. As a result, when healthcare professionals encounter patients suffering from substance use disorders, they may hesitate to diagnose or treat the condition. This lack of confidence often stems from the minimal addiction-related coursework during medical school and residency.
The consequences of this knowledge gap can be significant. Physicians who are uncertain about their ability to handle addiction may underdiagnose the condition, fail to refer patients for appropriate care, or feel uncomfortable discussing treatment options such as medication-assisted therapy (MAT). This ultimately contributes to the stigma surrounding addiction, reinforcing the idea that it is a moral failing rather than a treatable medical condition.
To address this issue, there is a growing call for enhanced addiction training in medical education. Incorporating comprehensive instruction on substance use disorders and evidence-based treatments into the core curriculum will better prepare healthcare providers to manage addiction effectively. It will also empower doctors to engage in compassionate, informed conversations with their patients, guiding them toward recovery.
Increased access to continuing education programs and specialized training for practicing physicians is also essential. By equipping healthcare providers with the tools and knowledge they need to address addiction confidently, we can bridge the gap in care and create a more supportive environment for individuals struggling with substance use disorders.
Ultimately, recognizing and addressing the inadequacy of addiction medicine training is a critical step in improving treatment outcomes and reducing the stigma that too often surrounds addiction.
The Hidden Challenge: How Resource Constraints Hinder Effective Addiction Treatment
Even when healthcare providers are committed to addressing addiction, they often face significant barriers due to resource constraints. Treating substance use disorders (SUDs) requires a comprehensive and multidisciplinary approach. Still, many doctors lack the necessary tools, support, and infrastructure to provide the level of care their patients need.
One of the most pressing challenges is limited access to specialized treatment facilities. Addiction often requires tailored interventions such as inpatient detoxification, rehabilitation, or outpatient counseling services. However, in many areas, these facilities are either scarce or overwhelmed by demand. This shortage means that patients may face long wait times or have to travel long distances to access proper care if they can access it at all.
Moreover, addiction treatment is rarely a one-size-fits-all solution. Many patients require ongoing support services, such as therapy, peer groups, housing assistance, or employment programs, to help them recover. Unfortunately, these support services are frequently underfunded or unavailable. Healthcare providers may refer patients to services that don’t exist in their communities, leaving individuals without the holistic care they need to succeed in recovery.
In addition to these structural challenges, inadequate funding for addiction programs further compounds the issue. Many addiction services, especially those reliant on public funding, are under-resourced. This lack of financial support not only limits the availability of services but also restricts healthcare systems’ ability to hire trained specialists, provide medication-assisted treatment (MAT), or offer long-term care. The result is often fragmented or incomplete treatment, with many patients falling through the cracks of an overburdened system.
Doctors who are willing to treat addiction often find themselves working within a broken system, unable to deliver the kind of comprehensive care that addiction recovery demands. For healthcare providers, this can be a source of deep frustration, as they are forced to navigate the limitations of a system that fails to prioritize addiction care.
To address this challenge, a concerted effort is needed to invest in addiction treatment infrastructure, increase funding for support services, and ensure healthcare providers have the resources necessary to offer a full spectrum of care. By addressing these resource constraints, we can help reduce the fragmented and suboptimal treatment that too often characterizes addiction care, leading to better outcomes for patients and healthcare systems alike.
Breaking the Stigma: How Misconceptions About Addiction Impact Healthcare
Stigma remains one of the most formidable barriers to effective addiction treatment, not only for patients but also for healthcare providers. Despite growing evidence that addiction is a medical condition with biological, psychological, and social dimensions, it is still too often viewed through a moral lens. This stigma can manifest in negative attitudes, hesitation, and even discrimination in healthcare settings, creating a toxic cycle that undermines both treatment and recovery.
For many healthcare professionals, the stigma surrounding addiction may influence their willingness to engage in addiction care. Some may perceive substance use disorders as self-inflicted or rooted in poor life choices, leading them to underestimate the role of genetics, trauma, and environmental factors in the development of addiction. These misconceptions can cause doctors to avoid working with patients who struggle with addiction or fail to prioritize addiction treatment in their practice.
Even when healthcare providers do treat addiction, stigma can still affect the quality of care they provide. Research has shown that negative attitudes toward patients with substance use disorders can result in less compassionate, patient-centered care. Doctors may be less likely to explore all treatment options or may harbor unconscious biases that lead to unequal treatment compared to patients with other chronic conditions. This not only damages the doctor-patient relationship but also reinforces the shame that many individuals with addiction already feel, making them less likely to seek help.
The effects of stigma extend beyond individual providers and into the broader healthcare system. Stigmatizing beliefs about addiction can contribute to a lack of institutional support, inadequate funding for addiction programs, and a reluctance to invest in addiction training and education. As a result, addiction continues to be marginalized within the medical field, perpetuating the notion that it is less deserving of attention and resources than other health conditions.
To break the cycle of stigma, healthcare providers must first acknowledge addiction as a complex, treatable medical condition. Greater emphasis on addiction education in medical training can help dispel harmful stereotypes and equip doctors with the knowledge and tools to approach addiction care with empathy and expertise. Additionally, fostering open conversations about addiction and challenging the biases that exist in healthcare settings are crucial steps in creating a more compassionate and effective system of care.
By addressing the stigma associated with addiction, we can not only improve treatment outcomes but also ensure that healthcare providers approach addiction care with the same dedication and understanding as they would any other medical condition. It’s time to recognize that addiction is not a moral failing—it is a chronic disease that deserves our full attention and resources.
Overcoming Barriers: The Role of Government in Enhancing Addiction Care
Tackling the barriers to effective addiction treatment requires more than individual effort; it demands significant government intervention and systemic change. As the addiction crisis continues to affect millions of people globally, it is clear that increasing funding and improving medical education are critical steps to address the shortcomings in the current healthcare system.
One of the most urgent needs is increased funding for addiction services. Expanding access to treatment and support begins with making addiction care financially feasible and widely available. Government funding can improve the availability of specialized treatment facilities, enhance the support services vital to recovery, and fuel research into new and effective treatment options. Whether it’s inpatient rehabilitation centers, medication-assisted treatment (MAT), or community-based recovery programs, a more significant financial investment is essential for building a robust addiction treatment infrastructure.
Beyond expanding access, adequate funding allows healthcare systems to integrate addiction services into mainstream medical care. Instead of isolating addiction treatment in specialized centers that many patients can’t access, we can weave these services into everyday healthcare settings, such as primary care clinics or hospitals. Doing so helps normalize addiction treatment, making it a routine part of medical practice rather than something to be addressed in isolation. This integration not only increases access but also reduces the stigma surrounding addiction by treating it like any other chronic health condition.
Another critical aspect of addressing addiction is improving medical education. Currently, addiction medicine receives minimal attention in many medical training programs, leaving healthcare providers underprepared to manage substance use disorders. Comprehensive training that covers the biological, psychological, and social aspects of addiction can equip healthcare professionals with the tools they need to diagnose, treat, and support patients struggling with addiction. By incorporating addiction education into medical school curricula and continuing education programs, we can reduce the reluctance many doctors feel about treating addiction and improve the quality of care.
Medical education reform and increased government funding can drive a more compassionate and practical approach to addiction treatment. When healthcare providers are well-trained and have access to sufficient resources, they can offer more comprehensive, patient-centered care. This not only benefits individuals struggling with addiction but also strengthens the healthcare system’s ability to respond to one of the most pressing public health challenges of our time.
Addressing the addiction crisis requires more than just treating symptoms—it requires a systemic overhaul. With government support, we can expand access to treatment, enhance the quality of care, and ultimately, destigmatize addiction. By prioritizing these changes, we can ensure that addiction care becomes an integral, normalized part of our healthcare system, helping more individuals find the path to recovery.
The Challenges of Government Intervention in Addiction Care: Bureaucracy, Ethics, and Equitable Treatment
While government intervention holds the potential to transform addiction care, implementing these changes is far from straightforward. Bureaucratic inefficiencies, uneven resource distribution, and ethical dilemmas can significantly hinder efforts to enhance treatment for individuals struggling with addiction. These challenges complicate the creation of a fair, effective, and accessible system for addiction care.
One of the significant obstacles is bureaucracy. Government programs designed to improve healthcare often face slow-moving processes, layers of red tape, and political hurdles. Even when funding for addiction services is allocated, the distribution of those resources can be inefficient, leading to delays in getting services up and running. Furthermore, resource distribution is often uneven, with certain regions or communities—mainly rural or underserved areas—receiving less support. This creates disparities in access to addiction care, where some individuals may have robust resources available while others struggle to find even basic treatment options.
Navigating the complexities of healthcare systems only adds to these challenges. Integrating addiction services into mainstream healthcare is a multi-faceted process that involves coordinating between different agencies, providers, and treatment facilities. Ensuring that these systems work together seamlessly to deliver comprehensive care requires careful planning and oversight, which can be difficult when bureaucracy gets in the way.
In addition to logistical and bureaucratic hurdles, ethical dilemmas emerge in the context of addiction care. The reluctance to treat individuals with substance use disorders often stems from lingering stigma and misconceptions. Still, it directly conflicts with healthcare providers’ ethical duty to offer equitable, non-discriminatory care to all patients. Addiction is a medical condition, and withholding or limiting treatment based on the complexity or perceived “moral” nature of the disorder is a violation of the principles of fairness and equality in healthcare.
When healthcare systems fail to address addiction adequately, they are effectively denying individuals access to care that is fundamental to their well-being. This goes against the core belief that every patient should receive high-quality, compassionate care regardless of their condition. Moreover, this disparity exacerbates existing health inequalities, as marginalized communities are often disproportionately affected by both addiction and the barriers to receiving treatment.
To overcome these challenges, governments must streamline bureaucratic processes to ensure that resources are distributed equitably and efficiently. This can be achieved through improved coordination among agencies, greater transparency in the allocation of funds, and efforts to reach underserved populations. At the same time, medical professionals and policymakers must work to shift the cultural perception of addiction, recognizing it as a chronic medical condition deserving of the same attention as any other illness.
By addressing both the practical and ethical barriers to addiction care, we can move toward a system that is not only more effective but also more just. While the road to implementing government interventions in addiction care is fraught with challenges, overcoming these obstacles is essential for building a healthcare system that truly serves everyone.
Frequently Asked Questions
Here are some common questions:
Why are some clinicians reluctant to treat addiction?
Common reasons include stigma, lack of training, limited time, fear of regulatory scrutiny, inadequate reimbursement, and discomfort managing complex social or behavioral needs.
Is reluctance usually due to a lack of compassion?
No. Most reluctance is systemic rather than personal. Many clinicians want to help but feel unprepared or unsupported to provide addiction care safely and effectively.
How does stigma contribute to reluctance?
Stigma frames addiction as a moral or behavioral issue rather than a medical condition, leading to pessimism about recovery and misconceptions about treatment effectiveness.
Why are medications for opioid use disorder sometimes avoided?
Misunderstandings that medications like buprenorphine or methadone “replace one addiction with another” discourage prescribing, despite strong evidence that they reduce overdose and improve survival.
Does lack of training play a role?
Yes. Many healthcare professionals receive minimal education in addiction medicine, leaving them unsure how to screen, initiate treatment, or manage relapse.
Are regulatory concerns a barrier?
Yes. Some providers fear audits, legal consequences, or increased administrative burden, even when prescribing within guidelines.
How does time pressure affect addiction treatment?
Short visits and productivity demands make it challenging to address substance use, which often requires counseling, coordination, and follow-up.
What happens when addiction goes untreated?
Patients experience delayed care, higher overdose risk, repeated emergency visits, hospitalizations, and involvement with the criminal justice system.
Conclusion
Addressing doctors’ reluctance to treat addiction requires a multifaceted approach that includes enhancing institutional support, implementing effective government policies, and confronting ethical concerns. By tackling these issues, we can work towards providing better care for individuals struggling with addiction and ensure that all patients receive the comprehensive treatment they need and deserve.
Video: The Broken System Keeping Addicts From Help #healthcare #facts