The lack of access to addiction therapy for teens has challenges spanning various sectors. From limited pediatrician training in addiction medicine to inadequate community resources and government support, barriers abound, hindering teens from accessing the help they need. Additionally, family support strategies play a crucial role in facilitating access to therapy for teens struggling with addiction. In this discussion, we delve into the complexities surrounding teen access to addiction therapy and explore the potential impact of pediatrician training, community resources, government initiatives, and family support strategies in addressing this critical issue. By understanding these challenges and implementing targeted interventions, we can work towards ensuring that teens receive the support and treatment necessary for their recovery from addiction.
Breaking Barriers: Challenges in Teen Access to Addiction Therapy in the U.S.
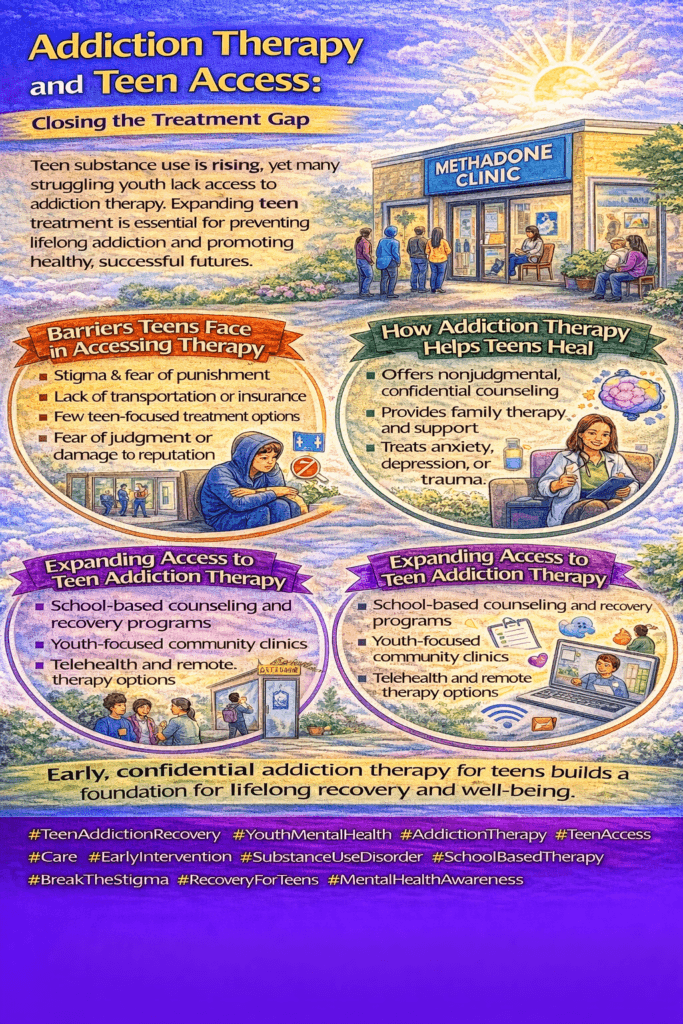
In the U.S., teens facing addiction often encounter significant barriers to accessing effective therapy, leaving many without the support they need. Understanding these obstacles is critical to improving access and care for needy young people. Here are some of the primary challenges:
- Stigma
The stigma surrounding addiction can make teens and their families hesitant to seek help, resulting in the underutilization of the limited therapy services available. Society often views addiction as a moral failing rather than a health condition, discouraging open discussions and proactive support. - Limited Resources
Specialized addiction therapy programs tailored to adolescents are limited, especially outside major urban areas. Many communities lack adequate funding, trained professionals, and dedicated treatment facilities that address the unique needs of teens, who benefit from a different approach than adults. - Lack of Awareness
Awareness is a critical factor. Many teens and parents may not be familiar with available treatment options or might struggle to recognize early signs of addiction. This lack of awareness often leads to delays in seeking help, allowing addiction to worsen. - Barriers to Access
Structural barriers, such as transportation, cost, and limited insurance coverage, further restrict access to addiction therapy. These issues are particularly pronounced for teens from low-income backgrounds or marginalized communities, who may lack affordable, nearby treatment options. - Confidentiality Concerns
Privacy is a sensitive issue for adolescents. Many teens worry that seeking therapy will expose their struggles to family members or peers, resulting in judgment or unwanted attention. This fear often deters them from reaching out for the help they need. - Reluctance to Engage
Adolescents may resist therapy due to feelings of shame, denial, or a desire to maintain independence. Therapy requires openness, which can be difficult for teens feeling vulnerable or defensive. This reluctance can make engagement challenging, limiting therapy’s effectiveness.
The Path Forward
A multifaceted approach is needed to truly address these barriers. This includes raising awareness of addiction as a health issue, increasing funding for youth-centered addiction resources, and addressing the structural and cultural barriers that hinder access. Education, stigma reduction, and privacy-protective policies can make a significant difference. Tailored interventions, informed by the specific needs of teens and their families, are crucial for building a more accessible and compassionate addiction treatment landscape for young people.
Bridging the Gap: Why Pediatricians Need More Training in Addiction Medicine
While substance use among children and teens is a critical issue, pediatricians often lack the necessary training in addiction medicine to address these challenges effectively. Several factors contribute to this training gap, but with the right changes, we can equip pediatricians to support young patients struggling with addiction. Here’s why addiction medicine training is limited in pediatrics and how we can address it:
- Historical Focus on Adults
Addiction medicine has traditionally been viewed as an adult specialty, often associated with adult patients in recovery. This history has contributed to a lack of focus on addiction training in pediatrics, even though early intervention in youth can be pivotal. - Perception of Pediatric Practice
Addiction treatment may not be considered a “core” part of pediatric care, which often emphasizes developmental milestones, general health, and preventive care. As a result, many pediatric training programs overlook addiction medicine, viewing it as outside their primary scope. - Limited Curriculum
Pediatric residency programs frequently focus on general pediatrics, development, and specific pediatric subspecialties like neonatology or adolescent medicine, leaving little room for addiction-specific training. As a result, pediatricians may receive minimal to no exposure to addiction medicine during their training. - Resource Allocation
Many training programs operate on limited resources and have to prioritize specific areas of pediatric care. Addiction medicine, not traditionally seen as a pediatric priority, often receives less funding and fewer resources, which limits program development and training opportunities. - Lack of Specialty Recognition
Addiction medicine is not always recognized as a formal subspecialty within pediatrics, reducing incentives for pediatricians to pursue specialized training in this field. Without formal recognition, few pediatricians see addiction as a viable or necessary area of focus. - Cultural Stigma
Addressing addiction in young populations can carry a significant stigma, which may discourage open conversations or proactive training in pediatric settings. This cultural hesitation can contribute to a reluctance to discuss or address addiction medicine within pediatric care.
Moving Forward
To fill this gap, concerted efforts are needed to integrate addiction medicine into pediatric training. This includes developing specialized curricula emphasizing the importance of addiction care, offering hands-on training, and encouraging mentorship in addiction medicine. Advocating for addiction medicine as a recognized pediatric specialty could also help increase interest and resources for training programs.
Equipping pediatricians with the tools and knowledge to identify and address substance use in youth will strengthen their role in preventive care and early intervention. This shift could make a profound difference in the lives of children and teens, offering them the support they need to navigate addiction issues with the guidance of trusted healthcare providers.
How Community Resources Are Expanding Access to Addiction Therapy for Teens
Access to addiction therapy can be a lifeline for teens struggling with substance use, yet many face significant obstacles in receiving the care they need. Community resources play a pivotal role in breaking down these barriers by implementing targeted strategies to reach teens and support their recovery. Here are some key ways communities are stepping up:
- Awareness Campaigns
Community organizations can run awareness campaigns to educate teens, parents, and educators about the importance of addiction therapy and the available local resources. These campaigns help break the stigma around addiction, making it easier for teens and their families to seek help without fear of judgment. - School-Based Programs
Partnering with schools to deliver addiction education, counseling, and support groups provides teens access to resources within a trusted environment. By integrating these services into schools, communities create safe spaces for teens to explore and address substance use issues. - Telehealth Services
Telehealth options allow teens to access therapy remotely, reducing barriers like transportation, privacy concerns, and stigma. Virtual counseling can significantly benefit teens in rural areas or those uncomfortable with in-person visits, providing consistent, confidential support. - Community-Based Support Groups
Support groups within the community that are tailored for teens struggling with addiction offer them a chance to connect with peers who understand their experiences. This peer support is invaluable, fostering a sense of belonging and motivating teens to stay engaged in their recovery. - Collaboration with Healthcare Providers
Partnering with local healthcare providers enables early identification and intervention. Pediatricians and primary care doctors can screen for substance use and refer teens to appropriate therapy services, streamlining the path to treatment and increasing early access to support. - Youth-Friendly Services
Making addiction therapy youth-friendly is essential for engagement. Offering flexible appointment times, incorporating technology, and using age-appropriate resources make therapy more accessible and appealing to teens, enhancing their willingness to participate. - Financial Assistance Programs
Financial barriers can deter many families from seeking addiction therapy for their teens. By offering sliding-scale fees or financial assistance programs, communities can ensure more teens have access to affordable, necessary care. - Community Collaboration
Joining forces with local government agencies, non-profits, faith-based groups, and other stakeholders allows communities to pool resources and expertise. This collaborative approach maximizes the reach and impact of addiction therapy services, creating a more robust support network for teens in need.
By tapping into these community resources and partnerships, communities can improve access to addiction therapy for teens and create a supportive, inclusive environment for their recovery. Together, these strategies make a significant difference in the lives of young people, helping them build healthier futures free from addiction.
Bridging the Gap: Why Pediatricians Need More Training in Addiction Medicine
While substance use among children and teens is a critical issue, pediatricians often lack the necessary training in addiction medicine to address these challenges effectively. Several factors contribute to this training gap, but with the right changes, we can equip pediatricians to support young patients struggling with addiction. Here’s why addiction medicine training is limited in pediatrics and how we can address it:
- Historical Focus on Adults
Addiction medicine has traditionally been viewed as an adult specialty, often associated with adult patients in recovery. This history has contributed to a lack of focus on addiction training in pediatrics, even though early intervention in youth can be pivotal. - Perception of Pediatric Practice
Addiction treatment may not be considered a “core” part of pediatric care, which often emphasizes developmental milestones, general health, and preventive care. As a result, many pediatric training programs overlook addiction medicine, viewing it as outside their primary scope. - Limited Curriculum
Pediatric residency programs frequently focus on general pediatrics, development, and specific pediatric subspecialties like neonatology or adolescent medicine, leaving little room for addiction-specific training. As a result, pediatricians may receive minimal to no exposure to addiction medicine during their training. - Resource Allocation
Many training programs operate on limited resources and have to prioritize specific areas of pediatric care. Addiction medicine, not traditionally seen as a pediatric priority, often receives less funding and fewer resources, which limits program development and training opportunities. - Lack of Specialty Recognition
Addiction medicine is not always recognized as a formal subspecialty within pediatrics, reducing incentives for pediatricians to pursue specialized training in this field. Without formal recognition, few pediatricians see addiction as a viable or necessary area of focus. - Cultural Stigma
Addressing addiction in young populations can carry a significant stigma, which may discourage open conversations or proactive training in pediatric settings. This cultural hesitation can contribute to a reluctance to discuss or address addiction medicine within pediatric care.
Moving Forward
To fill this gap, concerted efforts are needed to integrate addiction medicine into pediatric training. This includes developing specialized curricula emphasizing the importance of addiction care, offering hands-on training, and encouraging mentorship in addiction medicine. Advocating for addiction medicine as a recognized pediatric specialty could also help increase interest and resources for training programs.
Equipping pediatricians with the tools and knowledge to identify and address substance use in youth will strengthen their role in preventive care and early intervention. This shift could make a profound difference in the lives of children and teens, offering them the support they need to navigate addiction issues with the guidance of trusted healthcare providers.
Government Actions to Improve Access to Teen Addiction Therapy: A Path to Recovery
The teen years are crucial for development, but for some, addiction can interrupt this path, bringing significant challenges. Addressing teen addiction requires accessible, specialized therapy, yet many adolescents struggle to find the support they need. Here’s how the government can play a transformative role in expanding access to addiction therapy for teens:
- Funding and Grants
A dedicated allocation of funds and grants for adolescent addiction therapy can make a substantial difference. By investing in expanding therapy programs specifically designed for teens, the government can establish new treatment centers, enhance existing services, and provide financial assistance for needy families. - Training and Education
It’s essential to equip healthcare professionals, educators, and community leaders with the tools to recognize addiction in teens. Through government-funded training programs, these individuals can learn evidence-based treatment approaches and effective strategies for identifying and referring teens to therapy, ensuring that more young people receive timely support. - Integration into Healthcare Systems
Integrating addiction therapy within pediatric clinics, school-based health centers, and community clinics can help normalize therapy for teens. This approach places addiction support within the familiar settings they already visit for routine care, removing barriers and making therapy more accessible. - Telehealth Services
Expanding telehealth infrastructure and supportive policies would improve access to addiction therapy, especially in rural or underserved areas. For many teens, telehealth offers a private, flexible option for counseling, which can encourage participation and continuity of care. - School-Based Programs
Schools are ideal environments for early intervention. Government partnerships with schools can promote addiction education, counseling services, and peer support groups tailored to teen needs. By implementing these programs, schools can become proactive participants in addressing and preventing addiction. - Legislation and Policy
Supportive legislation is critical to making addiction therapy accessible. By mandating insurance coverage for addiction therapy, safeguarding patient confidentiality, and integrating addiction treatment into the juvenile justice and child welfare systems, government policies can remove significant obstacles that prevent teens from receiving care. - Public Awareness Campaigns
Awareness is half the battle. Government-backed campaigns that educate parents, caregivers, and teens about addiction, reduce stigma, and emphasize the importance of early intervention can change the public perception of addiction. These campaigns can also serve as a guide to accessing available resources and providing essential information. - Research and Evaluation
Investing in research is crucial to understanding what works best in addiction therapy for teens. By funding evaluation studies, the government can gather data on effective treatment strategies and measure the impact of policies on teen addiction treatment outcomes, allowing for continuous improvement.
With these measures, the government can take a decisive stand in supporting teen addiction recovery. Funding, education, healthcare integration, and policy shifts all play a part in removing barriers to access and creating a system where teens can find the help they need. Government action has the potential to reshape how we approach teen addiction, offering a future where all young people have access to adequate, compassionate care.
The Power of Family Support in Teen Addiction Recovery: Key Strategies for Success
When it comes to teen addiction recovery, family support can make a world of difference. Families play a vital role in guiding their teens toward addiction therapy, helping them overcome barriers to access, and encouraging a successful journey to recovery. Here are some practical strategies families can implement to support their teen in accessing and engaging in addiction therapy:
- Education and Awareness
Knowledge is power. By educating themselves about addiction, its impact on teens, and available treatment options, families are better equipped to advocate for their teens. Understanding how the treatment system works and what services are available helps families make informed decisions and navigate the complexities of finding the right support. - Open Communication
Teens are more likely to seek help if they feel safe discussing their struggles. Creating a non-judgmental environment encourages open conversations about addiction. By keeping lines of communication open, families can identify when therapy might be needed and explore options together in a way that respects the teen’s feelings and autonomy. - Encouragement and Motivation
Positive reinforcement from family members can have a substantial impact on teens. Expressing support for their decision to seek therapy, offering encouragement, and focusing on the benefits of recovery can help motivate them to engage in treatment. Small gestures of reassurance go a long way in building their confidence and commitment to recovery. - Facilitating Access to Therapy
Addiction therapy often requires logistical support, and families can take active steps to make the process easier. Researching local therapy options, arranging appointments, handling insurance paperwork, and providing transportation all help remove obstacles that might prevent a teen from accessing therapy. - Involvement in Therapy
Family involvement can enhance the effectiveness of therapy. Participating in family therapy sessions, joining family support groups, and engaging in the teen’s treatment plan create a support network that reinforces their recovery. Family presence in therapy sessions fosters understanding and contributes to a more supportive home environment. - Providing Emotional Support
Addiction can bring feelings of guilt, shame, and fear, which may weigh heavily on teens. Families can offer emotional support by listening without judgment, showing empathy, and reassuring the teen of their love and commitment. This support helps teens feel understood and provides a foundation of unconditional acceptance. - Setting Boundaries and Limits
Establishing boundaries around substance use and behavior is essential in encouraging accountability. Setting consistent rules and consequences demonstrates that the family is serious about recovery. Clear expectations help teens understand that their actions have implications, motivating them to seek and engage in therapy. - Seeking Support for Themselves
Supporting a teen with addiction can be challenging for families. Seeking counseling, joining support groups, and practicing self-care can help families cope and maintain resilience. Families are better equipped to provide sustained support for their teen’s recovery journey by prioritizing their well-being.
The journey to recovery can be daunting for teens, but with their families’ unwavering support, the path becomes a bit easier. Through open communication, encouragement, involvement, and setting boundaries, families actively guide their teens toward successful treatment and long-term recovery. Together, these strategies foster a supportive environment where teens can find the strength and stability they need to overcome addiction.
By implementing these family support strategies, families can play a pivotal role in increasing access to addiction therapy for teens and supporting their journey to recovery. Family involvement helps teens navigate practical challenges, such as accessing therapy, and provides essential emotional and motivational support. Each step—from education and open communication to boundary-setting and self-care—empowers families to become advocates for their teen’s well-being. Through these actions, families contribute to a more compassionate, supportive environment that fosters healing and resilience, giving teens the foundation they need to overcome addiction and thrive.
Frequently Asked Questions
Here are some common questions:
Why is teen access to addiction therapy important?
Adolescence is a critical period of brain development. Early treatment prevents long-term addiction, mental health complications, and academic or legal consequences.
Do many teens struggle to access addiction therapy?
Yes. Barriers include stigma, lack of youth-specific programs, transportation issues, insurance limitations, and fear of parental punishment or judgment.
Why are teens afraid to seek addiction treatment?
Many fear being labeled, getting in trouble, disappointing family, or losing privacy. Confidential and supportive environments help reduce this fear.
Are adult addiction programs appropriate for teens?
Not always. Teens need age-specific treatment that addresses family dynamics, school pressures, peer influence, and emotional development.
How does early substance use affect the teen brain?
Substance use during adolescence disrupts brain development, increasing impulsivity, emotional instability, and long-term addiction vulnerability.
What types of therapy work best for teens?
Individual counseling, family therapy, peer group programs, and mental health treatment for anxiety, depression, or trauma are most effective.
Can schools help teens access addiction therapy?
Yes. School counselors, on-site therapy programs, and referral partnerships improve early identification and access to care.
Does telehealth improve teen access to therapy?
Yes. Virtual therapy reduces transportation barriers, increases privacy, and expands access in underserved areas.
Should parents be involved in teen addiction treatment?
Yes. Supportive parental involvement improves recovery outcomes, provided teens feel safe and respected.
Can teens recover successfully from addiction?
Absolutely. With early access to appropriate therapy, teens can develop coping skills, rebuild confidence, and achieve long-term recovery.
Conclusion
Addressing teens’ lack of access to addiction therapy requires a multifaceted approach involving pediatrician training, community resources, government support, and family involvement. By addressing gaps in pediatrician education, expanding community-based resources, advocating for government funding and policies, and implementing family support strategies, we can improve teens’ access to addiction therapy. Collaborative efforts across these sectors are crucial to ensuring that teens receive the support and treatment they need for addiction recovery, ultimately promoting their health and well-being.
Video: