Involuntary treatment for severe addiction is a critical yet controversial approach used when individuals are unable to seek help independently due to the intensity of their condition. While it can be life-saving, it raises ethical concerns about autonomy and treatment efficacy. Family and community support can enhance the effectiveness of involuntary treatment by providing emotional, legal, and practical resources. At the same time, self-management strategies such as resilience-building and coping skills help individuals avoid reaching a crisis point. Examining the advantages, disadvantages, and ethical challenges of involuntary treatment highlights the importance of a supportive, multifaceted approach to addiction recovery.
Involuntary Treatment for Severe Addiction: A Lifeline or an Ethical Dilemma?
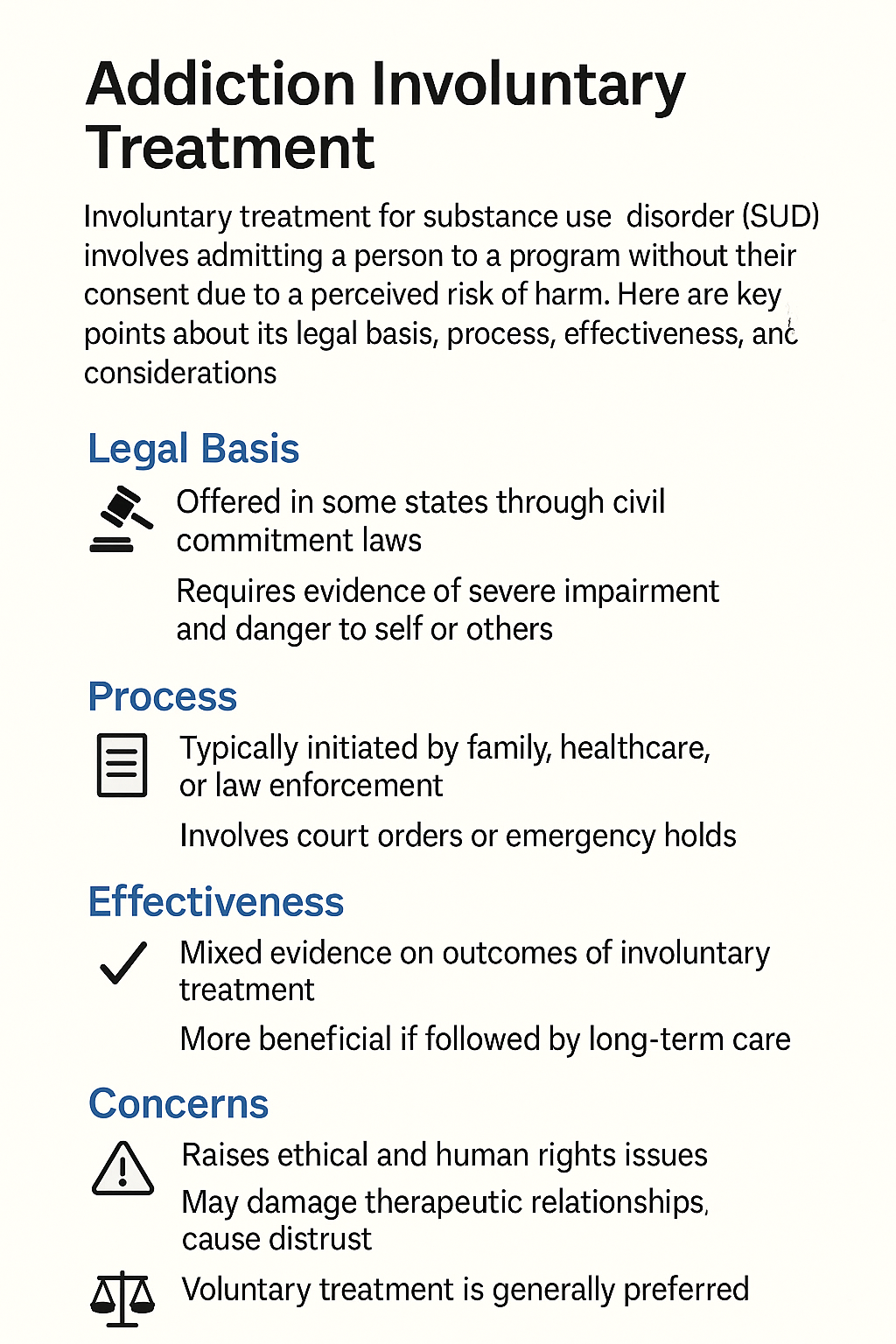
Involuntary treatment for severe addiction is a deeply complex topic, blending medical necessity, psychological care, and ethical debate. This approach involves interventions for individuals unable or unwilling to seek help voluntarily. Typically, involuntary treatment becomes an option when addiction poses a significant risk to someone’s health, safety, or well-being and when the individual cannot recognize the need for treatment. This blog explores critical forms of involuntary treatment, the legal and ethical considerations, and the challenges surrounding this controversial yet life-saving practice.
Key Types of Involuntary Treatment:
- Court-Ordered Treatment:
When addiction-related behaviors lead to legal trouble, courts may order addiction treatment as part of sentencing or parole conditions. These court-ordered programs can vary in intensity, from inpatient (residential) to outpatient settings, depending on the addiction’s severity. - Involuntary Commitment:
In cases where someone is deemed a danger to themselves or others due to addiction, they may be involuntarily committed to a treatment facility. It is a temporary measure to ensure their safety and provide immediate care. Legal standards for involuntary commitment vary but often require proof of imminent harm, such as suicidal thoughts, severe physical deterioration, or violent behavior. - Detoxification (Detox):
For individuals physically dependent on substances, involuntary detox may be administered in hospitals or specialized centers. Detoxification is an essential first step to safely withdraw from substances under medical supervision. When individuals are unable or unwilling to seek detox, legal orders may sometimes facilitate this process. - Inpatient (Residential) Treatment:
This form of treatment involves the individual residing in a facility to receive comprehensive therapy, counseling, and medical care for their addiction. Involuntary inpatient care is often reserved for individuals with severe addiction who have not succeeded with outpatient programs or are at significant risk of harm. - Outpatient Treatment:
Mandated outpatient treatment is less intensive than inpatient care and includes scheduled therapy, counseling, and support group sessions. While it may be enforced through court orders or as part of parole, it still offers structured, therapeutic support.
Legal and Ethical Considerations:
- Due Process:
Involuntary treatment must uphold ethical and legal standards to protect individual rights. Courts and medical professionals must often demonstrate the person’s inability to make informed treatment decisions and establish that treatment is essential to prevent harm. - Mental Health Evaluations:
Evaluations are often required to assess the individual’s mental capacity and treatment needs. These assessments aim to strike a balance between ensuring safety and respecting personal autonomy.
Effectiveness and Challenges:
Involuntary treatment can be life-saving for those in the grip of severe addiction. However, its success depends on factors such as the individual’s readiness for change, the quality of treatment, and post-treatment support. Many people initially resist treatment but, over time, engage positively in therapy and begin addressing the root causes of their addiction.
Despite its potential, involuntary treatment raises ethical concerns. Critics argue it can infringe on personal autonomy, and some individuals may not benefit from a forced approach if they are not mentally prepared for recovery. However, the goal remains to provide compassionate, effective care that fosters long-term recovery and safeguards health.
In summary, involuntary treatment for severe addiction is a nuanced approach, often viewed as a last-resort intervention when voluntary treatment has failed or is not feasible. While it poses ethical challenges, its primary aim is to save lives and help individuals reclaim their well-being. Ultimately, success in involuntary treatment requires thoughtful application, ethical considerations, and a strong support system post-treatment.
The Benefits of Involuntary Treatment for Severe Addiction: When Compulsory Care Saves Lives
Involuntary treatment for severe addiction, while controversial, offers undeniable benefits for individuals unable or unwilling to seek help due to the depth of their addiction. This intervention is often essential in life-threatening situations, providing a structured path toward recovery. Below, we discuss the key advantages of involuntary treatment for addiction and why it can be a practical last-resort approach for those who may not pursue help otherwise.
1. Immediate Intervention for Life-Threatening Situations
- Prevents Harm: Severe addiction can place individuals in immediate danger due to overdose risks, self-harm, and dangerous behaviors. Involuntary treatment ensures urgent medical intervention, saving lives and reducing further physical and psychological harm.
- Stabilizes Health: For individuals with intense physical dependencies, such as those addicted to opiates or alcohol, involuntary treatment provides a safe space for detoxification. Supervised detox can help manage withdrawal symptoms and stabilize health in a controlled environment.
2. Addresses Denial and Lack of Insight
- Breaks Through Denial: Addiction often creates a distorted perception of self and denial of the problem’s severity. Involuntary treatment bypasses this denial, ensuring that individuals receive essential care even if they’re not yet ready to accept their addiction.
- Initiates Change: Compulsory treatment can be the first step toward recovery for those who might not realize the impact of their addiction. With structured care, individuals often gain insight into their behavior and start addressing the underlying issues contributing to their addiction.
3. Provides Structure and Accountability
- Structured Environment: Inpatient settings remove individuals from addiction triggers and provide a safe, structured space for healing. This environment fosters a focused recovery process with therapy, monitoring, and continuous support.
- Accountability: Legal or medical mandates for treatment add a layer of accountability, encouraging individuals to engage with their treatment plans. The possibility of legal consequences for non-compliance can motivate individuals to participate actively in recovery.
4. Reduces Relapse Risk
- Safe Detoxification: Many addictions involve physical dependence, making the withdrawal process challenging and dangerous without medical support. Involuntary treatment allows individuals to detox under medical supervision, minimizing relapse risks and providing symptom management.
- Ongoing Support: Involuntary treatment programs often include aftercare planning, therapy, and follow-up support to reduce relapse rates. These measures ensure that individuals have a support system as they transition back into their daily lives.
5. Legal and Court-Ordered Safety Net
- Court-Ordered Intervention: For individuals facing legal issues due to addiction, court-mandated treatment can be a lifeline. Instead of jail time, these individuals receive treatment, helping them avoid legal repercussions and address the root causes of addiction.
- Reduces Criminal Behavior: Addiction often leads to criminal behaviors like theft or impaired driving. Involuntary treatment tackles the addiction, reducing the likelihood of future criminal acts and lessening the burden on the legal system.
6. Prevents Further Psychological Damage
- Breaking the Addiction Cycle: Involuntary treatment disrupts the cycle of addiction, helping individuals start working through the negative emotions and behaviors associated with substance abuse. Structured therapy teaches healthier coping strategies and fosters emotional resilience.
- Trauma-Informed Care: Many individuals struggling with addiction have a history of trauma. Involuntary treatment programs often offer trauma-informed care, helping people heal from past experiences that may be driving their addiction.
7. Offers Comprehensive and Holistic Care
- Holistic Support: Involuntary treatment includes a range of medical, psychological, and social services, addressing every aspect of addiction. This comprehensive care helps individuals achieve long-term recovery by targeting the physical, mental, and environmental factors of addiction.
- Therapeutic Approaches: Many programs integrate Cognitive Behavioral Therapy (CBT), family counseling, and group support. These interventions help individuals understand the roots of their addiction and build strategies for a healthier future.
8. Provides Relief for Families
- Support for Families: Addiction often places a heavy burden on families who feel helpless in the face of a loved one’s addiction. Involuntary treatment provides relief, knowing their loved one receives the necessary care.
- Reduces Family Conflict: Compulsory treatment can ease family tensions by offering a clear path to recovery and addressing issues that contribute to both addiction and family conflict.
9. A Lifeline for Severe, Long-Term Cases
- Support for Resistant Cases: Involuntary care may be the only viable solution for those who have resisted voluntary treatment. A structured setting with professional support allows individuals to work through their addiction in a safe environment, which can be crucial for long-term recovery.
While involuntary treatment raises ethical concerns regarding personal autonomy, its advantages for those with severe addiction are significant. It offers a structured, life-saving path that prioritizes health, provides support, and increases the chances of lasting recovery.
The Disadvantages of Involuntary Treatment for Severe Addiction: Balancing Urgent Care and Individual Rights
Involuntary addiction treatment can be life-saving, especially in cases of severe, life-threatening substance abuse. However, it comes with substantial downsides that can affect the effectiveness and ethical standing of such interventions. Here are the key disadvantages of involuntary addiction treatment and the challenges it presents for both individuals and society.
1. Violation of Personal Autonomy
- Loss of Individual Choice: Involuntary treatment removes the person’s choice regarding their treatment, which can violate their rights. Without voluntary buy-in, individuals may resist treatment, potentially reducing its effectiveness.
- Ethical Concerns: Forcing someone into treatment raises moral questions about the balance between saving lives and respecting personal autonomy. Many believe that treatment should be a choice, as self-motivation plays a critical role in addiction recovery.
2. Resistance to Treatment
- Lack of Motivation: Forced treatment can lead to low motivation, as individuals may engage with therapy half-heartedly. Genuine recovery often requires a willingness to change, which may be absent in involuntary settings.
- Increased Resentment: Individuals forced into treatment may feel anger or resentment toward those initiating it, making them less likely to engage in meaningful recovery and complicating the therapeutic process.
3. Limited Long-Term Success
- Short-Term Compliance Over Long-Term Change: Involuntary treatment often focuses on immediate compliance rather than instilling long-term behavioral change. Without internal motivation, individuals are at higher risk of returning to old habits once released from treatment.
- Higher Risk of Relapse: Those who undergo involuntary treatment may lack the skills, motivation, or resources needed to sustain recovery after treatment, leading to increased chances of relapse when faced with familiar triggers.
4. Psychological Trauma
- Risk of Re-Traumatization: For individuals with a history of trauma, involuntary treatment settings can evoke feelings of powerlessness, potentially re-triggering trauma responses. This may worsen psychological distress, creating new challenges for recovery.
- Stigma and Shame: Experiencing involuntary treatment can reinforce feelings of shame or failure, which may alienate individuals and make them reluctant to seek help in the future.
5. Overreliance on Legal or Institutional Systems
- Criminalization of Addiction: Treating addiction as a legal issue rather than a health issue can blur the line between care and punishment. Court-ordered treatment risks stigmatizing individuals, reinforcing a punitive approach rather than focusing on recovery.
- Lack of Individualized Care: Legal mandates for treatment often lead to standardized programs that may not cater to the unique needs of each person, potentially ignoring underlying mental health or trauma issues that are key to recovery.
6. Inadequate Resources and Treatment Quality
- Overburdened Systems: Court-mandated or involuntary treatment programs may be overwhelmed with individuals, reducing the resources available for personalized attention. This often compromises the quality of care individuals receive.
- Limited Therapeutic Options: Involuntary settings may lack comprehensive therapies like trauma-informed care or family therapy, which are essential for individuals with complex addiction issues. Without tailored support, treatment outcomes may suffer.
7. Financial and Legal Costs
- High Costs: Involuntary inpatient treatment can be costly, placing financial strain on public health systems and, in some cases, on individuals and their families.
- Legal Complications: The involuntary treatment process often involves complex legal proceedings, including court hearings and monitoring. This can create additional stress for all involved and consume public resources.
8. Potential for Abuse of Power
- Risk of Misuse: Involuntary treatment can be misused by individuals or systems for reasons unrelated to the individual’s health, such as exerting control over someone or as punishment. Such misuse can lead to mistrust of treatment facilities.
- Inadequate Safeguards: Without robust oversight, involuntary treatment facilities risk human rights abuses, including neglect or mistreatment. Ensuring proper care is crucial to prevent harm to individuals who are already vulnerable due to addiction or previous trauma.
9. Potential Disruption to Relationships
- Family and Social Strain: Families may experience guilt or conflict about forcing a loved one into treatment, potentially harming their relationships. This strain can lead to isolation and weaken social support systems that are vital for recovery.
- Disconnection from Loved Ones: Individuals who initiate involuntary treatment may feel alienated from friends or family, creating emotional distance that complicates the healing process.
Involuntary addiction treatment can be a double-edged sword. While it has the potential to save lives, it must be approached with caution, respect for personal dignity, and a commitment to ethical care. Forcing individuals into treatment without comprehensive support can lead to unintended consequences that affect not only their recovery but also their relationships and future willingness to seek help. Properly managed, involuntary treatment can still play a role in severe cases, but balancing immediate intervention with respect for personal autonomy is essential for meaningful, lasting change.
The Ethical Dilemmas of Involuntary Treatment for Severe Addiction: Balancing Rights and Responsibility
Involuntary addiction treatment often brings to the forefront complex ethical dilemmas that weigh personal autonomy against societal and medical responsibility. These dilemmas involve complex questions about an individual’s right to self-determination, the role of consent, and the justice of forced interventions. Here’s an in-depth look at the ethical issues central to involuntary addiction treatment and their challenges for healthcare providers, families, and society.
1. Violation of Autonomy and Personal Freedom
- Loss of Self-Determination: A key ethical concern in involuntary treatment is the violation of a person’s autonomy—the right to make personal decisions about their own life and body. Forced treatment removes this choice, contradicting the medical ethics principle of freedom.
- Coercion vs. Consent: Forced treatment can easily be seen as coercion, especially if the individual does not believe they need help. This raises ethical questions about overriding a person’s refusal when their addiction might impair decision-making.
2. Capacity to Consent
- Mental Competence: Addiction can impair judgment and decision-making, complicating assessments of an individual’s capacity to refuse treatment. If a person’s addiction affects their cognitive capacity, ethical questions arise about whether forced treatment is appropriate.
- Informed Consent: True informed consent requires a clear understanding of options and risks. Involuntary treatment challenges this process, as those forced into care may lack the readiness to understand or engage with their treatment, complicating ethical standards for consent.
3. Best Interest vs. Autonomy
- Paternalism: Involuntary treatment is often justified as “acting in the patient’s best interest.” However, this can conflict with respecting the person’s expressed wishes. The ethical dilemma lies in deciding when intervention is appropriate for their well-being without overstepping.
- Balancing Harm Prevention with Respect for Choice: If addiction places someone at imminent risk, some argue that intervention is warranted. Yet, it is essential to weigh this against respecting their autonomy, making harm prevention without overreaching, a complex balance.
4. Potential for Abuse and Misuse of Power
- Abuse of Authority: Medical professionals, legal authorities, or even family members may view involuntary treatment as an exercise of power. This creates a risk that the system could be exploited, with treatment used to exert control rather than to address genuine medical needs.
- Involuntary Treatment and Vulnerable Populations: When addiction stems from trauma or mental health issues, forcing treatment may compound harm rather than relieve it. In these cases, there’s a danger that power dynamics could harm rather than help, raising ethical concerns about exacerbating existing trauma.
5. Justice and Fairness
- Discrimination and Stigma: Involuntary treatment programs may disproportionately affect certain groups, such as low-income or marginalized communities, potentially leading to discrimination in access to care.
- Equal Access to Care: In regions with limited resources, access to quality involuntary treatment may not be equitable. This raises ethical questions about fairness and whether individuals in under-resourced areas face discrimination or inadequate care.
6. Effectiveness and Harm of Involuntary Treatment
- Questionable Effectiveness: Some evidence suggests that involuntary treatment may not yield sustainable results if individuals are not ready to commit to change, raising questions about its efficacy and ethical justification.
- Risk of Harm: Institutional settings can cause psychological or physical harm. For example, individuals with past trauma might be retraumatized, feeling more isolated or stigmatized, which can impede long-term recovery. Ethical care requires minimizing harm and preserving dignity, even in compulsory settings.
7. Conflicting Interests and Family Pressure
- Family Dynamics and Conflicts of Interest: Families may desire their loved one’s safety but prioritize their emotional needs over autonomy. This raises ethical concerns about family influence on treatment decisions.
- Financial and Emotional Motives: In some cases, families may seek involuntary treatment due to financial stress or control dynamics, complicating the ethics behind the intervention.
8. Impact on Trust in the Healthcare System
- Erosion of Trust: Forced treatment may damage individuals’ trust in the healthcare system, potentially leading to resistance to seeking future help. This can hinder the broader goal of promoting trust-based, voluntary care for addiction.
The ethical challenges of involuntary addiction treatment underscore the tension between protecting individuals from harm and respecting their autonomy. These dilemmas require careful consideration of the person’s capacity for decision-making, potential for damage, and long-term treatment effectiveness. Addressing these issues responsibly calls for a nuanced approach guided by ethical, solid, medical, and legal frameworks that balance the right to self-determination with the societal responsibility to protect and treat severe addiction compassionately.
Family Support Strategies in Involuntary Treatment for Severe Addiction: A Path to Recovery and Reconnection
Family support is a critical factor in the success of involuntary treatment for severe addiction. While the individual may initially resist treatment, family involvement can improve the chances of long-term recovery by providing stability, emotional support, and practical assistance. Here are essential family support strategies to consider when navigating the complexities of involuntary addiction treatment.
1. Education and Awareness
- Educating Family Members: Families benefit from understanding addiction, treatment options, and the steps involved in involuntary treatment. By learning about the complexities of addiction and recovery, family members can approach their loved one’s journey with greater empathy.
- Awareness of the Treatment Process: Familiarizing themselves with treatment stages—such as detox and counseling—can help families manage expectations and provide reassurance during challenging phases.
2. Communication and Emotional Support
- Open Communication: Maintaining open lines of communication with the treatment team helps families stay informed about their loved one’s progress. This enables them to offer practical support in line with treatment goals.
- Active Listening and Validation: Families can offer emotional support by actively listening and validating an individual’s feelings, even when the individual resists treatment. This may ease some resistance and improve cooperation with treatment.
- Setting Boundaries: Clear, consistent boundaries help prevent enabling behaviors and protect family members from burnout, allowing them to provide balanced, healthy support.
3. Family Therapy and Counseling
- Involvement in Therapy: Family therapy addresses relationship dynamics, helping families understand their role in the addiction process and learn how to support recovery constructively.
- Addressing Co-dependency: Many families unknowingly enable addictive behaviors; counseling can address co-dependent dynamics and encourage healthier interactions.
- Fostering Empathy and Support: Family therapy provides a safe space to express concerns and frustrations, fostering a non-judgmental, empathetic environment.
4. Supporting Compliance with Treatment
- Encouraging Participation: Family members can encourage their loved ones to engage in treatment, even if they initially resist. Attending sessions or joining support groups shows that they care about the individual’s recovery.
- Monitoring Progress: Families can help ensure their loved one follows treatment plans and attends follow-up appointments, assisting with practical matters like transportation to reduce barriers to treatment.
5. Fostering Hope and Patience
- Maintaining Hope: Family support fosters hope throughout the recovery journey, sustaining the person’s motivation, especially when progress is slow or setbacks occur.
- Patience and Understanding: Recovery is often lengthy and requires patience from loved ones. Accepting that setbacks are part of the process can help families support without frustration or enabling.
6. Establishing Support Networks
- Support Group Involvement: Families benefit from attending support groups, such as Al-Anon or Nar-Anon, which provide coping strategies and emotional support for those affected by addiction.
- Peer Support: Connecting with others in similar situations helps family members feel less isolated and gain practical insights for supporting recovery.
7. Aftercare and Relapse Prevention
- Supporting Aftercare Plans: Families can help keep their loved ones on track by encouraging participation in aftercare programs, such as outpatient therapy or sober living arrangements.
- Relapse Prevention Strategies: Involvement in prevention planning empowers families to recognize potential triggers, promote coping strategies, and create a stable home environment conducive to recovery.
8. Providing Practical Assistance
- Stabilizing the Home Environment: Creating a supportive, sober environment reduces stressors and potential triggers. Families may offer a safe living space or financial support if needed.
- Assisting with Daily Needs: Helping with transportation, childcare, or meal preparation allows the individual to focus on recovery.
9. Dealing with Guilt and Emotional Burden
- Managing Guilt: Family members may feel guilty for past actions or for pursuing involuntary treatment. Recognizing that treatment is in the best interest of their loved one can help alleviate guilt and focus on moving forward.
- Self-Care for Family Members: Supporting someone through addiction can be overwhelming. Family members must prioritize their well-being, taking time for therapy or respite when necessary to avoid burnout.
10. Building Trust and Rebuilding Relationships
- Rebuilding Trust: Addiction can strain relationships, but family support can help restore trust over time. This requires patience, forgiveness, and consistent encouragement as their loved one works toward recovery.
- Gradual Reintegration: Families can support reintegration by celebrating small successes and creating a loving, stable environment that reinforces positive change.
Family support is a foundational element of successful involuntary addiction treatment. Through education, communication, therapy, and practical support, families can create a pathway to recovery for their loved ones. Though involuntary treatment can be emotionally challenging, a strong family network increases the chances of long-term recovery, healing relationships, and restoring hope.
Leveraging Community Resources for Successful Involuntary Addiction Treatment and Recovery
Community resources play a pivotal role in supporting individuals undergoing involuntary treatment for severe addiction. These services extend the care provided in treatment facilities and help individuals reintegrate into society, manage triggers, and reduce the risk of relapse. Here, we explore essential community resource strategies that complement treatment and family involvement to promote sustained recovery.
1. Access to Addiction Treatment Centers and Rehabilitation Services
- Local Partnerships: Communities can partner with addiction centers to provide inpatient, outpatient, and detox programs tailored to individuals in involuntary treatment.
- Sliding-Scale Payment Options: Financial support, such as sliding-scale fees, can remove cost barriers, ensuring more people can access treatment regardless of financial status.
2. Crisis Intervention and Support Services
- Hotlines and Helplines: Crisis hotlines offer immediate support for individuals and families, guiding them through emergency resources and treatment options.
- Crisis Intervention Teams: Specialized teams of mental health professionals can stabilize situations before they escalate, providing an essential bridge to involuntary treatment.
3. Legal Support and Advocacy Services
- Legal Aid: Community legal services assist families with the legal processes of involuntary treatment, including filing petitions and understanding court requirements.
- Advocacy Programs: Advocacy organizations ensure that individuals receive ethical care and protect their rights throughout involuntary treatment and recovery.
4. Social Services and Case Management Support
- Case Management: Coordinating care among healthcare providers, social services, and legal teams, case managers create a continuum of care tailored to each individual’s unique needs.
- Assistance with Benefits: Social services help individuals access entitlements, such as Medicaid or SSI, which can cover treatment costs and reduce financial barriers.
5. Job Training and Educational Programs
- Vocational Training: Employment programs help individuals build job skills and establish routines, providing stability and reducing the risk of relapse.
- Educational Support: Programs offering GED preparation, college courses, or skill-building workshops enhance self-esteem and empower individuals in recovery.
6. Mental Health Services and Dual Diagnosis Programs
- Dual Diagnosis Treatment: Community mental health centers address both addiction and co-occurring mental health disorders, a crucial component for comprehensive care.
- Outpatient Counseling: Continued access to mental health support post-treatment helps individuals manage triggers, build coping skills, and strengthen recovery.
7. Support Groups and Peer Support Networks
- Recovery Groups: Organizations like Alcoholics Anonymous and Narcotics Anonymous offer supportive, non-judgmental environments that foster connection and encouragement.
- Peer Mentors: Recovery coaches with lived experience provide guidance, motivation, and practical advice to aid the transition from treatment to independent living.
8. Transitional Housing and Sober Living Environments
- Sober Living Homes: Transitional homes offer structured, substance-free environments where individuals can rebuild independence while maintaining sobriety.
- Temporary Housing Assistance: Community programs that provide temporary housing help stabilize individuals after treatment, reducing stress associated with housing insecurity.
9. Community Education and Anti-Stigma Campaigns
- Public Education Initiatives: Campaigns aimed at reducing addiction stigma educate the public on addiction as a treatable condition, fostering greater social acceptance.
- Anti-Stigma Events: Workshops for families and communities offer insights into supporting loved ones in recovery and creating a compassionate environment for individuals in treatment.
10. Family Support and Educational Resources
- Family Support Groups: Organizations like Al-Anon and Nar-Anon support families dealing with addiction by providing shared experiences, coping strategies, and resilience-building.
- Workshops for Families: Educational workshops help families understand the involuntary treatment process and equip them with tools for long-term support.
11. Aftercare Programs and Relapse Prevention
- Follow-Up Coordination: Aftercare programs provide ongoing support, including therapy appointments, relapse prevention planning, and regular medical check-ins.
- Relapse Prevention Tools: Community programs offer workshops and resources that help individuals identify triggers, develop coping strategies, and maintain recovery.
12. Financial Assistance and Grant Programs
- Aid for Low-Income Individuals: State grants and community charities offer financial assistance to those unable to cover treatment costs, such as therapy, medication, or transportation.
- Recovery Funding Programs: Certain communities provide dedicated funding for recovery services, allowing individuals to continue their treatment journey without financial hindrance.
Community resource strategies are invaluable for the success of involuntary treatment and long-term addiction recovery. By providing accessible addiction services, legal support, job training, mental health care, and family resources, community programs work together to create a robust support network. This integrated approach reduces relapse risks and offers individuals a pathway to recovery, dignity, and reintegration into society.
Self-Management Strategies to Prevent the Need for Involuntary Addiction Treatment
Self-management strategies are essential in helping individuals take control of their recovery, preventing addiction from escalating to the point where involuntary treatment becomes necessary. These strategies support long-term sobriety by building resilience, self-awareness, and practical skills. Here are some effective self-management approaches to help individuals stay on track in their recovery journey and avoid the need for crisis intervention:
1. Setting Clear Goals and Personal Boundaries
- Define Recovery Goals: Establishing clear, achievable goals—such as maintaining sobriety for a specific period or avoiding high-risk situations—helps individuals stay focused, motivated, and accountable.
- Establish Personal Boundaries: Setting firm boundaries, like avoiding certain people or places associated with substance use, can significantly reduce relapse risk and help individuals manage their environment.
2. Developing a Structured Routine
- Create Daily and Weekly Schedules: A well-structured routine incorporating work, self-care, exercise, and hobbies helps individuals stay busy and engaged, reducing time spent on addictive behaviors.
- Set Reminders for Healthy Habits. Regular exercise, meal planning, and sleep can significantly improve physical and mental health and prevent the return to harmful patterns.
3. Building Coping Skills for Stress and Triggers
- Practice Stress Management Techniques: Deep breathing, yoga, or mindfulness meditation can help individuals manage stress without using substances.
- Identify and Manage Triggers: By recognizing personal triggers—emotional, social, or environmental—individuals can proactively address them through therapy, journaling, or healthy coping strategies.
4. Engaging in Therapy and Counseling
- Participate in Regular Therapy: Therapy, such as cognitive-behavioral therapy (CBT), addresses underlying mental health issues like trauma or anxiety, helping individuals manage emotional challenges without substance use.
- Consider Group Counseling: Support groups like Alcoholics Anonymous (AA) or Narcotics Anonymous (NA) provide a sense of accountability, community, and shared experience, reinforcing one’s commitment to recovery.
5. Utilizing Support Networks
- Build a Strong Support System: Maintaining connections with supportive friends, family, or a sponsor can reduce feelings of isolation and offer practical support.
- Ask for Help When Needed: Reaching out for emotional or practical support before feeling overwhelmed can prevent a crisis and reduce the likelihood of needing involuntary treatment.
6. Practicing Mindfulness and Emotional Awareness
- Mindfulness Exercises: Techniques like meditation and grounding exercises improve self-awareness, helping individuals recognize cravings or emotional triggers before they escalate.
- Develop Emotional Resilience: Journaling, gratitude practices, and self-reflection can help process emotions, making it easier to resist the urge to use substances as a coping mechanism.
7. Focusing on Physical Health and Wellness
- Exercise Regularly: Physical activity reduces cravings and boosts mood and energy levels, helping individuals maintain emotional and physical health.
- Prioritize Sleep and Nutrition: Good sleep and nutrition are crucial in managing stress and maintaining a stable mood, reducing the risk of relapse.
8. Practicing Accountability and Self-Reflection
- Use Accountability Tools: Recovery journals and apps can help individuals track their progress, set reminders, and identify areas for improvement.
- Reflect on Consequences: Reminding oneself of the negative consequences of past substance use and the reasons for choosing recovery can strengthen motivation to stay sober.
9. Creating a Relapse Prevention Plan
- Develop a Relapse Prevention Plan: A personalized plan helps individuals anticipate high-risk situations and provides strategies to manage them, such as emergency contacts, coping techniques, or distractions.
- Establish a Plan for Setbacks: Accepting that setbacks may happen and having a plan to manage them can prevent a single lapse from escalating into a full relapse.
10. Learning and Growth through Recovery Programs
- Participate in Educational Programs: Workshops and recovery programs offer valuable insights into addiction, self-care, and emotional regulation, enhancing personal growth and resilience.
- Adopt a Lifelong Learner Mindset: Viewing recovery as an ongoing journey of growth encourages individuals to stay engaged and learn new skills to strengthen their ability to manage addiction.
11. Engaging in Meaningful Activities and Hobbies
- Find Activities That Bring Joy and Fulfillment: Engaging in hobbies or creative pursuits can help fill time, reduce stress, and improve self-esteem, making it easier to resist the lure of substances.
- Explore Volunteer Opportunities: Volunteering provides a sense of purpose, builds self-worth, and offers positive social connections, further motivating individuals to maintain healthy choices.
12. Practicing Self-Compassion and Resilience
- Practice Self-Compassion: It’s essential to practice self-compassion and avoid guilt or self-blame. A balanced, forgiving perspective encourages resilience when challenges arise.
- Build Resilience Through Setbacks: Recognizing that setbacks are a natural part of recovery helps individuals bounce back more quickly, preventing minor issues from escalating into crises that require involuntary treatment.
By adopting self-management strategies, individuals empower themselves to take control of their recovery and reduce the risk of addiction escalating to the point where involuntary treatment becomes necessary. Through goal setting, routine building, coping skills development, and seeking support, individuals can prevent relapse, enhance emotional resilience, and maintain long-term sobriety. These proactive strategies foster self-awareness, emotional stability, and independence, providing individuals with the tools to navigate addiction challenges and improve their quality of life.
Conclusion
Involuntary treatment for severe addiction presents a complex solution, balancing urgent intervention with challenges around autonomy and ethical considerations. While it can interrupt harmful behaviors and provide immediate care, the success of involuntary treatment often depends on the quality of support and resources provided by families and communities. These support systems help address practical and emotional needs, offering a foundation for long-term recovery. At the same time, self-management strategies are invaluable preventive measures, empowering individuals to take control of their recovery journey before a crisis arises. By understanding both the potential and limitations of involuntary treatment and supportive strategies, we can foster a more compassionate, comprehensive approach to addiction recovery.
Video: 5 Shocking Facts About Involuntary Rehab That Will Surprise You