Genetic-based therapy for addiction personalizes treatment by analyzing an individual’s genetic makeup, aiming to improve effectiveness through tailored interventions like pharmacogenomics. Driven by research on genetic influences in addiction, this approach offers potential benefits but also raises ethical concerns, privacy risks, and the challenge of overemphasizing genetics over psychological and social factors. While promising, its validity is still under study, making it a complementary tool rather than a standalone treatment.
The Future of Addiction Treatment: Genetics-Based Therapy
Genetic-based therapy for addiction focuses on utilizing a person’s genetic makeup to personalize and enhance treatment approaches. This innovative approach aims to improve treatment effectiveness by tailoring interventions to an individual’s unique biological factors. While still an evolving field, gene-based therapies offer several promising methods to treat addiction, including pharmacogenomics, genetic risk assessment, and even experimental gene therapy. By understanding these genetic influences, healthcare providers can create more targeted and effective treatment plans.
Pharmacogenomic Approaches: Personalized Medication
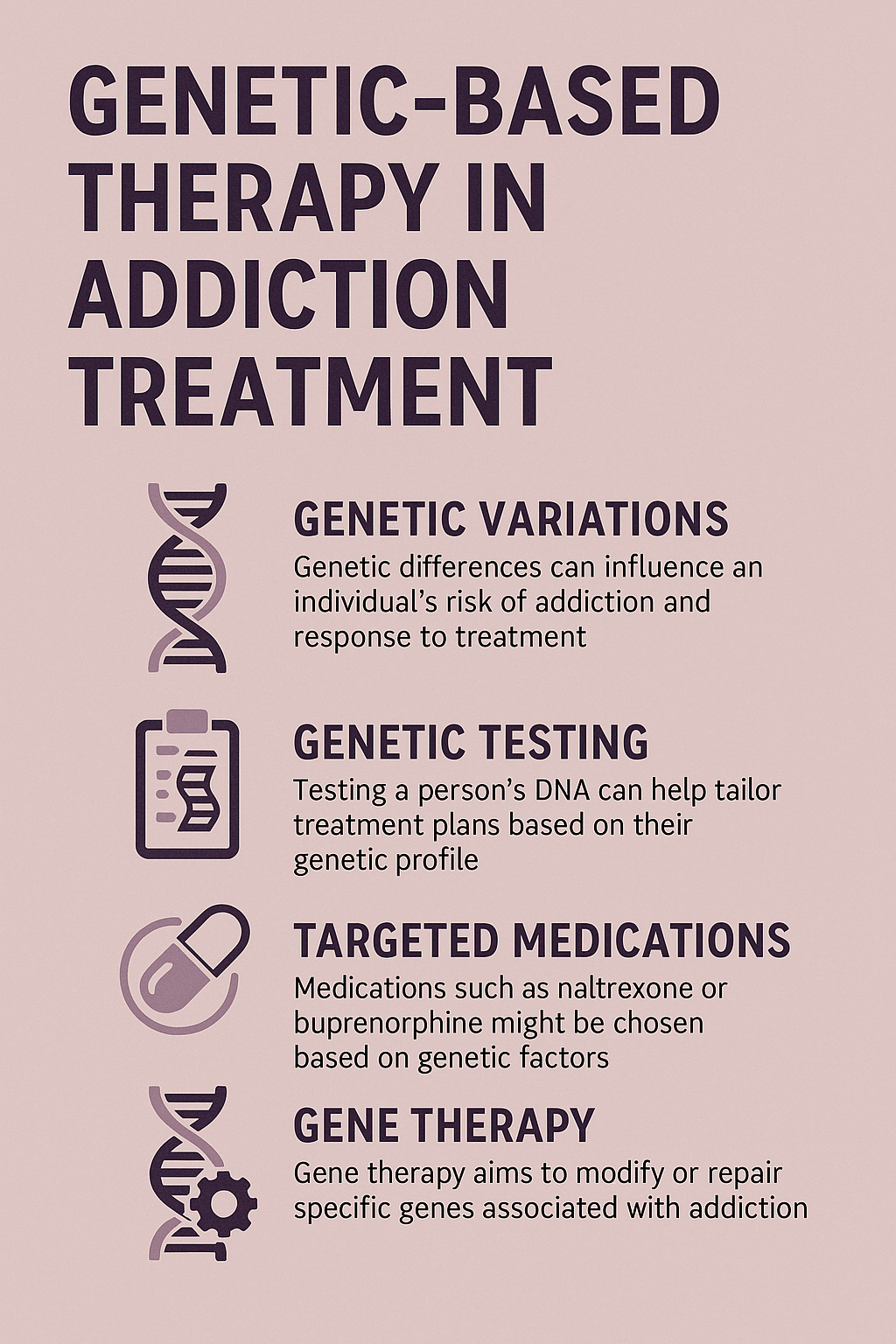
One of the most developed aspects of genetically based therapy is pharmacogenomics, which helps determine how individuals metabolize and respond to medications used in addiction treatment. Genetic testing can guide clinicians in choosing the most effective drugs, such as methadone, buprenorphine, or naltrexone, for opioid addiction. Additionally, it can help avoid medications that may cause harmful side effects, ensuring safer and more tolerable treatment options.
Identifying Genetic Predispositions to Addiction
Genetic research has identified specific markers that contribute to addiction susceptibility. Variations in genes related to dopamine receptors or serotonin pathways can indicate a higher risk for developing substance use disorders. By identifying these genetic predispositions, healthcare providers can implement early interventions, tailor treatment strategies, and focus on substances that pose the highest risk for an individual.
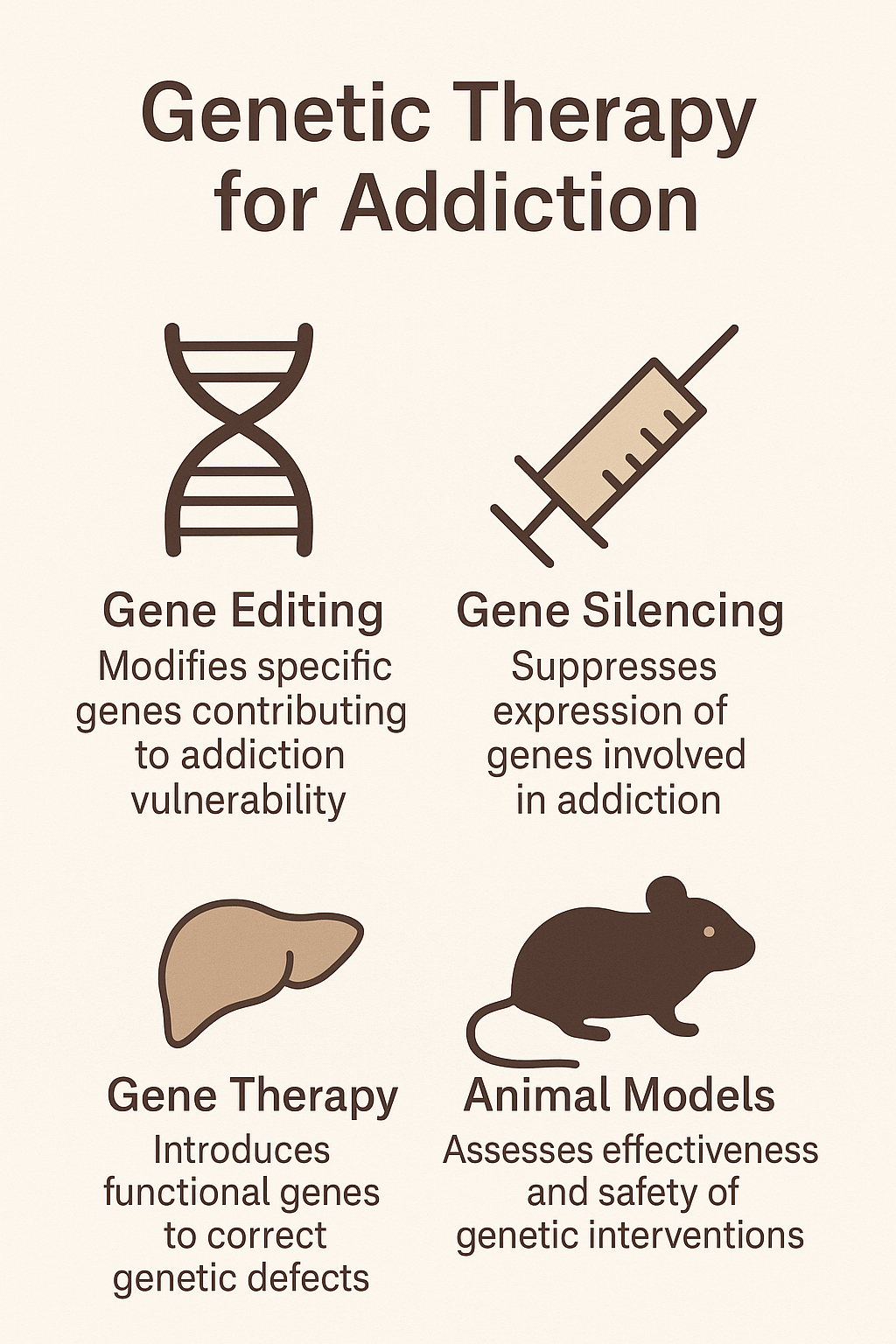
Gene Therapy: An Experimental Approach
Though still in its research phase, gene therapy presents a groundbreaking potential for addiction treatment. Scientists are exploring how modifying genes that influence dopamine signaling might reduce cravings and compulsive substance use. Technologies like CRISPR could allow for precise genetic modifications, potentially reducing an individual’s susceptibility to addiction.
Genetic Counseling and Education
Genetic counseling plays a crucial role in addiction treatment by educating individuals about their genetic risks and helping them make informed decisions regarding their treatment. This knowledge can motivate patients to adhere to treatment plans and adopt personalized behavioral therapies. For instance, individuals with genetic predispositions to anxiety or depression may benefit from tailored mental health interventions alongside addiction treatment.
Improving Treatment Adherence and Outcomes
Genetic insights can also predict relapse risk, allowing for proactive treatment adjustments. Certain genetic variations related to stress response and reward processing can indicate a higher likelihood of relapse. By recognizing these factors, healthcare providers can implement targeted relapse-prevention strategies, such as additional therapies or medication-assisted treatments, to improve recovery outcomes.
Preventive Interventions
Early genetic screening for addiction susceptibility enables preventive measures before a substance use disorder develops. Personalized prevention strategies may include lifestyle modifications, education on addiction risks, and behavioral interventions. Additionally, understanding genetic risks can help adjust environmental factors, reducing triggers and stressors that may lead to substance abuse.
In summary, genetics-based addiction therapy offers a promising future for personalized and effective treatment strategies. By leveraging genetic insights, healthcare providers can make informed decisions about medication choices, behavioral interventions, and relapse prevention strategies. While still an evolving field, gene-based therapy has the potential to revolutionize addiction treatment, ultimately leading to better outcomes and a more comprehensive approach to recovery.
The Advantages of Genetic-Based Therapy in Addiction Treatment
Therapy is increasingly shifting toward gene-based approaches due to advancements in genetic research, technology, and a better understanding of the complex interplay between genes, behavior, and the environment. This shift aims to provide more personalized, effective, and targeted treatments for addiction. Genetic-based therapy enhances treatment outcomes by tailoring interventions to an individual’s genetic profile, ultimately improving recovery success rates.
Understanding the Genetic Basis of Addiction
Genetics plays a significant role in addiction vulnerability. Certain genetic traits increase the likelihood of developing substance use disorders (SUDs). By integrating genetic data into therapy, healthcare providers can identify at-risk individuals, allowing for earlier interventions and more effective prevention strategies. Additionally, understanding biological mechanisms, such as variations in the dopamine and serotonin systems, enables the development of targeted therapies.
Personalized Treatment for Better Outcomes
Traditional addiction treatments often follow a standardized model, which may not work for everyone. Genetic-based therapy allows for individualized treatment by considering how a person’s genetic makeup influences their response to medications and therapies. Pharmacogenomic testing can determine the most effective medicines for each patient, reducing trial and error and minimizing adverse side effects.
Improving Treatment Success and Adherence
By tailoring treatments to genetic profiles, genetic-based therapy enhances the effectiveness of addiction treatments. Personalized therapies increase treatment adherence by selecting medications and interventions that are better tolerated. Patients are more likely to commit to recovery plans when treatments align with their genetic predispositions, leading to higher success rates.
Identifying Co-occurring Disorders and Environmental Interactions
Many individuals with addiction also struggle with mental health disorders. Genetic testing can reveal predispositions to both addiction and co-occurring mental health conditions, allowing for comprehensive treatment strategies. Additionally, recognizing the interaction between genetic and environmental factors helps healthcare providers develop holistic treatment plans that address both biological and social influences.
Reducing Relapse Rates with Genetic Insights
Genetic factors influence relapse risk by affecting cravings, stress responses, and reward-seeking behavior. Identifying individuals with a higher genetic risk for relapse enables healthcare providers to implement personalized relapse prevention strategies, such as additional support, behavioral interventions, or specific medications tailored to their needs.
Advances in Genetic Testing and Technology
With advancements in genetic testing, genome-wide association studies (GWAS), and reduced testing costs, genetic insights are becoming more accessible in clinical settings. These technological advancements enable more precise and science-driven addiction therapies, allowing for widespread integration of genetic-based treatments.
A Holistic Approach to Addiction Treatment
Genetic-based therapy supports the evolving perspective of addiction as a chronic, relapsing brain disease rather than just a behavioral issue. This approach aligns with the growing emphasis on holistic treatment, considering both genetic and environmental factors to provide individualized care and long-term recovery strategies.
As our understanding of addiction deepens, gene-based therapy is emerging as a powerful tool in personalized treatment. By leveraging genetic insights, healthcare providers can create targeted, effective treatment plans that improve outcomes and reduce relapse rates. While still evolving, genetic-based therapy represents the future of addiction treatment, offering a scientific, individualized approach to recovery.
The Disadvantages and Ethical Dilemmas of Genetic-Based Addiction Therapy
Genetic-based addiction therapy offers promising advancements in personalized treatment, but it also presents significant risks and ethical concerns. While the potential for tailoring interventions based on genetic predispositions is compelling, issues such as privacy, misuse of genetic information, accessibility, and incomplete scientific knowledge must be carefully examined. This blog explores the key disadvantages and ethical dilemmas associated with genetic-based addiction therapy.
1. Privacy and Confidentiality Issues
Genetic testing generates sensitive personal data, raising concerns about security and misuse. If leaked, this information could result in discrimination in employment or insurance. Additionally, patients may struggle to understand the implications of genetic testing fully, necessitating clear communication and stringent data protection policies.
2. Genetic Determinism and Stigma
There is a risk that gene-based therapy will overemphasize the role of genes in addiction, potentially leading to a deterministic view. Individuals informed of a genetic predisposition to addiction may experience fatalism, feeling powerless against their genetic makeup. This could reduce motivation for behavioral change and contribute to societal stigma surrounding addiction.
3. Potential Misuse of Genetic Information
Genetic data could be exploited in ways that harm individuals. Employers or insurers might discriminate against those with a predisposition to addiction, limiting their opportunities. Additionally, healthcare providers may rely too heavily on genetic data when designing treatment plans, potentially overlooking a patient’s personal experiences and environmental influences.
4. Access and Equity Concerns
Genetic-based therapies may be financially inaccessible for many, widening the gap between those who can afford personalized treatment and those who cannot. Over-reliance on genetic technology could also divert resources from more traditional, evidence-based addiction treatments that are currently accessible to a broader population.
5. Incomplete or Inaccurate Genetic Understanding
The science of genetic addiction therapy remains in its early stages. While specific genetic markers have been linked to addiction, they do not paint a complete picture. Genetic tests may produce false positives or negatives, leading to misleading conclusions about an individual’s risk or appropriate treatment plan.
6. Ethical Concerns
Genetic testing in minors presents serious ethical questions, particularly regarding informed consent and the potential psychological burden. There is also the risk of genetic discrimination, where individuals face bias based on their genetic predisposition to addiction. Furthermore, emerging gene-editing techniques like CRISPR carry the risk of unforeseen consequences and long-term side effects.
7. Risk of Treatment Ineffectiveness or Over-Reliance on Medication
While genetic insights can guide addiction therapy, they do not account for the full spectrum of factors influencing addiction. Relying solely on genetically based treatment methods without addressing social and psychological aspects may result in ineffective care. Additionally, excessive focus on pharmacological interventions tailored to genetic profiles could overshadow the importance of holistic recovery approaches.
8. Psychological and Social Impact
Learning about one’s genetic susceptibility to addiction may cause emotional distress, anxiety, or depression. Furthermore, genetic information can impact family dynamics, as individuals may feel compelled to share—or hide—their genetic risks from relatives, potentially leading to difficult ethical and emotional decisions.
While genetic-based addiction therapy offers innovative possibilities, it also raises significant concerns that must be addressed. Privacy, ethical considerations, access disparities, and the limitations of genetic science all pose challenges that require careful navigation. Moving forward, it is crucial to integrate genetic insights with traditional therapeutic approaches, ensuring that addiction treatment remains comprehensive, ethical, and accessible to all individuals.
The Validity of Genetics-Based Therapy in Addiction Treatment
Genetic-based therapy for addiction treatment is an evolving field, offering the promise of personalized treatment. While there are promising advancements, it has not yet become a fully validated or widely accepted approach. There are both the potential and the limitations of genetically based addiction therapy.
Promising Aspects of Genetics-Based Therapy for Addiction
Genetic Insights into Addiction Risk
Research has identified genetic markers associated with addiction susceptibility. Variations in dopamine receptors (e.g., DRD2) have been linked to a higher risk of substance use disorders (SUDs). Understanding genetic predispositions could allow for early interventions and tailored prevention strategies.
Pharmacogenomics – Tailored Medications
One of the most validated aspects of genetic therapy is pharmacogenomics, which helps determine how individuals metabolize medications. Genetic testing can enhance the effectiveness of addiction treatments like methadone, buprenorphine, and naltrexone, reducing the trial-and-error approach in medication selection.
Behavioral and Psychological Factors
Genetic research helps explain the neurobiological mechanisms behind addiction, improving behavioral therapies. For example, personalized approaches may focus on reducing cravings or modulating dopamine levels in individuals with genetic predispositions.
Gene-Environment Interactions
Both genetic and environmental factors influence addiction. Genetic-based therapy, when integrated with lifestyle and behavioral interventions, could provide a more comprehensive approach to addiction treatment.
Limitations and Challenges to Genetic-Based Therapy for Addiction
Incomplete Understanding of Genetic Factors
Despite progress, the full genetic basis of addiction remains unclear. Addiction is polygenic, meaning multiple genes contribute in small ways, making it challenging to pinpoint definitive genetic causes. Genetic tests currently available provide only partial insights.
Limited Availability of Tailored Treatments
While pharmacogenomics can guide medication selection, genetically based addiction treatments are not widely available. Most treatment programs still rely primarily on behavioral therapies and support systems.
Ethical and Social Concerns
Genetic determinism could lead to stigma or fatalism, in which individuals believe their genetic predisposition determines their fate. Additionally, concerns over genetic privacy and potential misuse by employers or insurance companies pose ethical challenges.
Risk of Over-Emphasis on Genetics
Focusing too heavily on genetic factors risks neglecting environmental and psychosocial influences. Addiction treatment remains most effective when it incorporates counseling, social support, and behavioral therapies alongside genetic insights.
Current Clinical Use and Future Potential
Current Clinical Use
Genetic-based therapies currently serve as a complementary tool rather than a standalone treatment. Pharmacogenomic testing is used in some settings to personalize medication prescriptions, but holistic treatment approaches remain central to addiction care.
Future Potential
As research advances, gene-based therapy may become more integrated into addiction treatment. Future applications could include identifying high-risk individuals early, refining personalized interventions, and potentially developing gene-editing therapies—though these remain speculative at present.
In summary, the validity of genetic-based addiction therapy is promising but still in its early stages. While pharmacogenomics has shown practical benefits, the broader application of genetic insights into addiction treatment remains a work in progress. As research advances, gene-based therapies may become more integral to personalized addiction treatment, but for now, they serve best as a supplementary tool within a comprehensive approach.
Frequently Asked Questions
Here are some common questions:
Question: What genetic therapy examples help with addiction?
Answer: Genetic therapy for addiction is still in the early stages of research, but several promising approaches are being explored. Here are some examples of genetically based therapies that have shown potential in treating substance use disorders (SUDs):
1. Gene Editing (CRISPR) for Addiction Treatment
- Targeting Dopamine Receptors (D1/D2 Pathways)
- Researchers are exploring CRISPR-based techniques to modify genes associated with dopamine signaling, such as DRD2, which influences reward and reinforcement mechanisms.
- By modifying these pathways, scientists aim to reduce the reinforcing effects of addictive substances like opioids, alcohol, and stimulants.
- Reducing Opioid Cravings via Gene Silencing
- Studies have looked at silencing the Mu-opioid receptor (OPRM1) gene, which mediates the pleasurable effects of opioids. By modifying this gene, it may be possible to reduce opioid dependence and cravings.
2. Viral Vector Gene Therapy
- Alcohol Use Disorder (AUD) – Modifying Dopamine and Serotonin Pathways
- Some experimental studies have used viral vectors to introduce or suppress genes involved in alcohol addiction. For example, increasing the expression of genes related to serotonin regulation (such as TPH2) could help modulate mood and cravings.
- Glial Cell Line-Derived Neurotrophic Factor (GDNF) Therapy for Alcoholism and Cocaine Addiction
- GDNF is a neurotrophic factor that supports neuronal survival and has been studied as a potential target for gene therapy.
- Animal studies suggest that increasing GDNF levels in the brain reduces alcohol and cocaine consumption by altering reward pathways.
3. Pharmacogenomics – Tailoring Medications Based on Genetics
- Personalized Treatment for Opioid Use Disorder (OUD)
- Genetic testing can identify variations in genes such as OPRM1 (the opioid receptor gene) and CYP450 enzymes that affect how a person responds to medications such as methadone, buprenorphine, or naltrexone.
- By using genetic information, doctors can tailor medication-assisted treatment (MAT) to improve effectiveness and reduce side effects.
- Nicotinic Receptor Genes (CHRNA5) and Smoking Cessation
- Genetic variations in CHRNA5 (which encodes a nicotinic acetylcholine receptor subunit) influence nicotine dependence and response to smoking cessation medications like varenicline.
- Pharmacogenomics studies are helping develop more effective, personalized nicotine addiction treatments.
4. Epigenetic Therapy for Addiction
- Targeting DNA Methylation and Histone Modification
- Addiction alters gene expression through epigenetic changes (modifications that affect gene activity without changing the DNA sequence).
- Researchers are exploring drugs that can reverse these changes by modulating DNA methylation and histone acetylation, which could help “reset” the brain’s response to medication and cravings.
5. Experimental Gene Therapy for Opioid Addiction
- Enzyme-Based Therapy to Block Opioid Effects
- Scientists are working on gene therapy approaches to introduce synthetic enzymes that break down opioids in the bloodstream before they reach the brain.
- This method could function like a “biological vaccine” against opioid overdose by preventing the drug from having its usual euphoric effects.
Future Directions
- Gene Therapy for Reward System Modulation
- Future gene therapy research may focus on modifying genes related to dopamine and glutamate signaling to help individuals with addiction regain normal brain function.
- Genetic Protection Against Addiction
- Some studies are exploring whether genetic modifications could make individuals less susceptible to addiction before it starts.
While gene therapy for addiction is still in the experimental phase, advancements in CRISPR, viral vector delivery, pharmacogenomics, and epigenetics offer promising avenues for developing more effective, personalized treatments. These approaches could revolutionize addiction treatment by targeting the biological mechanisms underlying substance dependence.
Question: What government policies would help genetic therapy evolve into part of medical treatment?
Answer: Government policies play a crucial role in the advancement and integration of genetic therapy into mainstream medical treatment. Several key policy areas can help genetically-based therapies, including those for addiction, evolve into widely accepted medical treatments. Here are some of the most impactful policies:
1. Research Funding and Grants
- Increased NIH and FDA Funding for Genetic Research
- Governments can expand funding for agencies like the National Institutes of Health (NIH) and the Food and Drug Administration (FDA) to support research on genetically based therapies.
- Specific funding programs for addiction-related genetic therapy could accelerate breakthroughs in personalized medicine.
- Public-Private Partnerships
- Governments can collaborate with private biotech firms and academic institutions to create innovation hubs focused on genetic medicine.
2. Regulatory Frameworks for Genetic Therapies
- Accelerated FDA Approval Pathways
- Policies that streamline the approval of genetically based therapies (such as expedited review processes under the FDA’s Breakthrough Therapy Designation) could bring safe treatments to market faster.
- Establishing Clear Guidelines for Gene Therapy in Addiction Treatment
- Regulatory bodies need to develop specific frameworks for gene therapy in addiction treatment to ensure safety, efficacy, and ethical compliance.
- Monitoring Long-Term Effects of Genetic Treatments
- Policies requiring long-term safety monitoring of genetic therapies would help address risks and build public trust.
3. Insurance Coverage and Healthcare Integration
- Expanding Medicare/Medicaid Coverage for Genetic Testing & Therapy
- Government policies can mandate insurance providers, including Medicare and Medicaid, to cover genetic testing for addiction risk and personalized pharmacogenomic treatments.
- Reimbursement Policies for Genetic Therapy
- New billing codes and reimbursement models can be introduced for genetically-based treatments to ensure they are financially viable for both patients and healthcare providers.
4. Ethical and Privacy Protections
- Strengthening Genetic Data Privacy Laws
- Expanding protections under laws such as the Genetic Information Nondiscrimination Act (GINA) would prevent employers or insurers from misusing genetic data.
- Informed Consent Regulations
- Governments can require strict informed consent policies to ensure patients fully understand the risks and benefits of genetic therapy before undergoing treatment.
- Ethical Oversight Committees
- Policies establishing national or international ethics review boards can ensure that genetic therapies align with human rights and medical ethics.
5. Education and Public Awareness
- Government-Backed Public Education Campaigns
- Increasing public awareness about the benefits and limitations of genetic therapy would help reduce skepticism and stigma around these treatments.
- Training for Healthcare Providers
- Policies can mandate training programs for doctors and addiction specialists to incorporate genetic testing and therapy into routine medical practice.
6. Incentives for Biotech Companies
- Tax Credits for Genetic Research & Development (R&D)
- Governments can offer tax breaks and incentives for pharmaceutical companies and biotech startups working on genetic therapy.
- Patent Protection & Licensing Policies
- Establishing balanced patent laws can encourage innovation while ensuring genetic therapies remain accessible and affordable.
7. Global Collaboration and Data Sharing
- International Regulatory Cooperation
- Harmonizing regulations across countries (e.g., through the World Health Organization (WHO) or the European Medicines Agency (EMA)) can accelerate the global adoption of genetically-based therapies.
- Open-Source Genetic Research Databases
- Governments can support shared databases for genetic research to accelerate discovery while protecting patient confidentiality.
For genetic therapy to become a mainstream part of medical treatment—including addiction therapy—governments must implement comprehensive policies that support research, ensure affordability, protect patient rights, and streamline regulatory approval. Balancing innovation with ethical safeguards will be key to successfully integrating gene-based therapies into everyday healthcare.
Question: What specific government policies in the US are in place to integrate genetic therapy into medical treatment?
Answer: The United States government has implemented several policies to integrate genetic therapies into mainstream medical treatment:
1. Regenerative Medicine Advanced Therapy (RMAT) Designation
Established under the 21st Century Cures Act, the RMAT designation by the FDA accelerates the development and approval of regenerative medicine therapies, including gene therapies. This program allows for expedited approval based on surrogate or intermediate clinical endpoints, facilitating faster patient access to innovative treatments.
2. National Center for Advancing Translational Sciences (NCATS)
Part of the National Institutes of Health (NIH), NCATS focuses on transforming scientific discoveries into health interventions. By supporting translational research, NCATS plays a pivotal role in advancing gene therapies from the laboratory to clinical application.
3. Bespoke Gene Therapy Consortium (BGTC)
The BGTC is a collaborative effort involving the NIH, FDA, non-profit organizations, and pharmaceutical companies. It aims to streamline the development of gene therapies for rare diseases by addressing challenges in manufacturing and regulatory processes.
4. Outcomes-Based Agreements for Gene Therapies
The Centers for Medicare & Medicaid Services (CMS) has entered into outcomes-based agreements with companies like Vertex Pharmaceuticals and bluebird bio. These agreements link reimbursement to the effectiveness of gene therapies, ensuring both access and value in patient care.
5. Accelerated Approval Pathways
The FDA offers accelerated approval pathways for therapies addressing severe conditions with unmet medical needs. For instance, uniQure’s gene therapy for Huntington’s disease, AMT-130, is undergoing testing under such an agreement, potentially expediting its availability to patients.
These policies collectively foster the development, evaluation, and integration of genetic therapies into medical practice, enhancing treatment options for various diseases.
Conclusion
Genetic-based therapy for addiction offers a promising step toward personalized treatment by leveraging genetic insights to improve effectiveness, particularly in medication response. While it holds potential for tailored interventions, it also presents ethical concerns, privacy risks, and the challenge of balancing genetic factors with psychological and social influences. Although research continues to explore its full validity, genetic-based therapy is not yet a standalone solution but rather a complementary tool within a broader, holistic approach to addiction treatment.
Video: Top Geneticist Reveals Breakthrough in Personalized Addiction Treatment
What If Genes Could Beat Addiction?