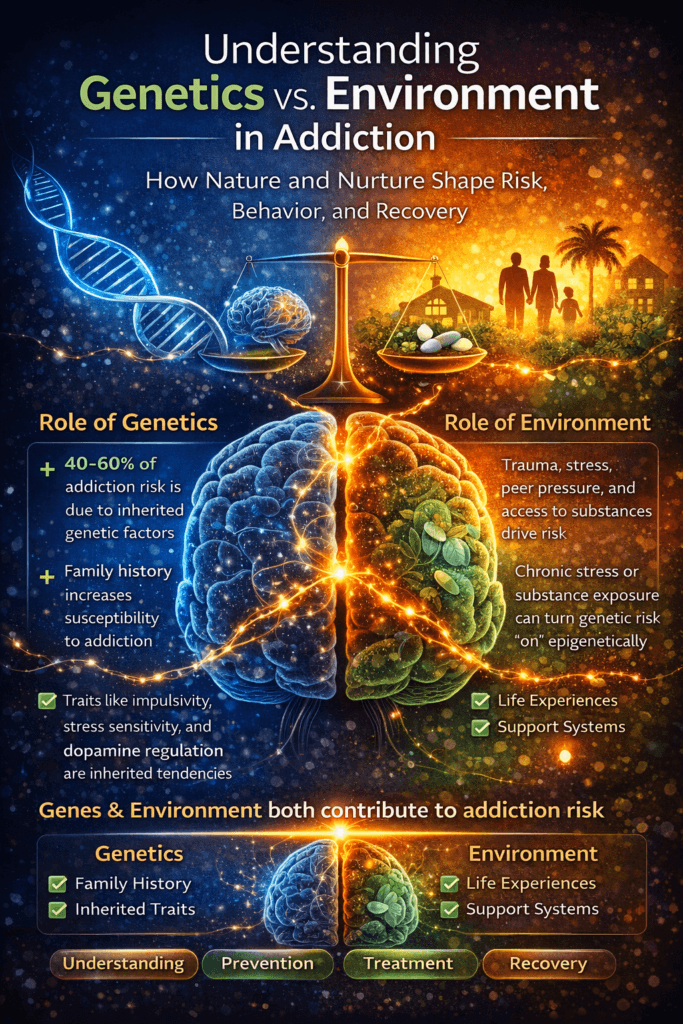
Addiction is best understood through the combined influence of genetics and environment rather than one or the other alone. Genetic factors can increase vulnerability by shaping how the brain responds to reward, stress, and impulse control, while environmental influences—such as trauma, family dynamics, social exposure, and access to substances—determine how that vulnerability is expressed. Understanding this interaction helps explain why addiction affects individuals differently and why risk is never fixed. It also shifts the conversation away from blame and toward informed prevention, treatment, and recovery.
Genetics vs. Environment in Addiction: Nature, Nurture, and the Brain
Addiction is often framed as a debate between genetics and environment—nature versus nurture—but modern science shows that it is the interaction between the two that truly shapes risk. Neither genetics nor environment alone determines whether someone will develop an addiction. Instead, addiction emerges from how inherited vulnerabilities intersect with life experiences, stressors, and exposures over time.
Genetics plays a significant role in addiction risk. Research suggests that roughly 40–60% of a person’s vulnerability to addiction is heritable. This does not mean there is a single “addiction gene.” Rather, multiple genes influence traits such as impulsivity, stress sensitivity, dopamine signaling, and the brain’s response to substances. A family history of addiction increases risk, not because addiction is inevitable, but because certain brain and behavioral traits can be passed down.
The environment is the other major force shaping addiction. Early life experiences, trauma, parenting style, peer influence, availability of substances, socioeconomic stress, and cultural norms all affect how the brain develops and copes with reward and stress. Chronic stress, neglect, or exposure to substance use—especially during childhood or adolescence—can prime the brain’s reward system to seek relief through external substances or behaviors.
The key bridge between genetics and environment is epigenetics. Environmental experiences can influence gene expression without altering the DNA sequence. Trauma, stress, substance exposure, and even positive factors like stable relationships or therapy can turn certain genes “on” or “off.” This means that genetic risk is not fixed; it is continuously shaped by lived experience.
Timing also matters. The adolescent brain is particularly sensitive to environmental influences because the reward system develops faster than the brain’s impulse-control mechanisms. Substance exposure during this period can strongly reinforce addictive pathways, especially in individuals with genetic vulnerability. Conversely, protective environments—supportive families, stable routines, and healthy coping skills—can significantly reduce risk, even in those with a strong genetic predisposition.
Understanding addiction as the result of genetics interacting with the environment reduces stigma and blame. It explains why two people can experience the same substance very differently, and why recovery requires more than simply removing the drug. Effective prevention and treatment focus on both sides of the equation: supporting brain health, addressing trauma and stress, strengthening coping skills, and creating environments that promote safety, connection, and purpose.
Addiction is not destiny. Genes may load the gun, but environment pulls—or restrains—the trigger. With the right supports, individuals can change the trajectory of risk, heal the brain, and build lasting recovery regardless of their genetic starting point.
Self-Management Strategies for Understanding Genetics vs. Environment in Addiction
Understanding the balance between genetics and environment can be empowering in addiction recovery. Many people feel discouraged when they learn addiction can run in families, but genetic risk is not destiny. Self-management strategies help individuals recognize inherited vulnerabilities and actively shape their environment to reduce risk and support long-term recovery.
A key self-management step is developing self-awareness. Knowing personal risk factors—such as family history, impulsivity, stress sensitivity, or mood instability—allows individuals to plan proactively. This awareness shifts thinking from “What’s wrong with me?” to “What do I need to manage differently?” Self-monitoring triggers, emotional states, and early warning signs helps interrupt patterns before they escalate.
Stress regulation is especially important for those with genetic vulnerability. Chronic stress can activate inherited risk pathways related to dopamine and reward seeking. Daily stress-management practices—such as exercise, mindfulness, structured routines, and relaxation techniques—reduce environmental pressure on the brain and lower the drive toward substances or compulsive behaviors.
Shaping one’s environment is another powerful strategy. This includes limiting exposure to high-risk situations, substances, or social settings that normalize use. Replacing these with recovery-supportive spaces—safe housing, sober social activities, healthy hobbies, and structured schedules—helps counterbalance genetic risk. Small environmental changes, practiced consistently, can significantly alter outcomes.
Building adaptive coping skills further reduces environmental impact. Skills such as problem-solving, emotion regulation, assertive communication, and delay of gratification strengthen the brain’s control systems. These skills are particularly important when genetic traits, such as impulsivity or emotional reactivity, are present.
Self-management also involves reframing beliefs about genetics. Instead of viewing family history as a sentence, it can be used as information. Understanding risk enables individuals to remain vigilant, seek support early, and prioritize recovery behaviors. Education about addiction as a brain-based condition reduces shame and increases motivation to engage in healthy routines.
Finally, consistency matters more than perfection. Genetics influence vulnerability, but daily choices shape expression. Through intentional self-management—awareness, stress regulation, environment design, and coping skill development—individuals can actively reduce risk, support brain healing, and build a recovery path that reflects resilience rather than inheritance.
Family Support Strategies for Understanding Genetics vs. Environment in Addiction
Families play a critical role in shaping how genetic vulnerability and environmental factors interact in addiction. While genetics may increase susceptibility, the family environment often determines whether that risk is activated or buffered. Understanding this balance helps families move away from blame and toward supportive, informed action.
One of the most important family strategies is education. When families understand that addiction involves both inherited risk and environmental influence, shame and judgment tend to decrease. Learning about genetics helps families recognize that addiction is not a moral failure, while understanding environmental factors highlights how daily interactions, stress levels, and communication patterns affect recovery.
Creating a stable and predictable home environment is especially protective. Consistent routines, clear expectations, and reduced chaos help regulate stress and support brain healing. For individuals with genetic vulnerability, emotional unpredictability, or conflict, these factors can amplify risk. Families that prioritize calm, structure, and reliability provide a powerful protective buffer.
Supportive communication is another key strategy. Families that use nonjudgmental language, avoid labeling, and focus on behaviors rather than character reduce emotional stress. Open conversations about triggers, stress, and progress help individuals feel safe discussing challenges early—before relapse risk escalates. Feeling understood and supported can counteract inherited sensitivity to stress or impulsivity.
Families also benefit from examining their own patterns. Intergenerational behaviors—such as coping with stress through avoidance, conflict, or substance use—can unintentionally reinforce environmental risk. By modeling healthy coping, emotional regulation, and help-seeking behavior, families actively change the environment and interrupt cycles that may have persisted across generations.
Clear boundaries are equally essential. Boundaries protect both the individual in recovery and the family system from enabling behaviors. When boundaries are consistent and compassionate, they reduce confusion and stress while reinforcing accountability. This structured environment helps individuals with genetic risk develop stronger self-regulation skills.
Finally, families should seek support for themselves. Family therapy, support groups, and education programs help relatives process fear, guilt, or frustration without projecting it onto the person in recovery. A well-supported family creates a healthier environment—one that can significantly reduce the impact of genetic vulnerability and promote lasting recovery.
When families understand the relative roles of genetics and environment, they gain power. By shaping a stable, supportive, and informed environment, families can help transform genetic risk into an opportunity for resilience, growth, and long-term healing.
Community Resource Strategies for Understanding Genetics vs. Environment in Addiction
Community resources play a vital role in helping individuals and families understand how genetics and environment interact in addiction. While genetic vulnerability may increase risk, communities shape the environments that either activate that risk or protect against it. Education, access to care, and supportive social structures can dramatically change outcomes—even for those with strong family histories of addiction.
One of the most powerful community strategies is public education. Community workshops, prevention programs, schools, and healthcare systems that teach addiction as a brain-based condition help reduce stigma and misinformation. When people understand that genetics influences vulnerability but does not determine destiny, they are more likely to seek help early and engage in prevention rather than denial.
Accessible treatment and mental health services are another critical factor. Counseling, medication-assisted treatment, trauma-informed care, and integrated primary care address environmental stressors that can trigger genetic risk. By treating co-occurring conditions like anxiety, depression, or chronic pain, communities reduce the pressure that often drives substance use in genetically vulnerable individuals.
Peer support and recovery communities also play a key role. Support groups, recovery centers, and peer coaching offer shared understanding and real-life examples of resilience. Seeing others with similar backgrounds succeed in recovery reinforces the idea that genetics is not fate. These environments promote accountability, connection, and hope—powerful protective factors against addiction.
Community policies and infrastructure also matter. Safe housing, employment programs, recovery-friendly workplaces, and sober living environments reduce chronic stress and instability. Since stress is a major environmental trigger for addiction, especially among those with inherited vulnerability, these supports directly lower risk and support long-term recovery.
Prevention-focused community efforts are equally important. Youth programs, mentorship, after-school activities, and trauma-informed schools help shape healthy coping skills early in life. By strengthening protective environments during critical developmental stages, communities can reduce the likelihood that genetic risk will manifest later in life.
Finally, community-based family and caregiver resources amplify impact. Family education programs, support groups, and counseling help entire systems understand intergenerational patterns and interrupt cycles of addiction. When communities support families—not just individuals—they create environments that promote intergenerational healing.
Understanding genetics versus environment at a community level shifts addiction from a private struggle to a shared responsibility. Through education, access, structure, and compassion, communities can transform genetic vulnerability into resilience and build pathways to recovery that are inclusive, sustainable, and hopeful.
Frequently Asked Questions
Here are some common questions:
1. Is addiction genetic?
Addiction has a genetic component, but it is not caused by a single “addiction gene.” Research suggests that about 40–60% of addiction risk may be heritable, meaning genetics influence vulnerability—not destiny.
2. If addiction runs in my family, will I develop it?
Not necessarily. A family history increases risk, but environmental factors such as stress, trauma, peer influence, and access to substances play a major role in whether addiction develops.
3. What environmental factors increase addiction risk?
Common factors include childhood trauma, chronic stress, unstable housing, peer substance use, early exposure to drugs or alcohol, and lack of social support.
4. How do genetics influence addiction?
Genes can affect how the brain responds to dopamine, stress, impulse control, and reward. Some individuals may experience stronger cravings or reduced sensitivity to natural rewards.
5. What is epigenetics in addiction?
Epigenetics refers to how life experiences can turn certain genes “on” or “off” without changing DNA. Trauma, stress, and substance exposure can influence gene expression over time.
6. Can a healthy environment reduce genetic risk?
Yes. Supportive families, strong coping skills, education, stable housing, and positive peer networks can significantly reduce the likelihood that genetic vulnerability will be expressed.
7. Are adolescents at higher risk?
Yes. The adolescent brain continues to develop, particularly in regions associated with impulse control. Early substance exposure can increase long-term addiction risk, particularly in those with genetic vulnerability.
8. Does understanding genetics reduce stigma?
Absolutely. Recognizing addiction as influenced by biology and environment shifts the narrative away from moral failure and toward medical and social understanding.
9. Can someone change their addiction risk?
While genes cannot be changed, behavior and environment can. Healthy routines, stress management, therapy, and strong social support reduce overall risk and support recovery.
10. Why is it important to understand both genetics and environment?
Understanding both helps individuals, families, and communities focus on prevention and early intervention rather than blame. Addiction risk is shaped by interaction—not fate.
Conclusion
Recognizing the interplay between genetics and environment empowers individuals, families, and communities to take meaningful action. While genetics may influence risk, environment shapes outcomes—and environments can be changed. Through awareness, education, supportive relationships, and access to effective resources, genetic vulnerability can be buffered rather than activated. Understanding genetics versus environment reframes addiction as a modifiable, treatable condition and reinforces a hopeful message: risk is not destiny, and recovery is possible at every stage.
Video: Genes May Predispose, But You Choose Recovery #addictionscience #hope