Fetal abnormalities related to addiction develop when alcohol, drugs, or nicotine interfere with the delicate processes of fetal organ formation, brain development, and placental function during pregnancy. These substances cross the placenta and disrupt blood flow, oxygen delivery, and nutrient absorption, thereby impairing cell growth and tissue development. As a result, infants may face complications such as low birthweight, congenital defects, neonatal abstinence syndrome, preterm birth, and long-term cognitive or behavioral delays. Preventing these outcomes requires a comprehensive and coordinated approach that supports both maternal health and fetal safety. When pregnant women engage in self-management strategies, receive strong family encouragement, and have access to consistent prenatal care and community-based treatment services, the risks associated with substance exposure decline significantly. With compassionate medical guidance and stable support systems, mothers are better equipped to protect their pregnancies, giving their babies a healthier and more secure start in life.
Addiction & Fetal Abnormalities: Risks to Fetal Development
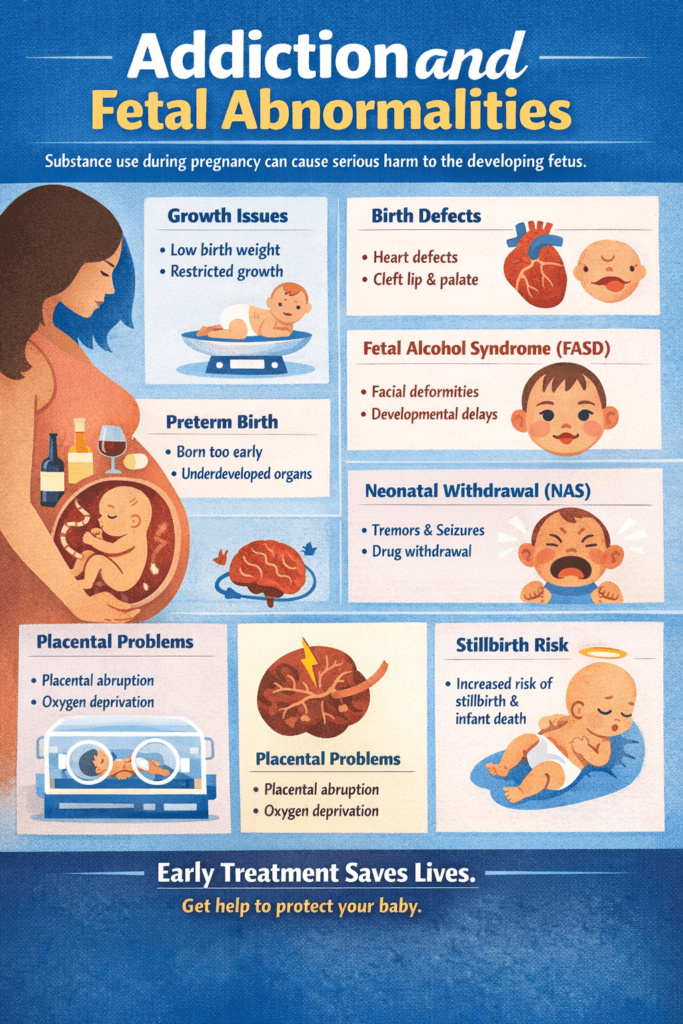
Substance use during pregnancy is a serious public health concern that can interfere with normal fetal development and lead to long-term health consequences for the child. Alcohol, tobacco, opioids, stimulants, cannabis, and misused prescription drugs can cross the placenta, disrupting the formation of organs, brain structures, and essential body systems. These exposures increase the risk of fetal growth restriction, congenital defects, neurological damage, withdrawal symptoms after birth, and even stillbirth. Understanding the fetal abnormalities linked to addiction during pregnancy highlights the importance of early prenatal care, medical support, and addiction treatment in protecting both mother and baby.
Fetal Abnormalities in Pregnancies Affected by Addiction
When a pregnant woman uses alcohol, tobacco, cannabis, opioids, stimulants, or other substances, these chemicals cross the placenta and interfere with normal fetal development. This can result in structural, neurological, and growth-related abnormalities.
1. Fetal Growth Restriction
Substance exposure can limit oxygen and nutrient delivery to the fetus, leading to low birth weight, small head circumference, and poor muscle and fat development. This is commonly associated with alcohol, nicotine, cocaine, and opioids.
2. Congenital Structural Defects
Alcohol and certain misused prescription drugs can interfere with organ formation, increasing the risk of heart defects, cleft lip or palate, limb abnormalities, and kidney or digestive tract malformations.
3. Brain and Nervous System Damage
Alcohol, methamphetamine, cocaine, and opioids can reduce brain volume, disrupt brain wiring, and impair cognitive development. These changes may result in learning disabilities, memory problems, and lower IQ.
4. Fetal Alcohol Spectrum Disorders (FASD)
Alcohol exposure during pregnancy can cause permanent conditions, including facial abnormalities, intellectual disability, attention problems, and poor impulse control. Alcohol remains the leading preventable cause of birth defects.
5. Neonatal Abstinence Syndrome (NAS)
Babies exposed to drugs in the womb may experience withdrawal after birth. Symptoms include tremors, irritability, feeding difficulties, seizures, and breathing problems. NAS is most commonly linked to opioid, benzodiazepine, and alcohol exposure.
6. Preterm Birth
Cocaine, methamphetamine, tobacco, and alcohol increase the likelihood of birth before 37 weeks, which can result in underdeveloped lungs and organs and a higher risk of infant mortality.
7. Placental Complications
Stimulants and nicotine can cause placental abruption, poor blood flow, and oxygen deprivation to the fetus, creating dangerous pregnancy complications.
8. Increased Risk of Stillbirth
Heavy alcohol use, smoking, opioid overdose, and stimulant use raise the risk of sudden fetal death in late pregnancy.
9. Long-Term Developmental Disorders
Prenatal exposure to alcohol, cannabis, and stimulants has been linked to ADHD-like symptoms, behavioral disorders, speech delays, and motor coordination problems later in childhood.
10. Weakened Immune and Organ Development
Substance exposure can impair liver and kidney development and weaken the infant’s immune system, increasing vulnerability to infections after birth.
Summary
Substance use during pregnancy can disrupt fetal growth, organ formation, brain development, and placental function. These disruptions may lead to congenital defects, developmental disabilities, withdrawal syndromes, preterm birth, or infant death. However, early prenatal care and addiction treatment greatly reduce these risks, improving outcomes for both mother and baby.
Self-Management Strategies to Prevent Fetal Abnormalities in Pregnant Women with Addiction
Pregnancy presents a critical opportunity to protect fetal health, especially when substance use is involved. Drugs and alcohol can cross the placenta and disrupt fetal development, increasing the risk of growth restriction, organ malformations, brain injury, and withdrawal symptoms after birth. However, many of these risks can be reduced when expectant mothers take active steps to manage their health and engage in early treatment. Self-management strategies empower pregnant women to seek prenatal care, begin evidence-based addiction treatment, improve nutrition, reduce stress, and build supportive daily routines. These actions not only improve maternal stability but also create a safer environment for healthy fetal development.
1. Seek Immediate and Consistent Prenatal Care
Attend prenatal appointments as early and as regularly as possible. Doctors can monitor fetal growth, detect early complications, and adjust treatment plans to protect the baby. Prenatal visits also screen for infections such as HIV, hepatitis, and STIs that can affect fetal development.
2. Begin Evidence-Based Addiction Treatment
Engage in medication-assisted treatment (MAT) for opioid use disorder, such as buprenorphine or methadone. These treatments stabilize withdrawal and reduce fetal stress. For alcohol, stimulants, benzodiazepines, and nicotine addiction, healthcare providers can create safer tapering or treatment plans to prevent withdrawal-related harm to the fetus. Avoid quitting substances “cold turkey,” as sudden withdrawal can be dangerous for both mother and baby.
3. Maintain Nutritional Support and Hydration
Substance use can deplete essential nutrients, such as folic acid, iron, and vitamin B12, which are critical for fetal brain and spinal cord development. Taking prenatal vitamins daily, eating balanced meals, and staying well-hydrated support placental blood flow and healthy fetal growth.
4. Practice Stress-Reduction Techniques
Chronic stress increases cortisol levels, which can impair fetal brain and immune development. Helpful strategies include mindfulness or grounding exercises, light physical activity approved by a doctor, deep breathing or guided imagery, and journaling or gratitude tracking.
5. Build a Structured Daily Routine
Set predictable sleep, eating, and rest schedules. Reduce triggers by avoiding environments or people that encourage substance use. Use calendar reminders, checklists, and small goals to stay organized and focused on wellness.
6. Utilize Harm-Reduction Strategies (If Still Using)
If full sobriety has not yet been achieved, reduce harm by using less frequently, avoiding binge use, never mixing substances, and avoiding drugs from unregulated sources due to fentanyl contamination. If injecting, use clean supplies while working toward stopping. Staying hydrated before and after use can also reduce fetal stress.
7. Strengthen Emotional Awareness and Coping Skills
Identify emotional triggers such as fear, shame, loneliness, or trauma. Develop healthy coping skills, such as calling a support person, taking a walk, distracting yourself with calming activities, or using positive affirmations, such as “My choices today protect my baby.” Regular counseling or therapy helps build long-term coping strategies.
8. Monitor and Track Symptoms
Keep a simple log of cravings, mood changes, physical symptoms, and fetal movement. Bringing this information to medical appointments helps care teams adjust treatment early and respond to potential risks.
9. Create a Safety Plan
Identify safe people to contact when cravings or relapse risk increase. Prepare a healthy coping toolkit with snacks, water, a stress ball, a journal, and helpline numbers. Know where local urgent care or emergency obstetric services are located.
10. Stay Connected to Support Groups
Join pregnancy-specific recovery groups such as Medication-Assisted Treatment Moms, AA or NA groups for pregnant women, SMART Recovery, or Celebrate Recovery. Peer support reduces isolation, increases motivation, and encourages healthier choices.
11. Avoid Risky Behaviors That Increase Fetal Harm
Avoid unprotected sex that may lead to infections affecting fetal development. Stay away from unsafe housing situations, violence, or chaotic environments. Follow medical advice on medications, sleep, and activity limits.
12. Engage in Trauma-Informed Therapies (If Needed)
Many pregnant women with addiction have trauma histories that increase relapse risk. Trauma-focused CBT, EMDR, and somatic therapies can support healing. Treating trauma lowers relapse risk and improves maternal–fetal bonding.
Summary
Substance use during pregnancy can place fetal development at serious risk. However, early prenatal care, addiction treatment, healthy routines, stress management, and strong support systems significantly reduce the likelihood of fetal abnormalities. By practicing self-management strategies and staying connected to medical and recovery support, pregnant women can protect their own health while giving their babies the strongest possible start in life.
Family Support Strategies to Prevent Fetal Abnormalities in a Pregnant Woman with Addiction
Family support plays a powerful role in protecting fetal health when a pregnant woman is struggling with addiction. Substance use during pregnancy can interfere with fetal growth, brain development, and organ formation, increasing the risk of birth defects and long-term developmental challenges. However, when families provide compassionate communication, practical assistance, emotional encouragement, and connection to healthcare services, they create a protective environment that reduces stress and promotes healthier choices. The following family support strategies help expectant mothers stay engaged in prenatal care and addiction treatment while improving outcomes for both mother and baby.
1. Promote Compassionate, Non-Judgmental Communication
Speak with empathy and avoid blame, shame, or criticism. Focus on safety and health rather than past mistakes. Use supportive phrases such as, “We’re here to help you stay healthy,” or “You’re not alone—let’s take this one step at a time.” Supportive communication reduces maternal stress, which directly lowers fetal risk.
2. Encourage and Facilitate Prenatal Care
Offer rides to prenatal appointments and help schedule or remember visits. Encourage open communication with healthcare providers. Families who stay involved in prenatal care help catch complications early, which is vital for preventing birth defects.
3. Support Engagement in Addiction Treatment
Help her attend outpatient programs, medication-assisted treatment appointments, therapy, or support groups. Celebrate small recovery wins. Avoid enabling substance use, such as giving money for drugs or ignoring unsafe behaviors. When families support consistent treatment, relapse rates decrease, and fetal development improves.
4. Create a Stable, Low-Stress Home Environment
Reduce household conflict and yelling. Keep routines predictable with regular meals, sleep schedules, and relaxation time. Help set up a calm space for rest and stress management. Lower maternal stress supports healthier fetal brain, heart, and immune development.
5. Help Reduce Triggers and High-Risk Situations
Remove substances from the home. Avoid hosting gatherings where substances are used. Encourage avoiding people who promote substance use. Join her in healthy activities such as walking, cooking, coloring, or gentle stretching. Fewer triggers mean fewer cravings and a safer pregnancy.
6. Help With Practical Needs
Addiction and pregnancy can overwhelm daily functioning. Families can help by preparing nutritious meals, ensuring prenatal vitamins are taken, providing childcare if needed, assisting with transportation, and helping with paperwork for insurance, treatment programs, or WIC. Meeting basic needs reduces the risk of relapse and promotes fetal health.
7. Support Healthy Coping Skills
Encourage deep breathing or grounding exercises together, short walks, journaling, calming music, mindfulness, or pregnancy-safe yoga. Healthy coping lowers stress hormones that interfere with fetal development.
8. Monitor for Warning Signs of Relapse or Distress
Watch for isolation, mood swings, missed appointments, increased cravings, or reconnecting with old using friends. Early intervention prevents binge use or withdrawal episodes that can endanger fetal safety.
9. Encourage Safe Sleep, Nutrition, and Hydration
Prepare balanced meals, offer gentle reminders to eat and drink water, and create a bedtime routine for healthy sleep. Good nutrition and hydration help prevent anemia, birth defects, and placental complications.
10. Provide Emotional Reassurance and Pregnancy Bonding
Talk gently to her and the baby. Encourage bonding activities such as reading to the baby or keeping a pregnancy journal. Reinforce that she is capable of healthy change. Emotional support strengthens motivation to maintain sobriety.
11. Help Keep Her Safe
Remove violent, unsafe, or chaotic individuals from the home. Ensure she has access to emergency care. Encourage safe sex practices to reduce the risk of infections that affect fetal development. Support boundaries with partners who use substances.
12. Support Connection to Community Resources
Help her connect with WIC, OB clinics, substance-use treatment programs, housing support, parenting classes, and peer recovery groups. Connecting to community resources reduces stressors and improves pregnancy outcomes.
Summary
Families are a critical protective factor in pregnancies affected by addiction. Through compassionate communication, stable home environments, practical assistance, and encouragement of prenatal and addiction treatment, families can significantly reduce the risk of fetal abnormalities. With strong family involvement and medical support, pregnant women are better equipped to protect their health and give their babies the best possible start in life.
Community Resource Strategies to Prevent Fetal Abnormalities in Pregnant Women with Addiction
1. Expand Access to Low-Barrier Prenatal Care
Communities can provide walk-in prenatal clinics, mobile OB units, and telehealth visits to make care more accessible. Offering prenatal services within addiction treatment centers reduces the need for multiple appointments. Prioritizing same-day visits for pregnant women with substance use ensures early monitoring. Early and consistent prenatal care helps detect fetal abnormalities, growth restrictions, infections, and organ development concerns as soon as possible.
2. Increase Availability of Medication-Assisted Treatment (MAT) Programs
Ensuring opioid treatment programs accept pregnant patients without waitlists is essential. Community health centers and OB offices can provide buprenorphine and methadone, while integrated MAT and prenatal care services under one roof simplify treatment. MAT stabilizes withdrawal, reduces fetal distress, and prevents low birth weight and congenital abnormalities.
3. Provide Trauma-Informed Behavioral Health Services
Free or low-cost counseling, mental health therapy, and pregnancy-specific support groups help address underlying trauma and emotional stress. Trauma-informed care prevents retraumatization and lowers relapse risk. Community clinics should offer therapists trained in perinatal mental health and addiction to meet the specialized needs of pregnant women.
4. Create Pregnancy-Specific Support Groups
Support groups such as Recovering Moms programs, Moms in MAT groups, Celebrate Recovery for Expecting Mothers, and SMART Recovery Pregnancy Circles reduce isolation and build motivation. These groups also provide education on fetal health risks and recovery strategies.
5. Strengthen Harm-Reduction Programs
Community harm-reduction services can provide clean supplies, prenatal vitamins, condoms, and referrals to care. Distributing fentanyl test strips and naloxone kits prevents overdose emergencies. Harm-reduction case managers help women navigate appointments, insurance, and transportation. These programs reduce infections such as HIV, hepatitis C, and STIs that are linked to fetal abnormalities and pregnancy complications.
6. Expand Access to Safe Housing Programs
Pregnancy-priority housing, substance-free shelters, transitional housing with recovery coaches, and residential programs that allow infants to remain with their mothers provide stability. Safe housing decreases stress, improves nutrition, and supports consistent treatment—key factors in healthy fetal development.
7. Provide Case Management and Care Coordination
Pregnancy case managers can connect mothers to prenatal care, addiction treatment, childcare, housing, and nutrition resources. Community health workers and peer mentors help accompany women to appointments and assist with paperwork. This wraparound support reduces stressors that often lead to missed care or relapse.
8. Increase Access to Nutrition and WIC Services
WIC programs provide food vouchers, prenatal vitamins, nutrition counseling, and breastfeeding education. Community food pantries offering pregnancy-friendly items improve fetal nutrition and reduce the risk of birth defects.
9. Improve Transportation Assistance
Medicaid ride programs, bus vouchers, ride-share partnerships, and mobile clinic routes help women attend prenatal and addiction treatment appointments. Transportation support removes one of the most common barriers to early prenatal care.
10. Offer Community-Based Parenting and Pregnancy Education
Free childbirth classes, parenting courses for mothers in recovery, doula support trained in addiction care, and home-visiting nurse programs strengthen maternal confidence and knowledge of maternal health. Education increases treatment participation and reduces risky behaviors that harm the fetus.
11. Provide Legal and Advocacy Support
Legal aid services help mothers navigate housing, custody, insurance, and safety concerns. Safe-reporting policies encourage women to seek prenatal and addiction care without fear of punishment. Reducing fear leads to more prenatal visits and fewer fetal complications.
12. Connect to Behavioral Health Hotlines and Crisis Lines
Community hotlines, perinatal mental health lines, addiction crisis services, and warm lines offer immediate emotional support. These services provide help during cravings, distress, or relapse risk—critical moments that impact fetal safety.
13. Strengthen Cross-System Collaboration
Partnerships between OB/GYN clinics, addiction treatment centers, hospitals, public health departments, and social service agencies ensure coordinated care. Collaboration allows mothers to receive continuous, comprehensive support throughout pregnancy.
Summary
Community resources are a powerful protective force in pregnancies affected by addiction. When prenatal care, addiction treatment, mental health services, housing support, nutrition programs, and transportation assistance are accessible and coordinated, pregnant women are far more likely to engage in care early and consistently. These community-based strategies reduce maternal stress, prevent relapse, and significantly lower the risk of fetal abnormalities—giving both mother and baby the opportunity for a healthier future.
Frequently Asked Questions
Here are some common questions:
1. How does substance use affect a developing fetus?
Substances consumed by a pregnant woman pass through the placenta to the fetus. These chemicals can interfere with organ formation, brain development, oxygen supply, and nutrient delivery, increasing the risk of birth defects and developmental disorders.
2. Which substances are most harmful during pregnancy?
Alcohol, opioids, cocaine, methamphetamine, nicotine, and certain misused prescription medications are strongly linked to fetal abnormalities. Alcohol is the leading preventable cause of birth defects.
3. Can alcohol cause permanent fetal damage?
Yes. Alcohol exposure can cause Fetal Alcohol Spectrum Disorders (FASD), leading to permanent physical, cognitive, and behavioral impairments.
4. What is Neonatal Abstinence Syndrome (NAS)?
NAS occurs when a baby is exposed to drugs in the womb and experiences withdrawal after birth. Symptoms include tremors, feeding difficulties, irritability, seizures, and breathing problems.
5. Can smoking during pregnancy harm the fetus?
Yes. Nicotine reduces oxygen to the fetus and increases the risk of low birth weight, preterm birth, stillbirth, and placental complications.
6. Does cannabis use during pregnancy cause fetal abnormalities?
Research links prenatal cannabis exposure to low birth weight and long-term effects on attention, memory, and behavior, although studies are ongoing.
7. Is it safe to quit substances suddenly during pregnancy?
Not always. Sudden withdrawal from alcohol, opioids, or benzodiazepines can be dangerous for both mother and fetus. Medical supervision is recommended.
8. Can medication-assisted treatment (MAT) help pregnant women with addiction?
Yes. MAT using medications such as methadone or buprenorphine stabilizes the mother, prevents withdrawal, and improves fetal outcomes compared to continued illicit drug use.
9. Does early prenatal care reduce fetal risks?
Yes. Early prenatal care allows healthcare providers to monitor fetal development, manage addiction safely, provide nutritional support, and detect complications early.
10. Are fetal abnormalities always permanent?
Some effects, such as withdrawal symptoms or low birth weight, may improve with treatment and care. However, structural defects and brain development injuries are often permanent.
11. Can a healthy baby still be born if the mother had substance use problems?
Yes. When pregnant women enter treatment early, receive prenatal care, and stop or medically manage substance use, outcomes improve significantly.
12. What support services help prevent fetal harm?
Prenatal clinics, addiction treatment programs, mental health counseling, peer support groups, housing assistance, and nutrition programs all help protect fetal health.
13. What should a pregnant woman do if she is using substances?
Seek medical care immediately. Healthcare providers can offer safe treatment options without judgment and help protect both mother and baby.
14. Can stress and trauma increase the risk of substance use during pregnancy?
Yes. Many women use substances to cope with trauma, anxiety, or depression. Treating mental health conditions reduces relapse risk and improves pregnancy outcomes.
15. Is fetal harm from addiction preventable?
In many cases, yes. Early treatment, consistent prenatal care, family support, and community resources greatly reduce the risk of fetal abnormalities.
Conclusion
Preventing fetal abnormalities in pregnancies affected by addiction depends on empowering mothers with consistent self-care, emotional support, and safe recovery pathways. When pregnant women build healthy routines, seek prenatal and addiction treatment, and learn stress-reduction skills, they can greatly reduce the risks to their developing baby. Family members play a critical role by offering practical help, encouraging treatment, and creating a calm, substance-free environment. At the same time, community resources—such as prenatal clinics, medication-assisted treatment programs, housing services, peer support groups, and harm-reduction programs—provide essential layers of stability and guidance. Together, these strategies create a protective network that helps mothers stay safer, healthier, and more supported throughout pregnancy, giving their infants the best possible chance at strong fetal development and a healthy future.
Video: This Happens to Babies When Parents Struggle With Addiction #pregnancy #fetal #awareness