People with addiction remain in denial, often unaware of the severity of their condition due to both psychological defenses and brain changes that affect judgment and self-awareness. This denial can lead to blaming others and resisting help. Breaking through it requires self-management, supportive family involvement, and access to community resources like support groups and outreach programs. Together, these strategies can guide individuals toward recognition and recovery.
Why Denial in Addiction Isn’t Just Denial: The Hidden Forces That Keep People Stuck
Denial in addiction is complex, and it often stems from a combination of biological, psychological, and social factors. Understanding why someone might genuinely believe they “don’t have a problem” is key to offering compassionate, practical support. Here’s a closer look at what drives denial beneath the surface:
🧠 1. Brain Changes from Addiction
Addiction physically alters the brain’s reward system and executive function—areas responsible for decision-making, judgment, and self-awareness. Over time, the brain becomes wired to prioritize the substance above all else, even at the cost of seeing the damage it’s causing. Insight and self-reflection are impaired so that denial can feel like the truth to the person experiencing it.
💭 2. Cognitive Dissonance
Cognitive dissonance is the mental discomfort people feel when their actions clash with their self-image. For instance, someone may think, “I’m a responsible person. But responsible people don’t drink every day.” Instead of confronting this contradiction, the brain may protect itself by saying, “I don’t really have a problem.” This isn’t always conscious lying—it’s self-preservation.
🛡️ 3. Defense Mechanisms
Denial is one of several defense mechanisms the mind uses to avoid uncomfortable truths. Common examples include:
- Rationalization: “I only use it because work is stressful.”
- Minimization: “At least I’m not as bad as them.”
- Projection: “Everyone else has a problem, not me.”
These defenses offer short-term emotional relief but long-term harm.
👥 4. Stigma and Shame
Admitting to addiction can feel like admitting failure—especially in a society that still views substance use through a moral lens. Many people fear judgment, rejection, or punishment. Some internalize the stigma, which deepens their shame and makes it harder to be honest with themselves or others.
😖 5. Trauma and Emotional Avoidance
For many, substances are a way to numb deep emotional pain—trauma, grief, anxiety, or depression. Letting go of the substance means facing those raw emotions, which can feel overwhelming or even unbearable. Denial serves as a protective layer that keeps the coping mechanism intact.
🧩 Why Denial Isn’t Just Stubbornness
Denial in addiction is not simply about refusing to see the truth. It’s a layered response built on:
- Neurological changes that distort self-perception
- Psychological defenses that reduce guilt and shame
- Social stigma that discourages honesty
- Emotional pain that makes change feel dangerous
Why People with Addiction Blame Others: It’s More Than Just Avoiding Responsibility
It’s a sharp and often frustrating experience: someone deep in addiction insists their substance use is everyone else’s fault. But much like denial, blame is usually a psychological survival strategy, not just deflection or manipulation. Understanding why people with addiction blame others can open the door to more compassionate and effective responses.
🧠 1. Defense Mechanisms: Projection and Externalization
Blaming others is a common defense mechanism. Two key types show up in addiction:
- Projection: placing one’s own negative feelings or behaviors onto someone else.
- Externalization: attributing personal actions to outside forces rather than taking responsibility.
Saying “If you hadn’t treated me this way, I wouldn’t drink” is often easier than saying “I’m drinking in a way that’s hurting people.” This mental strategy helps avoid shame, guilt, and internal pain—at least temporarily.
🧠💥 2. Cognitive Dissonance
People with addiction often experience cognitive dissonance—the discomfort of acting in ways that conflict with their self-image. To reduce this, the brain may shift the blame:
- “My job is too stressful.”
- “My partner pushes me to the edge.”
- “Anyone else in my situation would use it too.”
These beliefs help protect their self-esteem and avoid confronting painful truths.
😖 3. Trauma and Learned Behavior
Many people struggling with addiction come from environments marked by trauma, instability, or dysfunctional communication. In such settings, blaming others may have been modeled or even necessary for emotional survival.
They may genuinely feel that others are responsible for their pain. And if substance use is their way of coping, then it makes emotional sense—if not rational sense—to blame those who caused the pain.
🔄 4. Avoiding Change
Blame can also serve as a delay tactic. If someone admits they are responsible for their substance use, it implies that they may need to change, which is scary and overwhelming.
By saying “You’re the problem,” they shift focus away from themselves and avoid facing the idea of giving up a coping mechanism they still rely on.
💬 5. Manipulation vs. Survival
Blaming behavior might look manipulative, and sometimes it is—but often it’s more about emotional survival than conscious control. Many people are addicted:
- Feel deeply vulnerable
- Rely on substances to get through the day
- Genuinely believe what they’re saying in the moment
They aren’t always trying to deceive others—sometimes they’re trying to convince themselves.
🧩 What Blame Really Means in Addiction
Blame in addiction is not just about avoiding responsibility—it’s a mix of survival strategies and altered thinking. Often, people blame others because:
- They’re protecting themselves from shame and pain
- Their brain are using defense mechanisms to reduce emotional overload
- They’re trying to justify continued use
- They’ve been shaped by environments where blame was normalized
Understanding the psychology behind blame doesn’t excuse harmful behavior, but it helps us approach the issue with empathy—and helps guide people toward healing when they’re ready.
How to Help Someone with Addiction See They Need Help—Without Pushing Them Away
There’s no simple script—but there are powerful, compassionate strategies that can open the door to honesty, self-reflection, and eventually, recovery.
🧠 1. Create a Safe, Judgment-Free Space
People in denial expect to be attacked or shamed. So when you approach them calmly, it’s disarming in a good way.
- Speak respectfully and with care.
- Avoid labels like “addict” or “junkie.”
- Try: “I’ve noticed you’ve been struggling, and I care about you.”
Why it works: It reduces shame and makes it emotionally safer for them to be honest.
💬 2. Use “I” Statements, Not “You” Accusations
Saying “You’re ruining your life” will trigger defensiveness. Instead, say:
- “I feel scared when I see what’s happening.”
- “I miss the old you.”
Why it works: It focuses on your experience rather than their failures.
📊 3. Mirror Reality—Gently
Don’t try to force them to see they have a problem. Reflect the real-life consequences without judgment:
- “You’ve missed work a few times—are you okay?”
- “You’ve seemed more distant lately. I wonder if the drinking is part of that.”
This invites reflection, not argument.
🧠💡 4. Use Motivational Interviewing Tools
This technique helps people explore both sides of their ambivalence.
Ask open-ended questions like:
- “What do you like about using?”
- “What don’t you like about how things have been?”
When they express any desire for change, echo it:
- “It sounds like part of you is ready for things to be different.”
⏳ 5. Be Patient, but Stay Consistent
Denial often fades in stages:
- Precontemplation – No problem
- Contemplation – Maybe there’s a problem
- Preparation – Thinking about change
- Action – Seeking help
Even moving from Step 1 to Step 2 is progress. Stay present and persistent.
🧠🔗 6. Focus on Life Functioning, Not the Substance
Sometimes it helps to avoid talking directly about the substance:
- “Do you feel like life’s where you want it to be right now?”
- “What’s been hardest for you lately?”
This invites them to connect the dots themselves.
🤝 7. Offer Help—Not Ultimatums (Unless Safety Is at Risk)
Ultimatums often backfire unless it’s about serious safety concerns. Instead, offer a partnership:
- “Would you be open to talking to someone—just once?”
- “I’ll go with you if that helps.”
Support without pressure builds trust.
🚨 8. In Crisis Situations, Consider a Structured Intervention
For serious addiction, a carefully planned intervention might be needed—with a professional present. Key elements:
- Planned in advance
- Focused on love, not blame
- Includes a clear treatment path
🧩 Helping Them See the Truth, Gently
Helping someone out of denial isn’t about forcing the truth—it’s about guiding them toward it:
✅ Stay calm, compassionate, and specific
✅ Use curiosity, not confrontation
✅ Reinforce any minor signs of insight
✅ Offer support without control
When they’re ready to take the first step, they’ll remember who stood by them.
How People with Addiction Can Begin Honest Self-Reflection—Without Shame
Many people assume addiction blocks self-awareness—but with the proper support, people struggling with addiction can engage in deep, meaningful reflection. The key is creating emotional safety. Addiction often numbs feelings, warps self-image, and instills fear of facing reality. So the process needs to be gentle, guided, and non-shaming.
Here’s how self-reflection can unfold:
🧠 1. Reflection Happens Gradually
Self-awareness doesn’t come in one big moment—it often starts small:
- “I’m not happy with how life feels.”
- “Maybe this isn’t working anymore.”
That’s enough. Those flickers of insight matter.
🪞 2. Ask Reflective Questions (Even the Hard Ones)
These prompts can help someone look inward without shame:
- “What was I trying to escape when I used?”
- “What have I lost because of this?”
- “Have I ever tried to stop? Why or why not?”
- “Do I feel like myself anymore?”
Writing them down often feels safer than thinking them alone.
📓 3. Try Journaling or Audio Diaries
Reflection deepens when we slow our thoughts:
- Track cravings and triggers
- Record regrets and successes
- Describe emotions honestly
Prefer to talk? Audio notes work too. Both let people externalize their inner world.
👥 4. Use Therapy or Group Support as a Mirror
It’s hard to reflect clearly in isolation. Supportive spaces like:
- Therapy (especially addiction-informed)
- Groups like AA, NA, or SMART Recovery
…offer compassionate feedback.
Example: A sponsor might say,
“You say you’re fine, but your week sounds really tough. Are you sure you’re okay?”
That kind of gentle insight builds awareness.
🌀 5. Use a Cost/Benefit Reflection Tool
Try a “decisional balance sheet”:
| Pros of Using | Cons of Using |
|---|---|
| Helps me sleep | Hurts relationships |
| Temporary relief | I feel worse after |
| Pros of Stopping | Cons of Stopping |
|---|---|
| Better health | Withdrawal |
| More clarity | Fear of boredom |
Seeing it all laid out can shift thinking from “I need this” to “This might be hurting me.”
🪞 6. Name the Consequences Honestly
Ask:
- “What have I sacrificed?”
- “Who have I hurt?”
- “Do I have as much control as I thought?”
Not to self-punish, but to see the whole picture.
❤️ 7. Balance Honesty with Self-Compassion
The truth is hard—but it must be paired with kindness:
“Yes, I’ve made mistakes. But I’m trying to understand myself. That matters.”
Addiction thrives on shame. Recovery begins with self-honesty + self-kindness.
🧩 How People with Addiction Can Reflect
✅ Ask reflective questions gently
✅ Use journaling or audio notes
✅ Talk with therapists or groups for outside insight
✅ Explore pros and cons of using vs. stopping
✅ See consequences clearly—but without shame
✅ Practice self-compassion throughout
How Families Can Support a Loved One in Denial—With Compassion and Boundaries
Supporting a loved one with addiction—especially when they’re in denial—is emotionally exhausting, confusing, and painful. But there are ways to help that are both compassionate and effective.
Here are eight family strategies that can make a real difference:
❤️🩹 1. Be Supportive—But Don’t Enable
It’s a fine line. Real support means expressing care and concern—not covering for the person or shielding them from the consequences of their behavior.
Helpful Support Sounds Like:
“I’m here for you, and I want to help you when you’re ready.”
Enabling Looks Like:
- Lying to employers or friends
- Giving money that funds substance use
- Making excuses for harmful actions
Tip: Let natural consequences unfold, but never withdraw your love.
🧠 2. Educate Yourself About Addiction and Denial
Denial isn’t just being “in denial.” It’s a neuropsychological symptom of addiction—often reinforced by brain changes and emotional defense mechanisms.
Learn About:
- The stages of change (from denial to action)
- How substances affect motivation, judgment, and insight
- Common defenses like rationalizing, minimizing, or blaming
Why it helps: Understanding reduces resentment and enables you to respond strategically rather than emotionally.
🧘 3. Stay Calm and Consistent
Addiction often breeds chaos. Your calmness can be an anchor.
Try Saying:
“I’m scared when I see how much you’re drinking.”
“I miss the version of you before this took over.”
Avoid: Angry confrontations, shouting matches, or threats. Stay grounded—even if they aren’t.
📣 4. Use Gentle, Specific Confrontation
Avoid broad labels like “You’re an addict.” Instead, focus on observable behaviors:
“You missed Jamie’s birthday because you were passed out—do you think that’s okay?”
“You said you were done, but I found another bottle—what happened?”
Stick to facts. That’s harder to deny.
🧩 5. Encourage Reflection, Not Just Action
You may want them in rehab right now. But reflection often comes before readiness. Ask open-ended questions:
- “Is this helping or hurting you?”
- “Are you okay with how things are going?”
Reflection creates room for insight. Orders shut it down.
🧠 6. Use the CRAFT Method (Community Reinforcement and Family Training)
CRAFT is a proven, science-based model that teaches families how to:
- Reinforce sober behavior
- Communicate positively
- Reduce enabling
- Gently encourage treatment—without ultimatums
Why it works: It supports change while preserving the relationship and your own mental health.
Need help using CRAFT? I can walk you through examples.
🚫 7. Avoid Common Pitfalls
❌ Nagging or Yelling – It fuels defensiveness
❌ Shaming or Blaming – Shame is a relapse trigger
❌ Ultimatums Too Soon – Only use when boundaries are crossed, and only if you can enforce them
🧘♀️ 8. Protect Your Own Mental Health
You matter too. Supporting someone in denial is draining. To stay strong, prioritize your well-being.
- Join a support group (like Al-Anon or SMART Family & Friends)
- See a therapist who understands addiction dynamics
- Set and maintain boundaries that protect your peace
You can love someone and still say “no” to harm.
✅ Family Strategies That Help
| Strategy | Why It Works |
|---|---|
| Stay supportive, not enabling | Builds trust while avoiding codependency |
| Use calm, consistent messages | Keeps communication open and reduces resistance |
| Focus on behavior, not identity | Avoids triggering shame or shutdown |
| Ask open-ended, reflective questions | Encourages insight rather than rebellion |
| Learn CRAFT methods | Backed by evidence to promote treatment engagement |
| Take care of yourself | Prevents burnout and sets a healthy example |
You don’t have to fix everything all at once. Even small shifts—like learning new communication tools or saying “I love you, and I’m here when you’re ready”—can start to move the needle.
How Communities Can Gently Challenge Denial and Support Addiction Recovery
Denial is one of addiction’s most powerful defenses—and breaking through it often requires more than one voice. When families, professionals, and friends aren’t getting through, community resources can offer broader, sustained encouragement and accountability.
Here’s how community-based support can help someone slowly begin to see their situation more clearly:
🧭 1. Peer-Led Support Groups (Even if They’re Not Ready to Quit)
Sometimes, denial begins to crack just by sitting in a room with others who’ve lived through addiction.
Examples include:
- 12-Step Groups (AA, NA, Cocaine Anonymous)
- SMART Recovery (science-based and non-religious)
- LifeRing, Refuge Recovery, or other mindfulness/secular programs
Even if someone insists they “don’t have a problem,” hearing others share similar stories can spark insight:
“That sounds like me… and they’re calling it addiction. Maybe I need to take a second look.”
📍 2. Community Health Clinics and Harm Reduction Centers
For people who aren’t ready to stop using these services, they offer nonjudgmental, walk-in support—focused on safety and dignity.
They might offer:
- Medical care and STD testing
- Needle exchanges
- Naloxone (Narcan) or fentanyl test strips
- On-site counselors available for low-pressure conversations
Why it works: Feeling safe and respected can soften defenses and create room for reflection.
📚 3. Public Awareness Campaigns & Real Stories in the Media
People often dismiss what loved ones say—but they may pay attention to a documentary, podcast, or lived-experience panel.
Ideas:
- Share a podcast episode or recovery story on social media
- Recommend a documentary or YouTube video featuring lived experiences
- Attend local town halls or “Voices of Recovery” panels
When someone hears,
“I didn’t think I had a problem either, until…”
they may start rethinking their own situation.
🧑⚕️ 4. Motivational Interviewing Outreach Programs
Some community outreach programs include trained professionals who go directly to where people are—without judgment.
These outreach workers:
- Visit shelters, encampments, or homes
- Offer harm reduction and low-barrier health services
- Build trust slowly, without pressuring change
Why it works: It meets people where they are and lets insight grow at their pace.
🏛️ 5. Drug Courts and Diversion Programs (for Legal-Involved Individuals)
For individuals who enter the justice system due to their substance use, structured diversion programs can be powerful motivators.
These programs may include:
- Mandated counseling and group therapy
- Regular drug testing
- Educational programs focused on self-reflection
Even if someone isn’t ready for change, the structure can plant seeds that grow into genuine insight.
🧘♂️ 6. Faith-Based or Spiritual Recovery Communities
For people with strong spiritual or religious ties, faith-based recovery groups can offer a values-based path to change.
Examples:
- Celebrate Recovery
- The Salvation Army’s recovery programs
- Church-based addiction support groups
These communities can provide emotional support, purpose, and accountability grounded in faith and compassion.
🤝 7. Family & Community Education Workshops
Some towns or organizations host free workshops for families and concerned community members. These can:
- Teach how addiction and denial work
- Share effective support techniques (like the CRAFT method)
- Build solidarity and reduce shame
Seeing other families go through the same thing can be eye-opening—not just for relatives, but for the person struggling too.
“I’m not the only one facing this. Maybe I do need help.”
🧩 Community Strategies That Help with Denial
| Resource Type | How It Helps |
|---|---|
| Peer support groups | Models insight and breaks isolation |
| Harm reduction centers | Offers safety and dignity, not pressure |
| Awareness campaigns | Uses real stories to bypass defensiveness |
| Outreach programs | Builds trust with low-pressure contact |
| Legal diversion programs | Creates structured opportunities for reflection |
| Faith-based support | Provides a moral and spiritual path to change |
| Family education | Empowers loved ones and reduces stigma |
No one breaks through denial alone. Community resources offer mirrors, models, and momentum that family and friends can’t always provide on their own. When insight feels too threatening or painful, the right setting—and the right voice—can make all the difference.
If you’re supporting someone in denial, consider connecting them (or yourself) with one of these community options. You don’t have to wait until they’re “ready” to start planting seeds of change.
Frequently Asked Questions
Here are some common questions:
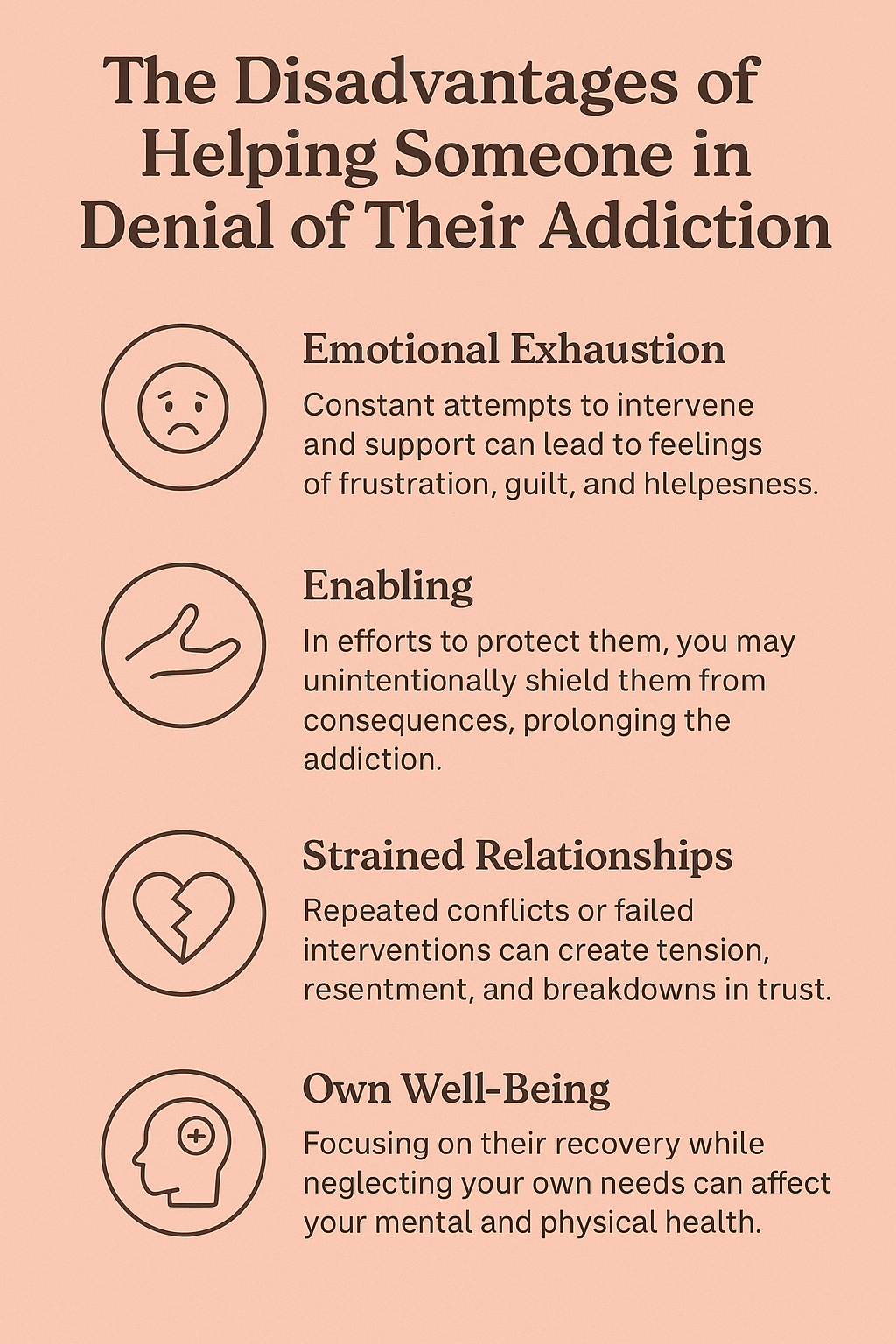
Question: What are the disadvantages of helping someone in denial of their addiction?
Answer: Helping someone in denial of their addiction is courageous, but it comes with real emotional, relational, and practical challenges. Here are some of the main disadvantages to be aware of:
1. Emotional Exhaustion
You may end up investing more energy than they are willing to, leading to burnout, frustration, or resentment. It can feel like talking to a wall, especially when they minimize or reject your concerns.
You want change more than they do—and that’s draining.
2. Enabling Risk
In trying to “help,” you might accidentally shield them from consequences, especially if you:
- Cover for their behavior
- Give money or housing
- Make excuses to others
This can prolong the addiction by removing the natural motivators for change.
3. Damage to the Relationship
Pushing too hard can strain or even break the relationship. They may:
- Get defensive or angry
- Cut off contact
- Accuse you of judging or controlling them
You risk becoming the “enemy” in their eyes, even when your intentions are loving.
4. Neglecting Your Own Needs
Supporting someone in denial can consume your life—emotionally, financially, and mentally. You may put your own well-being, relationships, or health on the back burner while trying to “save” them.
You can’t heal someone by breaking yourself.
5. False Hope and Repeated Disappointment
You might hold onto hope that they’ll change soon, only to be let down repeatedly when they relapse or deny there’s an issue. This cycle can erode your trust, hope, and sense of stability.
6. Delay in Professional Help
By constantly stepping in, you might delay them from seeking formal treatment. Sometimes loved ones become the central “support system,” and the person doesn’t feel urgency to get outside help.
7. Safety Risks
If their addiction leads to aggressive or erratic behavior, helping them might put you or others at physical or emotional risk—especially in high-conflict situations.
Helping someone in denial is incredibly hard. The key is to support without sacrificing yourself—use boundaries, protect your peace, and avoid doing the emotional work for them.
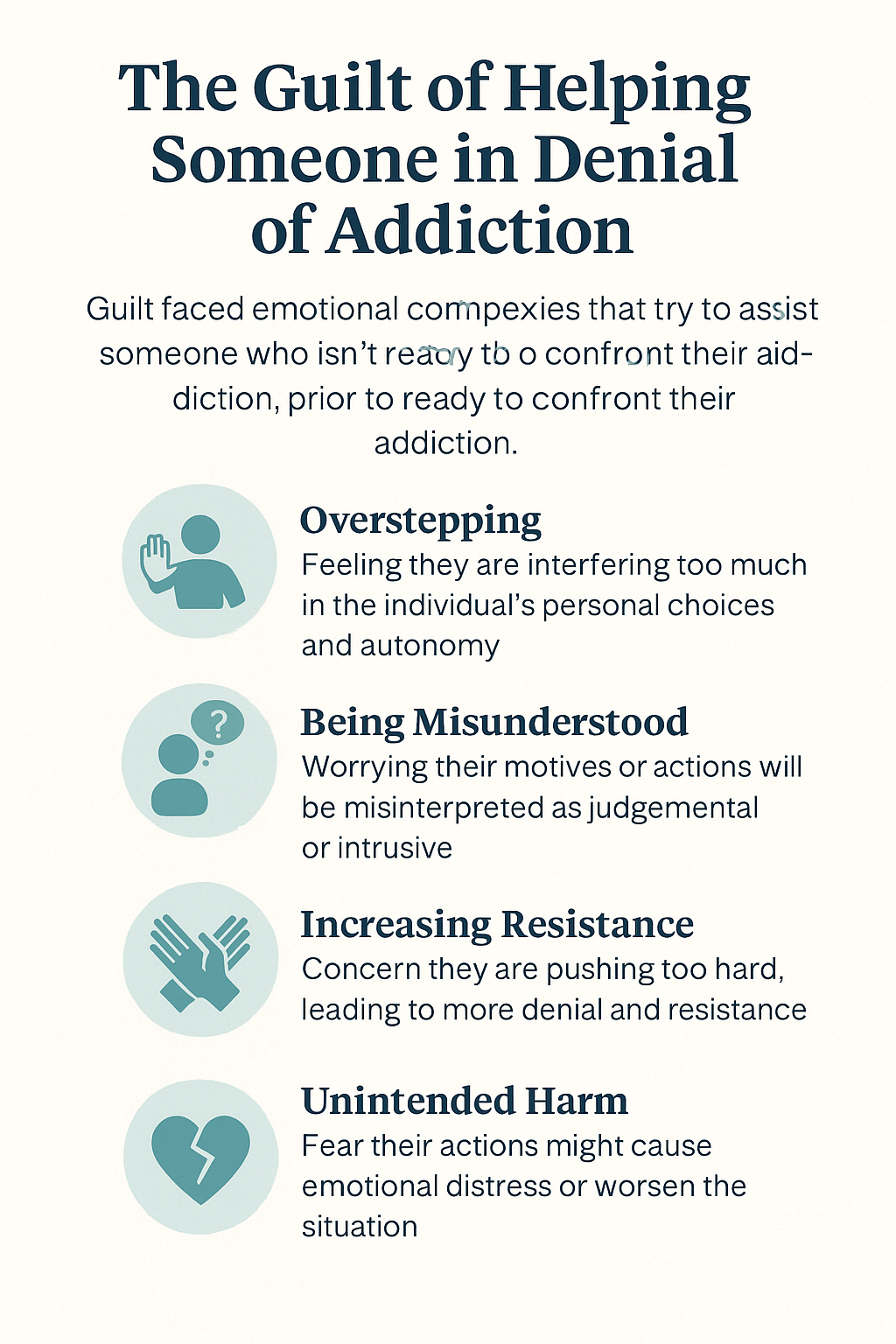
Question: What is the guilt involved in helping someone in denial of addiction?
Answer: The guilt involved in helping someone in denial of addiction can be profound, confusing, and persistent. It stems from a painful clash between wanting to help and feeling helpless, and from second-guessing your role—especially when things don’t improve.
Here are the common types of guilt people feel in this situation:
1. Guilt for Setting Boundaries
You might feel guilty for:
- Saying “no” to money or shelter
- Refusing to lie or cover up for them
- Pulling back to protect your own health
Even when it’s the healthy choice, it can feel like abandonment or betrayal.
2. Guilt for Not Doing Enough
There’s often a nagging feeling of:
“If I just tried harder, said it better, or did more—they’d change.”
You may feel responsible for their recovery, especially if you’re the one closest to them, trying to help. But addiction is not something you can fix for someone else.
3. Guilt for Enabling in the Past
People often feel ashamed if they:
- Gave money or rides that supported use
- Looked the other way
- Believed their excuses too many times
“I should have seen it sooner.”
“I helped them keep going—without realizing it.”
This guilt can be heavy, even if you were acting out of love or fear.
4. Guilt Over Anger and Resentment
It’s common to feel angry at the person—especially when they deny, lie, or hurt others—but then feel guilty for being angry.
You may think:
- “They’re sick… I shouldn’t be mad.”
- “What kind of person gets mad at someone in pain?”
But anger and guilt often go hand in hand when you’re emotionally stretched thin.
5. Survivor’s Guilt (If Others Didn’t Make It)
If you’ve seen others lose their battle with addiction—or if you’re in recovery yourself—you might feel a deeper kind of guilt about being “okay” while they’re still stuck.
6. Guilt Over Tough Love or Ultimatums
If you’ve ever said, “I can’t be around you while you’re using” or “You can’t live here if this continues,” guilt can rush in fast—especially if the person spirals afterward.
Even necessary boundaries can feel like cruelty when someone is struggling.
Guilt shows up when love meets powerlessness.
But guilt doesn’t mean you’re doing the wrong thing—it means you care deeply in a situation where the outcomes aren’t in your control.
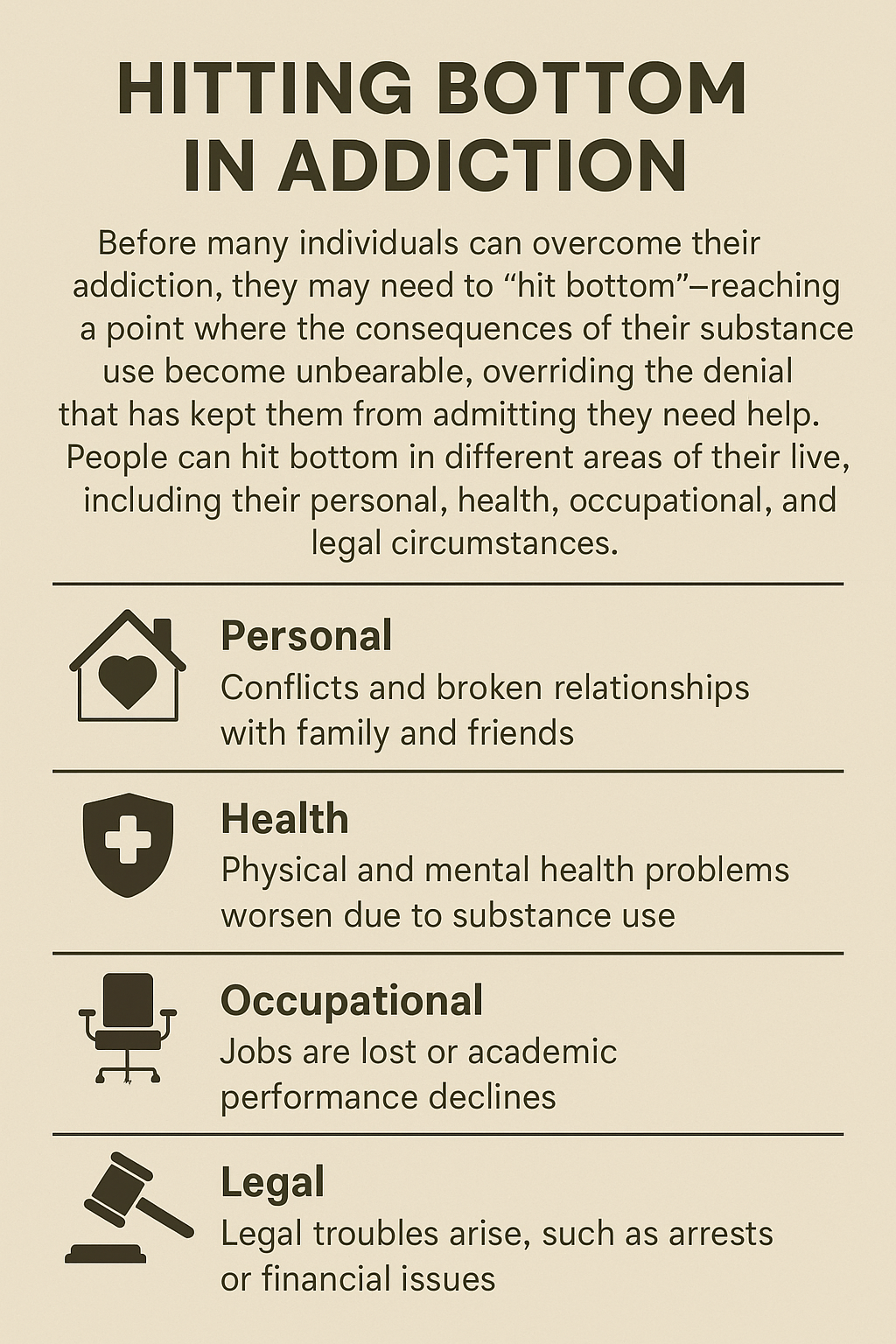
Question: What situations are called “hitting bottom: before admitting to the addiction and asking for help?
Answer: “Hitting bottom” refers to the point where someone with an addiction experiences enough pain, loss, or consequences that denial breaks—and they begin to see the need for change. It’s often misunderstood as one dramatic crash, but it can look very different for each person.
Here are some everyday situations that are often called “hitting bottom”:
💔 1. Relationship Loss
- A partner leaves.
- Kids are taken away, or contact is cut off.
- Close friends or family stop talking to them.
This kind of loss often breaks the illusion that “everything is under control.”
💼 2. Job or Career Collapse
- Being fired for performance or absenteeism.
- Losing a professional license.
- Ruined reputation in their field.
For many, identity is tied to work—so losing it can shake denial hard.
🧍♂️ 3. Social Isolation
- Realizing no one calls anymore.
- Feeling completely alone even in a crowd.
- Not being invited to family gatherings or events.
Loneliness can become a mirror: “How did I end up here?”
⚖️ 4. Legal Trouble
- DUI, arrest, jail time.
- Custody battles related to substance use.
- Court-mandated treatment or probation.
The structure of the legal system can force a level of clarity—especially if they’re told, “Get help or go to jail.”
💸 5. Financial Collapse
- Losing housing or becoming homeless.
- Bankruptcy or deep debt.
- Selling important things or stealing to use.
When survival becomes difficult, the reality of addiction often hits hard.
🧠 6. Mental Health Crisis
- Panic attacks, severe depression, and suicidal ideation.
- Feeling like they’re “losing their mind.”
- Realizing their coping method is making things worse.
These internal signals can be just as powerful as external losses.
🏥 7. Health Scare
- Overdose or hospitalization.
- Diagnosed with liver failure, infection, or other serious illness.
- Seeing the physical toll in the mirror: weight loss, sores, and aging rapidly.
Physical consequences are hard to deny once they become visible or life-threatening.
☠️ 8. Loss of Someone Else to Addiction
- A friend dies of an overdose.
- A sibling is hospitalized.
- Seeing someone else’s bottom becomes a wake-up call: “That could be me.”
❗Important Note:
“Bottom” is relative.
What feels like rock bottom for one person may not register for another. Some people hit multiple “bottoms” and still resist change.
Conclusion
Denial in addiction is a complex barrier shaped by both psychological defenses and neurological changes that distort self-perception. This often leads individuals to shift blame and avoid responsibility, making recovery more difficult. However, with consistent self-management practices, supportive family involvement, and accessible community resources, individuals can begin to confront their denial and move toward healing. A coordinated, compassionate approach increases the chances of breaking through denial and supporting long-term recovery.
Videos: The TOP 3 Mistakes You Make When Helping an Addict
What REALLY Happens When You Hit Rock Bottom with Addiction