Suicide risk in individuals with substance use disorders (SUDs) is influenced by mental health issues, trauma, isolation, and lack of support, along with demographic factors. Prevention requires a multifaceted approach, including self-management, family and community support, policy changes, and societal shifts. Reducing stigma, enhancing emotional regulation, and fostering support can improve recovery and prevent suicide.
The Interwoven Struggle: Understanding the Link Between Addiction and Suicide
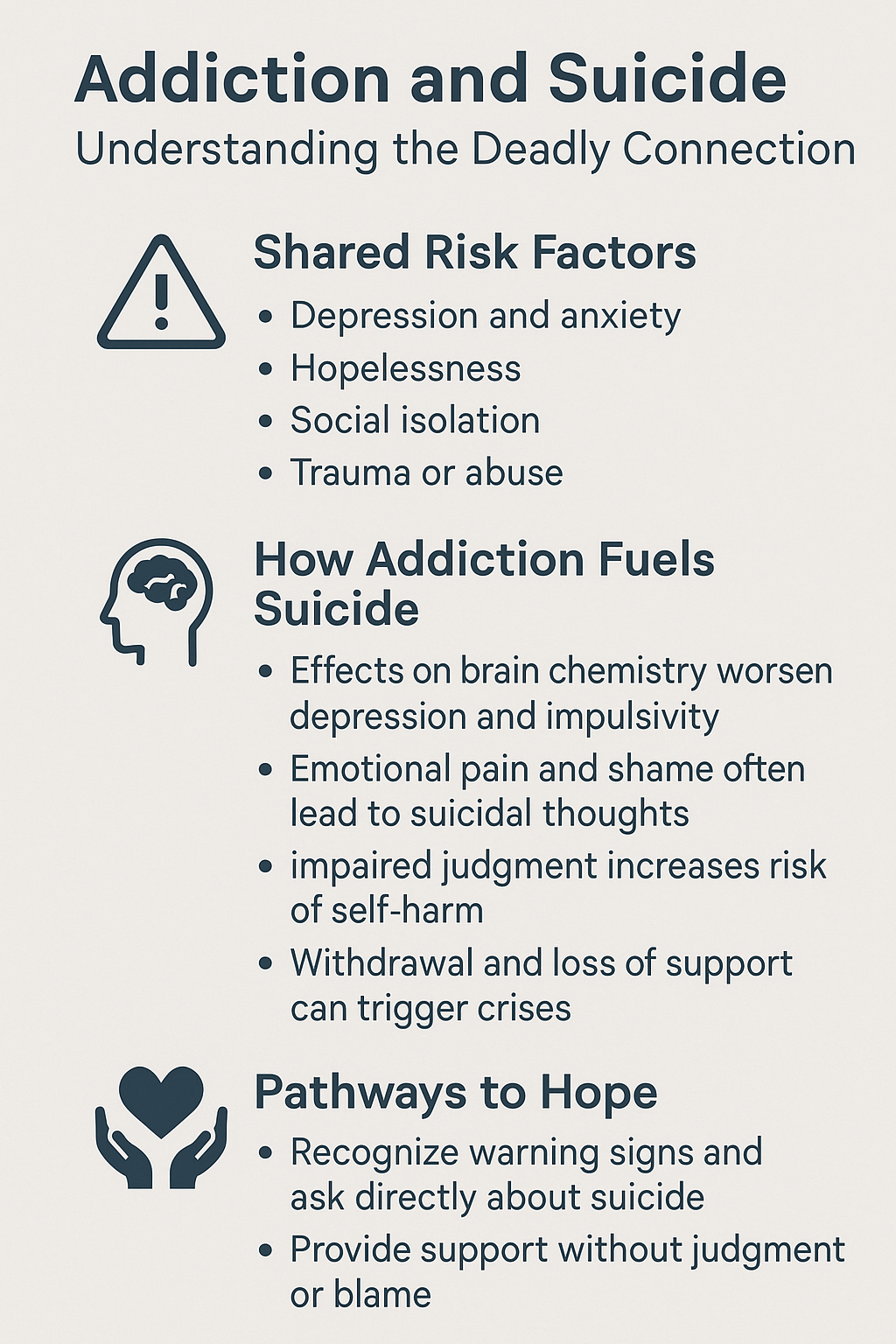
Addiction and Suicide: Understanding the Deadly Connection
Addiction and suicidal risk are deeply interconnected, with one often exacerbating the other. Individuals struggling with substance use disorders (SUD) frequently face intense emotional, psychological, and physical challenges that increase their vulnerability to suicidal thoughts and behaviors. Understanding the key factors that contribute to this connection is crucial for prevention, intervention, and support.
1. The Psychological Toll of Addiction
- Mental Health Issues: Many individuals with addiction also suffer from co-occurring mental health conditions such as depression, anxiety, or post-traumatic stress disorder (PTSD). These mental health disorders amplify feelings of despair and hopelessness—two significant risk factors for suicide.
- Guilt and Shame: Addiction can create overwhelming feelings of guilt and shame. Many individuals feel trapped in a cycle of substance use and regret, believing they have lost control of their lives. This deep-seated self-loathing can push them toward suicidal ideation.
2. The Physical and Neurological Impact
- Brain Chemistry Alterations: Substance abuse alters the brain’s reward and mood-regulation systems. Chronic drug or alcohol use can lead to emotional instability, poor impulse control, and increased vulnerability to depression, which in turn elevates the risk of suicide.
- Withdrawal Effects: The withdrawal process—especially from substances like opioids, alcohol, and benzodiazepines—can lead to extreme anxiety, depression, and even suicidal thoughts. The intensity of these withdrawal symptoms sometimes causes individuals to act on self-destructive impulses.
3. Risky Behaviors and Increased Vulnerability
- Self-Destructive Patterns: Substance use impairs judgment, increasing the likelihood of dangerous behaviors such as reckless driving, self-harm, and unsafe decision-making. These behaviors heighten the risk of fatal consequences, whether intentional or accidental.
- Overdose Risks: Many overdoses occur in the context of despair. While some may be accidental, others are deliberate acts of self-harm. The blurred line between an overdose and suicide makes it critical to address underlying mental health concerns in individuals with SUD.
4. The Social and Environmental Struggles
- Isolation and Loneliness: Addiction often leads to strained relationships, social withdrawal, and a deep sense of loneliness. Without a strong support system, individuals may feel disconnected and without purpose, increasing their risk of suicide.
- Financial and Life Stressors: Addiction can lead to job loss, economic instability, legal troubles, and family breakdowns. The accumulation of these stressors can make individuals feel hopeless, reinforcing thoughts of suicide as a way out.
5. The Challenge of Co-Occurring Disorders
- Dual Diagnosis: Many people with addiction also have an underlying mental illness, a condition known as dual diagnosis. The presence of untreated or poorly managed mental health conditions can worsen substance use and increase the risk of suicide.
- Lack of Comprehensive Treatment: If addiction and mental health disorders are treated separately, individuals may feel their struggles are never fully addressed. Effective, integrated treatment is essential to break this cycle.
Addressing the Risk: Prevention and Intervention
To reduce suicide risk among individuals with addiction, a proactive and compassionate approach is necessary.
- Screening for Suicide Risk: Healthcare providers must assess both addiction and suicidal ideation during evaluations. Tools like the Columbia-Suicide Severity Rating Scale (C-SSRS) can help identify those at high risk.
- Integrated Treatment Approaches: Treating addiction and co-occurring mental health conditions together leads to better outcomes. Comprehensive programs that combine medical care, therapy, and peer support can significantly reduce both substance use and suicidal ideation.
- Cognitive Behavioral Therapy (CBT): CBT and other therapeutic approaches can help individuals challenge negative thought patterns and develop healthier coping mechanisms. Therapy plays a vital role in managing emotional distress and reducing suicidal risk.
Protective Factors: Building Resilience and Hope
- Strong Support Networks: Meaningful connections with family, friends, or support groups can provide encouragement and hope. Peer support communities, such as Narcotics Anonymous (NA), offer a sense of belonging that can reduce isolation.
- Access to Treatment and Crisis Support: Detox programs, counseling, and crisis hotlines provide vital resources for individuals struggling with addiction and suicidal thoughts. Ensuring accessible, non-judgmental support can save lives.
- A Message of Hope: Recovery is possible, and fostering resilience is crucial. Many individuals have successfully overcome addiction and mental health struggles, finding purpose and fulfillment beyond substance use.
In summary, addiction and suicide are intertwined struggles, but with the right interventions, support systems, and comprehensive treatment, lives can be saved. By addressing both substance use and mental health challenges simultaneously, we can create pathways to recovery and renewed hope for those who need it most.
Addiction and Suicide: Examining the Demographics and Risk Factors
Substance Use Disorders (SUDs) are strongly associated with an increased risk of suicidal ideation and attempts. Research consistently shows that individuals with SUDs are at a significantly higher risk of experiencing suicidal thoughts and engaging in self-harm compared to the general population. This link is influenced by a combination of psychological, biological, and social factors that vary across different demographic groups.
1. Understanding the Demographics of Addiction and Suicide
While addiction and suicide can affect anyone, specific populations are at a heightened risk due to underlying vulnerabilities.
Age Groups Most Affected
- Young Adults (18-34): This group experiences high rates of substance misuse, particularly alcohol and stimulants. Impulsivity and mental health struggles, such as depression and anxiety, contribute to elevated suicide risks.
- Middle-Aged Adults (35-54): This demographic has the highest rates of suicide, often due to life stressors, chronic health conditions, financial struggles, and substance use.
- Older Adults (55+): While less likely to misuse substances at high levels, older adults who do struggle with addiction face increased suicide risks, especially those dealing with chronic pain, social isolation, and depression.
Gender Differences
- Men: More likely to die by suicide, particularly those who abuse alcohol or opioids. Men often underutilize mental health services, contributing to higher suicide rates.
- Women: More likely to experience suicidal ideation and attempts, especially when struggling with co-occurring depression and substance use disorders.
Racial and Ethnic Disparities
- Native American and Alaska Native populations have the highest rates of both substance use disorders and suicide, often linked to historical trauma, socioeconomic disparities, and lack of mental health resources.
- White, non-Hispanic individuals have high rates of opioid-related deaths and suicide, particularly in rural areas affected by the opioid crisis.
- Black and Hispanic communities experience lower suicide rates but face significant barriers to accessing addiction and mental health treatment, which can lead to unaddressed distress.
2. Psychological and Neurobiological Factors
Mental Health Disorders and Addiction
Many individuals with SUDs have co-occurring mental health disorders, such as:
- Depression and Anxiety: These conditions contribute to feelings of hopelessness and self-harm tendencies.
- PTSD: Trauma survivors, including veterans and abuse victims, often turn to substances as a coping mechanism, increasing suicide risk.
- Bipolar Disorder and Schizophrenia: These severe mental health conditions are strongly linked to both substance use and suicidal behavior.
Brain Chemistry and Impulsivity
- Substance use alters neurotransmitter systems, particularly serotonin and dopamine, which regulate mood and impulse control. This disruption can increase depression and impulsive decision-making, leading to suicidal actions.
3. Social and Environmental Stressors
Economic and Relationship Struggles
- Unemployment and financial distress are major suicide risk factors, particularly for middle-aged men with alcohol or opioid use disorders.
- Family and relationship conflicts often contribute to both addiction and suicidal ideation, particularly when combined with domestic violence or custody disputes.
Social Isolation and Stigma
- Addiction can lead to the loss of social connections, further deepening feelings of loneliness.
- Stigma surrounding substance use and mental health can prevent individuals from seeking help, increasing their risk of suicide.
4. Overdose as a Form of Suicide
Intentional vs. Accidental Overdose
- Some overdoses occur as deliberate suicide attempts, especially among those struggling with opioid addiction.
- Others may be unintentional but driven by self-destructive tendencies, where individuals engage in reckless substance use without regard for consequences.
5. The Role of Withdrawal in Suicide Risk
The withdrawal process from substances like alcohol, opioids, and benzodiazepines can lead to severe depression, anxiety, and suicidal thoughts. The distress associated with withdrawal increases the likelihood of suicidal behavior if appropriate medical and psychological support is not available.
6. Strategies for Risk Assessment and Intervention
Screening and Early Detection
Healthcare providers should routinely screen individuals with SUDs for suicide risk using tools like:
- Columbia-Suicide Severity Rating Scale (C-SSRS)
- Patient Health Questionnaire (PHQ-9) for depression and suicidal ideation
Integrated Treatment for Addiction and Mental Health
- Dual diagnosis treatment programs address both substance use and underlying mental health disorders.
- Cognitive Behavioral Therapy (CBT) and Dialectical Behavior Therapy (DBT) help individuals develop coping mechanisms to manage distress without turning to substances.
Crisis Intervention and Support
- Immediate access to crisis hotlines, emergency mental health services, and inpatient care is essential for those experiencing acute suicidal ideation.
- Medication-assisted treatment (MAT) for opioid and alcohol addiction can reduce relapse risk and stabilize mood.
7. Protective Factors and Hope for Recovery
Strong Social Support Networks
- Family, friends, and peer support groups like Alcoholics Anonymous (AA) or Narcotics Anonymous (NA) provide encouragement and accountability.
Hope-Based Treatment Approaches
- Recovery-focused programs that emphasize resilience, personal growth, and life purpose can help individuals regain a sense of hope and self-worth.
Increased Access to Care
- Expanding access to affordable, stigma-free addiction and mental health services can reduce suicide rates among individuals with SUDs.
Addiction and suicide are deeply interconnected, with demographic factors playing a crucial role in shaping risk levels. Understanding the psychological, biological, and social elements of this crisis can help guide more effective prevention and intervention strategies. By providing integrated treatment, strong social support, and crisis intervention resources, we can reduce the devastating impact of addiction-related suicides and promote pathways to healing and recovery.
Empowering Recovery: Self-Management Strategies for Addiction and Suicide Prevention
Self-management strategies play a crucial role in preventing suicide among individuals with substance use disorders (SUDs). These strategies empower individuals to take control of their recovery, manage their mental health, and reduce the risk of suicidal ideation. By implementing self-care techniques, fostering resilience, and enhancing emotional regulation, individuals can cultivate a sense of agency and stability. Below are several self-management strategies designed to support recovery and mitigate suicide risk.
1. Developing a Strong Support System
Building a Network of Support
- A reliable support network is essential for individuals in recovery. This includes family, friends, peer support groups, and professional counselors. A strong community reduces feelings of isolation, a significant risk factor for suicide.
Peer Support
- Engaging in support groups such as Alcoholics Anonymous (AA), Narcotics Anonymous (NA), or online recovery communities provides a safe environment to share experiences and receive guidance from those with similar struggles.
Family Support
- Educating family members about addiction and mental health fosters a compassionate home environment. Encouraging open communication and providing resources for family members can enhance their ability to offer meaningful support.
2. Engaging in Regular Mental Health Check-Ins
Daily Emotional Check-Ins
- Individuals in recovery should regularly assess their emotional state by acknowledging feelings of distress, sadness, or anxiety early on. Awareness of these emotions helps in taking proactive steps to prevent crises.
Journaling
- Writing about emotions, experiences, and thoughts provides insight into one’s mental state. A journal can serve as a tool for self-reflection and emotional regulation.
Self-Reflection
- Setting aside time for reflection on recovery progress, personal goals, and emotional well-being reinforces commitment to long-term health.
3. Coping Strategies for Stress and Emotional Pain
Developing Healthy Coping Skills
- Effective coping mechanisms help manage substance cravings and suicidal thoughts. Techniques such as deep breathing, progressive muscle relaxation, and guided imagery can be helpful.
Mindfulness and Meditation
- Practicing mindfulness helps individuals stay grounded and manage stress. Techniques such as meditation and breathing exercises promote emotional stability.
Cognitive Behavioral Techniques (CBT)
- CBT techniques assist in recognizing and challenging negative thought patterns that contribute to both substance use and suicidal ideation.
Grounding Exercises
- For those experiencing overwhelming emotions, focusing on the five senses or engaging in physical activities like stretching or walking can help shift attention away from distressing thoughts.
4. Developing a Relapse Prevention Plan
Creating a Personalized Plan
- A relapse prevention plan outlines strategies for managing cravings and avoiding high-risk situations. This plan should include specific actions such as calling a support person, engaging in a calming activity, or attending a meeting.
Identifying Triggers
- Recognizing personal triggers—such as stress, social settings, or certain emotions—enables individuals to prepare strategies for managing them effectively.
Emergency Contacts and Hotlines
- Having immediate access to support contacts, including crisis hotlines and trusted individuals, ensures help is available in moments of distress.
5. Setting Realistic Goals and Tracking Progress
Establishing Personal Goals
- Setting achievable short-term and long-term goals provides direction and purpose. Using the SMART (Specific, Measurable, Attainable, Relevant, Time-bound) criteria can enhance the effectiveness of goal-setting.
Daily or Weekly Goals
- Goals may include attending recovery meetings, engaging in self-care, or practicing mindfulness. Celebrating small achievements fosters motivation and a sense of accomplishment.
Tracking Recovery Progress
- Monitoring milestones such as sober days or emotional growth reinforces positive behavior and serves as a motivational tool during difficult times.
6. Practicing Self-Care and Healthy Lifestyle Choices
Physical Health Maintenance
- Good physical health significantly improves mental well-being. Regular exercise releases endorphins, which reduce stress, anxiety, and depression.
Exercise
- Activities such as walking, yoga, or strength training can enhance mood, reduce cravings, and boost self-esteem.
Sleep Hygiene
- Maintaining a consistent sleep routine is essential for mental health, as poor sleep increases the risk of substance relapse and suicidal thoughts.
Nutrition
- A well-balanced diet supports brain function and mood stabilization, reducing the likelihood of emotional fluctuations that could trigger relapse or suicidal ideation.
7. Developing Emotional Regulation Skills
Identifying and Expressing Emotions
- Learning to recognize and communicate emotions in healthy ways prevents suppression, which can lead to substance use or suicidal thoughts.
Emotional Validation
- Encouraging self-compassion and recognizing emotions as valid without judgment reduces distress and impulsive behavior.
Distress Tolerance
- Techniques such as radical acceptance and positive distraction (e.g., engaging in hobbies or relaxation activities) help manage emotional pain without resorting to harmful behaviors.
8. Developing a Suicide Prevention Safety Plan
Creating a Safety Plan
A structured suicide prevention plan outlines steps to take when suicidal thoughts arise. It should include:
- Recognizing Warning Signs: Identifying personal indicators of distress (e.g., increased hopelessness, withdrawal, self-harm thoughts).
- Emergency Contacts: Listing trusted individuals and mental health professionals who can offer immediate support.
- Coping Strategies: Engaging in healthy activities that have been effective in managing distress.
- Distraction Techniques: Having a list of enjoyable activities to shift focus away from distressing thoughts.
- Seeking Professional Help: Contacting crisis hotlines or mental health services when necessary.
9. Mindfulness of Substance Use Triggers
Avoiding High-Risk Situations
- Avoiding environments or situations that encourage substance use helps reduce relapse risk.
Mindful Awareness
- Practicing mindfulness in moments of temptation allows individuals to pause and make conscious choices rather than acting impulsively.
Creating New Habits
- Replacing old behaviors with healthier routines fosters long-term recovery and personal growth.
In summary, self-management strategies are essential for individuals with substance use disorders who are at risk of suicide. By fostering self-awareness, emotional regulation, and strong support networks, individuals can take control of their recovery and mental health. These strategies not only help manage addiction and prevent relapse but also offer a sense of hope, purpose, and empowerment. Through consistent self-care and proactive planning, individuals can navigate challenges with resilience and move toward a fulfilling life free from substance dependence and suicidal ideation.
Family Support Strategies for Addiction and Suicide Prevention
Family support plays a critical role in preventing suicide among individuals struggling with substance use disorders (SUDs). Families can provide emotional support, encourage treatment, help address underlying mental health issues, and create a safe environment for recovery. The following family support strategies can be effective in reducing the risk of suicide among individuals with substance use problems:
1. Fostering Open Communication
- Encourage Honest Dialogue: Families can foster an environment that supports open communication, allowing individuals to express their feelings without fear of judgment. Regular check-ins and conversations can help identify any signs of suicidal ideation or distress early.
- Listen Actively: Active listening is vital. Family members should focus on understanding the person’s emotions and thoughts without immediately offering solutions or judgment. This validates their feelings and helps the individual feel supported.
- Non-Judgmental Attitude: Avoid blaming or shaming the person for their substance use or mental health struggles. Criticism can increase feelings of shame and isolation, which may escalate suicidal thoughts.
2. Promote Professional Treatment
- Encourage Therapy and Counseling: Encourage the individual to seek professional help, whether it be through counseling, cognitive-behavioral therapy (CBT), dialectical behavior therapy (DBT), or family therapy. Therapy can help address the underlying issues of addiction and mental health disorders, reducing the risk of suicidal ideation.
- Dual Diagnosis Treatment: Many people with substance use disorders also suffer from mental health disorders. Family members should encourage treatment that addresses both the substance use and co-occurring mental health conditions simultaneously. Integrated treatment is more effective in reducing the risk of suicide.
- Assistance with Accessing Resources: Help the individual find local treatment centers, addiction support groups (such as Narcotics Anonymous or Alcoholics Anonymous), and mental health services. Navigating the healthcare system can be overwhelming, and family support can reduce barriers to care.
3. Provide Emotional and Social Support
- Emotional Validation: Acknowledge the individual’s emotional pain. Validating their feelings rather than dismissing them can prevent further isolation and help the person feel understood.
- Encourage Positive Relationships: Support the individual in building a strong network of positive relationships with family members, friends, and peers in recovery groups. Social support is essential for recovery and reducing feelings of isolation.
- Avoid Enabling Behaviors: While showing compassion is essential, families should avoid enabling behaviors that reinforce the addiction. This may include covering up the person’s substance use, making excuses for them, or allowing the addiction to go unaddressed. Enabling can prolong the addiction and increase suicidal risk.
4. Monitor and Ensure Safety
- Create a Safe Environment: Remove or secure any items that could be used for self-harm, such as firearms, sharp objects, or medications. Ensuring that the individual is in a safe environment is crucial, especially during periods of heightened emotional distress.
- Monitor Warning Signs: Family members should educate themselves about the warning signs of suicide and substance misuse. These may include withdrawal from social activities, mood swings, increased substance use, feelings of hopelessness, or expressing thoughts of death. Early intervention can prevent further escalation.
- Have Emergency Plans: Family members should have a plan in place in case the individual expresses suicidal ideation or attempts self-harm. This could involve contacting a therapist, calling a suicide hotline, or seeking immediate medical attention.
5. Encourage Healthy Lifestyle Changes
- Support a Healthy Routine: Encouraging a structured routine that includes regular meals, exercise, and sleep is essential for both physical and emotional health. A healthy lifestyle can help regulate mood and reduce stress, which in turn can help reduce both addiction and suicidal thoughts.
- Promote Healthy Coping Mechanisms: Families can help the individual develop healthier ways to cope with stress and negative emotions. This could involve learning mindfulness techniques, practicing relaxation exercises, or engaging in activities that promote well-being, such as creative hobbies or outdoor activities.
- Support Medication Management: For those receiving treatment that involves medication (such as antidepressants or medications for addiction), families can help ensure proper adherence to prescribed regimens and help manage any side effects.
6. Create a Non-Stressful, Supportive Home Environment
- Reduce Conflict: Chronic family conflict or stress can exacerbate addiction and increase suicidal risk. Families should work toward reducing conflict within the home and creating a stable, predictable environment that supports recovery.
- Establish Boundaries and Expectations: While providing emotional support, family members must set clear boundaries and expectations for the individual’s behavior. These boundaries can help create structure and prevent relapse or suicidal ideation by establishing clear rules for what is acceptable in the home.
- Offer Hope and Encouragement: Encouraging the individual to see that recovery is possible, no matter how difficult the journey may seem, is key in reducing feelings of hopelessness. Family members should remind the individual of their strengths and offer encouragement through setbacks.
7. Education and Awareness
- Educate the Family: Family members should educate themselves about substance use disorders, mental health issues, and the potential link to suicide. Understanding the nature of addiction and the struggles involved can help them provide more effective support.
- Understand the Cycle of Addiction and Suicide Risk: Learning about the cyclical nature of addiction and the way it can feed into suicidal ideation helps families understand the patterns and challenges the individual is facing. This awareness can guide appropriate interventions.
- Be Aware of Mental Health Symptoms: Families should be familiar with the symptoms of depression, anxiety, and other mental health issues that often accompany substance use disorders. Recognizing these symptoms early can help reduce the risk of suicide.
8. Encourage Engagement in Support Groups
- Family Support Groups: Support groups for families of individuals with substance use disorders (e.g., Al-Anon or Nar-Anon) can provide much-needed guidance, emotional support, and resources. Family members can connect with others who are going through similar struggles and gain insights into managing the challenges of addiction and preventing suicide.
- Support the Individual in Joining Peer Groups: Encouraging the individual to join peer support groups such as Narcotics Anonymous (NA) or Alcoholics Anonymous (AA) can provide a community of individuals who understand the struggles of addiction. Peer support helps reduce feelings of isolation and offers emotional and practical support.
9. Address Family Dynamics and Past Trauma
- Family Therapy: Family therapy can help address dysfunctional family dynamics and improve communication. It can help family members understand their roles in the individual’s addiction and recovery process and heal from past trauma or conflicts that may contribute to the addiction or suicidal risk.
- Addressing Past Trauma: If the individual’s addiction is rooted in past trauma or abuse, family members can support therapy focused on trauma recovery, which may reduce both the substance use and the suicidal ideation linked to unresolved trauma.
10. Know When to Seek Professional Help
- Seek Professional Guidance: Families should know when to seek professional help for themselves and the individual with substance use issues. If the situation becomes too overwhelming or if there are signs of immediate suicidal risk, it is essential to reach out to a therapist, counselor, or hotline for guidance.
- Involvement in a Crisis Plan: In case of crisis, having access to professional resources such as suicide prevention hotlines, mental health crisis services, or addiction counselors is essential. Families should be aware of these resources and have them readily available.
Community Resource Strategies for Addiction and Suicide Prevention
Community resources play a vital role in preventing suicide among individuals with substance use disorders (SUDs). These resources offer support, treatment options, and opportunities for engagement that can reduce isolation, improve access to care, and address the root causes of both addiction and suicidal ideation. Below are several community-based strategies and resources that can help prevent suicide among individuals struggling with substance abuse.
1. Accessible Mental Health and Substance Use Treatment Services
- Integrated Treatment Centers: Community-based treatment centers that offer integrated care for both substance use and mental health disorders (dual diagnosis treatment) are essential. These centers provide comprehensive services that address both addiction and the underlying mental health issues contributing to suicidal thoughts.
- Outpatient Counseling and Therapy: Local mental health clinics and outpatient programs provide counseling and therapy for individuals dealing with both substance use and mental health issues. These services are typically more affordable and accessible than inpatient care.
- Crisis Stabilization Services: Community-based crisis centers can provide immediate care and stabilization for individuals experiencing a mental health crisis. These services often include a safe space for individuals to recover from acute substance intoxication, manage withdrawal symptoms, or address urgent suicidal thoughts.
2. 24/7 Suicide and Crisis Helplines
- National Suicide Prevention Lifeline: Providing access to national suicide prevention helplines (such as the 988 Suicide & Crisis Lifeline in the U.S.) can offer immediate support for individuals in crisis. These hotlines connect people with trained counselors who can provide emotional support, coping strategies, and guidance for seeking help.
- Substance Use Disorder Hotlines: Many communities have local or national helplines explicitly dedicated to substance abuse recovery, such as the Substance Abuse and Mental Health Services Administration (SAMHSA) helpline. These hotlines can help connect individuals with resources for treatment and recovery support, as well as offer crisis intervention for those at risk of suicide.
3. Peer Support and Recovery Groups
- 12-Step Programs (AA, NA, etc.): Communities can offer support through 12-step programs such as Alcoholics Anonymous (AA) and Narcotics Anonymous (NA), which provide ongoing support and social networks for individuals in recovery. These programs promote sobriety, emotional well-being, and social connection, all of which can help prevent suicidal thoughts.
- Peer Support Specialists: Peer support programs, where individuals with lived experience of substance use and mental health struggles provide guidance and support, are becoming more widespread in many communities. Peer support specialists can offer a unique form of empathy and practical advice that can resonate with individuals at risk of suicide.
- Support Groups for Families: Community organizations can offer support groups for the family members of individuals struggling with substance abuse (e.g., Al-Anon or Nar-Anon). These groups provide education, emotional support, and guidance on supporting loved ones through recovery while maintaining healthy boundaries.
4. Crisis Intervention Teams (CIT)
- Crisis Intervention Teams: Many communities have specialized crisis intervention teams composed of trained law enforcement officers and mental health professionals who are equipped to respond to situations involving individuals with substance use disorders and suicidal ideation. These teams can help de-escalate crises, provide immediate mental health interventions, and ensure that individuals receive the appropriate care.
- Mobile Crisis Teams: In some areas, mobile crisis teams can be dispatched to an individual’s home or community setting when a mental health crisis is reported. This service can prevent unnecessary hospitalizations and help connect the individual with more appropriate mental health and addiction treatment resources.
5. Community-Based Outreach and Education Programs
- Public Awareness Campaigns: Community organizations can launch public education campaigns to raise awareness about the risks of substance use, the signs of suicide, and available resources for both. These campaigns can reduce stigma, increase knowledge about mental health and addiction, and encourage individuals to seek help before reaching a crisis point.
- Community Education on Suicide Prevention: Providing training for community members, including educators, healthcare workers, first responders, and family members, can improve their ability to identify signs of suicide and intervene effectively. Training programs like QPR (Question, Persuade, Refer) or mental health first aid can help individuals recognize warning signs and take action to support someone at risk.
6. Safe Housing and Supportive Environments
- Sober Living Homes: Sober living homes are community-based housing options that provide a structured, substance-free environment for individuals in recovery. These homes offer a supportive environment for people transitioning from inpatient treatment or those struggling with maintaining sobriety, reducing isolation, and preventing relapse, which can contribute to suicidal thoughts.
- Affordable Housing Resources: Addressing homelessness or unstable housing situations is essential for individuals struggling with addiction and mental health issues. Lack of stable housing is a significant risk factor for both substance use and suicidal ideation. Communities can help provide access to affordable housing, creating a safer, more stable environment for recovery.
7. Youth and School-Based Programs
- School Mental Health Programs: Schools can implement programs that educate students about the risks of substance use and suicide, as well as teach coping skills and stress management techniques. Programs that provide emotional support, mental health screenings, and access to counselors can be instrumental in identifying at-risk youth and intervening early.
- Youth Mentorship Programs: Community-based youth mentorship programs can help provide emotional guidance and support for young people at risk of substance use and mental health problems. Positive adult role models can help youth navigate life challenges and reduce the likelihood of engaging in risky behaviors that can lead to substance use and suicidal ideation.
8. Collaboration with Local Employers and Workplaces
- Workplace Wellness Programs: Employers can play a role in preventing suicide among individuals with substance use issues by implementing employee wellness programs. These programs can provide support for mental health, substance use issues, and stress management, and they can encourage employees to seek help before reaching a crisis point.
- Employee Assistance Programs (EAPs): Many workplaces offer EAPs that provide confidential counseling and support services for employees facing personal issues, including addiction and mental health concerns. These programs can help employees access resources before problems escalate to suicide risk.
9. Access to Medical Care and Harm Reduction Strategies
- Medication-Assisted Treatment (MAT): MAT is a critical resource for individuals with opioid use disorders and other substance use issues. Community clinics and local health departments can provide MAT, which has been shown to reduce substance use, improve mental health, and decrease the risk of overdose and suicide.
- Harm Reduction Programs: Harm reduction strategies, such as needle exchange programs, supervised injection sites (where legal), and overdose prevention education, help individuals with substance use disorders reduce the physical risks associated with substance use. These programs can create a safer environment for people to receive support and may prevent fatal overdose or self-harm.
In summary, community resources play an essential role in preventing suicide among individuals with substance use disorders by providing accessible care, emotional support, crisis intervention, and opportunities for social connection. By ensuring that individuals have access to mental health services, addiction treatment, peer support, and harm reduction resources, communities can significantly reduce the risk of suicide. Coordination between healthcare providers, local agencies, schools, and employers can create a comprehensive, supportive system that addresses the complex needs of individuals facing both addiction and suicidal ideation.
Government Interventions for Addiction and Suicide Prevention
Government resources and strategies are crucial for preventing suicide among individuals with substance use disorders (SUDs). These strategies involve both federal and local agencies working together to create a broad system of care, prevention, and support for those at risk. Below are key government-led strategies and resources that can help reduce suicide risk in individuals struggling with substance abuse.
1. Federal Programs and Initiatives
Substance Abuse and Mental Health Services Administration (SAMHSA)
SAMHSA is the primary federal agency overseeing mental health and substance use treatment in the U.S. SAMHSA funds numerous programs aimed at both preventing substance use and supporting recovery. Key programs include:
- National Suicide Prevention Lifeline (988): A 24/7 national hotline that connects individuals in crisis to trained counselors, offering specialized support for individuals with substance use disorders.
- Grants for Suicide Prevention: SAMHSA administers funding through its Suicide Prevention Resource Center to local and state governments, tribes, and organizations for suicide prevention programs.
- Co-Occurring Disorder Programs: Initiatives focused on treating individuals with both mental health and substance use disorders through integrated treatment programs.
Centers for Disease Control and Prevention (CDC)
- The CDC plays a pivotal role in suicide prevention through research and public health initiatives. By funding state and local health departments, the CDC implements evidence-based prevention strategies, such as public education campaigns and community engagement programs.
National Institute on Drug Abuse (NIDA)
- NIDA funds research on the links between substance use and suicide and promotes programs that integrate mental health and addiction treatment. It also supports public education campaigns raising awareness about the mental health risks associated with drug and alcohol use.
2. State and Local Government Strategies
Statewide Suicide Prevention Plans
- Many states have developed Suicide Prevention Plans, which involve collaborations between health departments, mental health organizations, and addiction treatment centers. These plans use federal funding to expand treatment services, promote mental health education, and improve suicide prevention efforts in high-risk populations.
Medicaid and Medicaid Expansion
- Medicaid provides critical support for people with SUDs, covering medication-assisted treatment (MAT) and mental health counseling. Many states have expanded Medicaid under the Affordable Care Act, improving access to these services.
Medicaid/Medicare Integration for Co-occurring Disorders
- States are integrating Medicaid/Medicare services to improve care for individuals with both mental health and substance use disorders, leading to better treatment outcomes and reduced suicide risk.
3. Crisis Intervention and Response
Crisis Intervention Teams (CIT)
- Local governments train law enforcement officers to respond effectively to mental health crises, ensuring that individuals at risk of suicide or overdose receive proper care.
Mobile Crisis Units
- In some areas, mobile crisis units staffed with mental health professionals provide in-the-field assessments and intervention, reducing unnecessary incarceration or hospitalization.
4. Harm Reduction Policies
Harm Reduction Programs
Governments have implemented harm reduction strategies to reduce suicide risk among people with SUDs. Examples include:
- Needle Exchange Programs: Reducing the risk of overdose and disease transmission.
- Supervised Injection Sites: Offering medical supervision to prevent overdoses and encourage treatment engagement.
- Naloxone Distribution: Providing free naloxone kits to first responders and at-risk individuals to prevent overdose deaths.
5. Public Education Campaigns
- Governments fund campaigns to reduce the stigma surrounding addiction and mental health, encouraging individuals to seek help. Examples include SAMHSA’s “Talk. They Hear You.” campaign, which educates parents on preventing youth substance use.
6. Access to Treatment and Rehabilitation Services
State-Funded Addiction Treatment
- Many states offer free addiction treatment services for uninsured individuals, including detox, outpatient therapy, inpatient rehab, and long-term recovery support.
Medication-Assisted Treatment (MAT) Coverage
- Federal and state governments support MAT programs for opioid and other substance use disorders, combining medications with counseling and therapy to stabilize mental health and reduce cravings.
7. Research and Data Collection
National Suicide Prevention Research
- Federal agencies like SAMHSA, NIH, and NIDA fund research on the connections between substance use and suicide, helping to develop better prevention, treatment, and intervention strategies.
8. Workplace and Employer Resources
Employee Assistance Programs (EAPs)
- Governments encourage or mandate Employee Assistance Programs (EAPs) in workplaces, providing confidential counseling and support services for employees struggling with substance use and mental health issues.
9. Support for Families and Communities
Family Support and Education Programs
- Government agencies fund family-oriented programs that educate family members on addiction and suicide prevention. SAMHSA’s Family Support Program provides resources to help families support their loved ones while maintaining healthy boundaries.
In summary, government interventions play a vital role in preventing suicide among individuals with substance use disorders. Through research, public education, crisis intervention, harm reduction, and expanded access to treatment, federal, state, and local governments can create a comprehensive system of care that reduces suicide risk and supports long-term recovery.
The Influence of Social Media on Addiction and Suicide Prevention
Social media has become a powerful tool for outreach, education, and support, offering unique opportunities to prevent suicide among individuals struggling with substance use disorders (SUDs). With millions of people engaging on platforms like Facebook, Instagram, Twitter, TikTok, and others, social media strategies can play a key role in raising awareness, providing resources, offering peer support, and connecting individuals to treatment services. Below are effective social media strategies to prevent suicide among substance abuse users:
1. Raising Awareness Through Educational Campaigns
Public Education Campaigns:
- Launching campaigns on social media platforms to educate the public about the relationship between substance abuse and suicide risk is crucial. These campaigns can:
- Highlight the signs of both substance use disorders and suicidal ideation.
- Provide statistics about the prevalence of suicide among individuals with addiction.
- Educate the public about the connection between mental health and substance use.
- Promote the importance of seeking help and normalizing conversations about mental health and addiction.
- Example: the #BreakTheSilence campaign on Instagram or Twitter, encouraging people to share their stories and reduce stigma.
Infographics and Shareable Content:
- Create visually appealing and easy-to-understand infographics that share facts about substance use, mental health, and suicide prevention. Shareable content can quickly reach a broad audience, especially when accompanied by a strong call to action (e.g., “Call the Suicide Prevention Lifeline” or “Find treatment options here”).
Hashtag Campaigns:
- Use targeted hashtags to raise awareness and create community engagement. Examples include #EndTheStigma, #SpeakUpAboutMentalHealth, or #RecoveryIsPossible, which can spread information and develop conversations around addiction and suicide prevention.
2. Providing Direct Access to Resources and Support
Linking to Crisis Resources:
- Frequently post links to suicide prevention hotlines (like the 988 Suicide & Crisis Lifeline) and substance use disorder resources (e.g., SAMHSA helpline, treatment centers).
- Pin essential resources at the top of social media profiles for easy access.
- Encourage followers to share these resources within their communities.
Virtual Peer Support Groups:
- Use platforms like Facebook Groups, Discord, Reddit, or Instagram to create virtual spaces for individuals with substance use issues to connect. These groups can provide:
- Peer support
- Shared experiences
- Encouragement
- A safe space to discuss struggles with addiction and mental health
Online Support Communities:
- Partner with established online mental health and addiction support communities (e.g., Reddit’s r/addiction, r/mentalhealth, or Sober Grid) to share valuable information, resources, and offer virtual check-ins.
3. Using Influencers and Ambassadors to Reduce Stigma
Influencer Partnerships:
- Collaborate with mental health advocates, recovery influencers, and public figures who have lived experience with addiction or suicide prevention to share messages of hope and recovery.
Celebrity Endorsements and Testimonials:
- Celebrities or public figures who are open about their struggles with substance use or mental health can normalize the conversation.
- Example: A celebrity sharing their story about seeking help for substance abuse, addiction recovery, or overcoming suicidal thoughts can be powerful in reducing stigma and inspiring others.
4. Live Streaming and Interactive Sessions
Live Q&A with Experts:
- Host live streaming sessions with mental health professionals, addiction counselors, or recovery coaches. These sessions can be interactive, allowing individuals to ask questions about substance use, mental health, coping strategies, and suicide prevention.
- Example: Live stream discussions on how to deal with cravings, how to talk to someone about suicide prevention, or how to build a healthy support system.
5. Promoting Recovery and Hopeful Stories
Success Stories:
- Share stories of individuals who have recovered from substance use disorders and suicidal ideation. Personal stories can be highly motivating to others in similar situations.
- Encourage people to share their recovery journeys using hashtags like #MyRecoveryJourney or #SobrietyIsPossible.
6. Collaborations with Nonprofits and Public Health Agencies
Partnering with Nonprofits:
- Collaborate with organizations focused on suicide prevention, substance use recovery, and mental health, such as AFSP, SAMHSA, or NIDA.
Public Service Announcements (PSAs):
- Governments and nonprofit organizations can use social media to share PSAs on the importance of mental health and addiction treatment.
- Example: A video series about how the brain responds to addiction and the importance of early intervention.
7. Interactive Features and Tools
Polls and Surveys:
- Use polls or surveys to engage followers and gather insights into their mental health and substance use experiences.
Mindfulness and Stress Reduction Challenges:
- Encourage followers to engage in activities that reduce stress and anxiety, such as mindfulness exercises, journaling, or meditation challenges.
8. Monitoring and Moderating Content
Content Moderation:
- Social media platforms can implement automated systems or employ mental health professionals to monitor content for harmful or triggering behavior.
Safe Communities:
- Create online support groups that foster a safe environment and enforce strict moderation policies to protect individuals from harmful comments or interactions.
In summary, social media strategies for preventing suicide among substance abuse users rely on creating a culture of awareness, education, peer support, and access to resources. By leveraging social media’s reach, fostering open conversations, offering real-time support, and providing educational and inspirational content, these platforms can be a lifeline for those in need. Collaborative efforts among mental health professionals, influencers, nonprofits, and individuals can create a powerful online community that promotes recovery and provides the support needed to prevent suicide.
Society’s Influence on Addiction and Suicide: Shaping a Culture of Prevention and Support
The societal landscape plays a crucial role in shaping attitudes, behaviors, and access to support systems for individuals struggling with substance use disorders (SUDs) and suicidal ideation. Cultural change strategies can significantly impact the way addiction and mental health are perceived, helping to reduce stigma, promote recovery, and create an environment that supports individuals at risk.
1. Reducing Stigma Around Addiction and Mental Health
Normalize Conversations About Mental Health and Addiction
- One of the most significant cultural barriers to seeking help for substance use and suicidal ideation is stigma. Society must recognize addiction and mental health conditions as treatable medical conditions rather than moral failings.
Public Awareness Campaigns
- Government agencies, nonprofits, and mental health organizations can lead national campaigns to educate the public that addiction and mental illness require treatment, not shame. Initiatives such as “Not One More” and #EndTheStigma on social media can shift public perceptions.
Storytelling and Personal Testimonials
- Encouraging individuals to share their lived experiences through blogs, social media, interviews, or books can humanize addiction and mental health struggles, fostering empathy and understanding.
Educating the Public on the Link Between Addiction and Suicide
- Public education campaigns should highlight how untreated addiction contributes to mental health challenges, increasing suicide risk. Schools, workplaces, and media outlets can collaborate to raise awareness about this critical connection.
Changing Media Representation
- The media plays a significant role in shaping public attitudes. Partnering with content creators to ensure accurate and compassionate portrayals of addiction and recovery can help reduce stigma and inspire hope.
2. Building a Supportive Community and Social Environment
Fostering Compassionate Communities
- Communities that promote empathy and support can provide crucial emotional and practical assistance to individuals facing addiction.
Community Programs
- Local initiatives, including recovery support groups, peer mentoring, and educational workshops, can create strong support networks.
Encouraging Empathy in Schools
- Teaching emotional intelligence and empathy from an early age can help future generations better understand addiction and mental health challenges.
Creating Safe Spaces for Dialogue
- Non-judgmental spaces such as support groups and online forums can encourage open discussions about addiction and mental health struggles.
Workplace Support Systems
- Employers can create a culture that normalizes seeking help by providing Employee Assistance Programs (EAPs), mental health days, and an open environment for employees to discuss their needs.
3. Promoting Education and Awareness Across Society
Mental Health and Substance Use Education
- Ensuring accessible education on addiction and mental health at all levels can empower people to recognize warning signs and seek help.
Curriculum Development
- Schools and universities should integrate substance use and mental health education into curricula to equip students with the necessary knowledge and skills.
Workplace Training
- Implementing wellness programs, mental health first aid training, and suicide prevention workshops in workplaces can create a more supportive environment.
Public Education Campaigns for Families
- Providing families with resources and workshops can help them support loved ones struggling with addiction without enabling harmful behaviors.
Parenting Programs
- Encouraging open conversations between parents and children about substance use and mental health can help build resilience and awareness from an early age.
4. Encouraging Early Intervention and Prevention
Strengthening Early Intervention Systems
- Early intervention should be viewed as an opportunity for healing rather than failure. Training educators, healthcare providers, and law enforcement to recognize early warning signs is crucial.
School-Based Programs
- Schools can offer mental health screenings and peer-support programs to encourage early intervention.
Health Education Campaigns
- Governments can sponsor initiatives that emphasize recognizing early warning signs of addiction and suicide risk, reducing harm before crises emerge.
5. Improving Access to Treatment and Support
Shifting Cultural Attitudes Toward Seeking Help
- Society must redefine seeking help as a strength rather than a weakness, encouraging individuals to pursue recovery without fear of judgment.
Healthcare Providers’ Role
- Medical professionals should emphasize the benefits of early treatment and integrate mental health screenings into routine care.
Expanding Access to Affordable Treatment
- Policymakers must work to eliminate financial and logistical barriers to treatment, ensuring that support is available to underserved and marginalized communities.
6. Incorporating Indigenous and Culturally Sensitive Approaches
Culturally Tailored Programs
- Recognizing the unique needs of Indigenous and immigrant populations is essential. Programs should integrate culturally relevant and trauma-informed approaches to addiction and suicide prevention.
Community-Based and Culturally Relevant Support
- Traditional healing practices and community-centered approaches can enhance effectiveness in diverse populations.
Advocacy for Minority Mental Health
- Targeted awareness campaigns can help address disparities in mental health and substance use treatment among minority groups.
7. Leveraging the Role of Technology and Social Media
Using Technology to Promote Awareness and Support
- Digital platforms, apps, and social media can help spread messages of hope, connect individuals with resources, and reduce stigma.
Digital Mental Health Platforms
- Online forums, teletherapy services, and mobile applications can expand access to counseling and peer support.
Influencer and Celebrity Advocacy
- Public figures can play a decisive role in normalizing mental health conversations and promoting recovery.
In summary, creating a cultural shift to address addiction and suicide prevention requires systemic change in how society perceives and responds to these challenges. By reducing stigma, increasing awareness, fostering compassion, and expanding access to treatment, society can build a more supportive environment where individuals struggling with substance use disorders feel empowered to seek help. These cultural strategies are essential in preventing suicide and promoting long-term recovery.
Frequently Asked Questions
Here are some common questions:
Question: What are the signs that addiction will turn into suicide?
Answer: Addiction and suicide are closely linked, as substance use disorders (SUDs) can worsen mental health conditions, increase impulsivity, and lead to feelings of hopelessness. Here are some key warning signs that addiction may escalate into suicidal ideation or attempts:
1. Worsening Mental Health Symptoms
- Persistent hopelessness or despair – Expressing thoughts like “Things will never get better” or “I don’t see a way out.”
- Severe depression or anxiety – Increasing emotional distress, withdrawal from activities, and lack of interest in life.
- Increased isolation – Avoiding friends, family, or support groups, preferring to be alone.
2. Escalating Substance Use
- Binge use or increased frequency – Using substances more often or in larger amounts to numb emotional pain.
- Polydrug use – Mixing substances (e.g., alcohol with opioids or stimulants), which increases overdose risk.
- Loss of control – Being unable to stop using despite severe negative consequences.
3. Expressing Suicidal Thoughts or Behaviors
- Talking about death or suicide – Statements like “I wish I weren’t here” or “Everyone would be better off without me.”
- Making indirect references – Writing goodbye letters, giving away possessions, or discussing what life would be like without them.
- Previous suicide attempts – A history of attempts increases the risk of future suicide.
4. Social and Behavioral Changes
- Extreme mood swings – Sudden shifts from deep sadness to appearing oddly calm or resolved.
- Withdrawing from relationships – Cutting off communication or avoiding responsibilities.
- Engaging in reckless behavior – Driving under the influence, unsafe sexual behavior, or engaging in fights.
5. Physical and Psychological Signs of Decline
- Neglecting self-care – Poor hygiene, malnutrition, or lack of sleep.
- Unexplained injuries – Possible self-harm or previous suicide attempts.
- Decline in job or school performance – Struggling with basic daily tasks and responsibilities.
6. History of Trauma or Loss
- Recent significant loss – Death of a loved one, breakup, job loss, or financial crisis.
- Unresolved trauma – Childhood abuse, neglect, or PTSD that worsens with substance use.
7. Access to Means of Suicide
- Stockpiling pills, buying weapons, or researching methods – A strong warning sign requiring immediate intervention.
- Engaging in risky overdoses – Using dangerous amounts of substances without regard for survival.
What to Do If You Recognize These Signs
- Encourage professional help – A therapist, addiction specialist, or crisis hotline can offer immediate support.
- Reach out and listen – Let them know you care, without judgment.
- Limit access to lethal means – Remove weapons, excess medications, or substances from their environment.
- Support harm reduction efforts – Encourage safer substance use practices if quitting isn’t immediately possible.
If someone is in immediate danger, call emergency services or a crisis hotline. Early intervention can save lives.
Question: What are resources and strategies to prevent addiction and suicide?
Answer: Resources and Support Strategies for Addiction and Suicide Prevention
If you or someone you know is struggling with addiction and suicidal thoughts, some resources and strategies can provide support and guidance.
Crisis Support Resources
Emergency and Crisis Hotlines
- National Suicide Prevention Lifeline (U.S.) – Dial 988 (24/7 confidential support)
- Crisis Text Line – Text HELLO to 741741 (24/7 support via text message)
- SAMHSA’s National Helpline – Call 1-800-662-HELP (4357) for substance use treatment referrals
- Veterans Crisis Line – Dial 988, then press 1 (for veterans and military service members)
- Trevor Project (LGBTQ+ support) – Call 1-866-488-7386 or text START to 678678
- Local Emergency Services – If there is an immediate danger, call 911 (or the emergency number in your country).
Support Strategies for Prevention and Recovery
1. Seeking Professional Help
- Therapy and Counseling – A licensed therapist or counselor specializing in addiction and mental health can help develop coping strategies.
- Psychiatrists and Medication Management – If needed, medication for depression, anxiety, or addiction (e.g., Suboxone, Naltrexone) can be part of treatment.
- Rehabilitation Programs – Inpatient or outpatient addiction treatment centers offer detox, therapy, and relapse prevention.
2. Building a Support Network
- Family and Friends – Open, non-judgmental communication with loved ones can provide emotional support.
- Support Groups – Organizations like Alcoholics Anonymous (AA), Narcotics Anonymous (NA), or SMART Recovery offer peer-based support.
- Peer Recovery Coaches – Some communities provide trained individuals in recovery who help guide others through the process.
3. Self-Help and Coping Strategies
- Journaling – Writing about emotions and triggers can help safely process thoughts.
- Mindfulness and Meditation – Reducing stress and increasing emotional awareness can help prevent impulsive behaviors.
- Physical Activity – Exercise releases endorphins, which improve mood and reduce cravings.
- Creative Outlets – Art, music, and writing can be therapeutic tools for expressing emotions.
4. Reducing Access to Lethal Means
- Safe Medication Storage – Lock away or limit access to large amounts of medications.
- Firearm Safety – Store guns securely or remove them from the home if suicidal thoughts are present.
- Supervised Substance Use – If quitting immediately isn’t possible, harm reduction strategies (e.g., supervised injection sites, naloxone for overdoses) can prevent fatal outcomes.
5. Addressing Root Causes
- Trauma-Informed Care – Many with addiction and suicidal thoughts have unresolved trauma; working with a trauma-informed therapist can help.
- Financial and Housing Support – Accessing social services, shelters, or employment programs can reduce stressors that contribute to substance use.
Online and Digital Resources
- FindTreatment.gov – Locate addiction treatment centers in the U.S.
- To Write Love on Her Arms (TWLOHA) – Mental health and addiction awareness resources.
- r/stopdrinking and r/addiction (Reddit) – Online peer support communities for those in recovery.
- Apps for Mental Health & Sobriety –
- Sober Grid (connects people in recovery)
- WEconnect (helps track recovery goals)
- Calm / Headspace (guided meditation for stress and anxiety)
Encouraging Early Intervention
Promote Community Awareness – Educate others about addiction and suicide prevention through schools, workplaces, and local events.
Talk About It – Addressing concerns early can prevent a crisis.
Encourage Help-Seeking – Normalize therapy, support groups, and professional treatment.
Question: What to do during an acute suicidal crisis?
Answer: Acute Suicidal Crisis steps for help
If someone is experiencing an acute suicidal crisis, immediate action is critical to ensure their safety. Here’s what to do:
1. Assess Immediate Danger
- Are they in immediate danger? If they have a weapon, have taken a hefty dose of drugs/alcohol, or are making active plans, call 911 (or the emergency number in your country) right away.
- Ask Directly: “Are you thinking about suicide?” Asking does NOT increase the risk—it shows that you care and can open the door to help.
2. Stay With Them
- Do not leave them alone if they are actively suicidal.
- Remove or secure lethal means (e.g., firearms, medications, sharp objects).
- Encourage them to breathe slowly if they are panicking.
3. Call for Help
- Emergency Services (911) – If they are in immediate danger.
- 988 Suicide & Crisis Lifeline (U.S.) – Dial 988 for free, confidential support.
- Crisis Text Line – Text HELLO to 741741 (24/7 support via text).
- Local Mental Health Crisis Teams – Many areas have mobile crisis units that can respond to the person rather than the police.
4. Listen Without Judgment
- Be calm and patient—your reaction matters.
- Validate their feelings: Say, “I hear you, and I want to help you get through this.”
- Avoid saying things like “Just think positive” or “You have so much to live for” (these can feel dismissive).
5. Get Them to a Safe Place
- Take them to an ER, crisis center, or a trusted person’s home where they can be monitored.
- If they refuse help but remain at risk, contact a crisis professional or local authorities for a welfare check.
6. Encourage Professional Support
- Help them call a therapist, doctor, or crisis hotline for a safety plan.
- If they are under the influence, medical detox or stabilization may be needed first.
7. Follow Up After the Crisis
- Check in frequently to show continued support.
- Help them set up therapy, support groups, or a treatment plan.
If YOU Are in Crisis
Create a safety plan: Identify triggers, coping strategies, and emergency contacts.
Tell someone you trust.
Call 988 or a crisis hotline.
Go to the nearest hospital or crisis center.
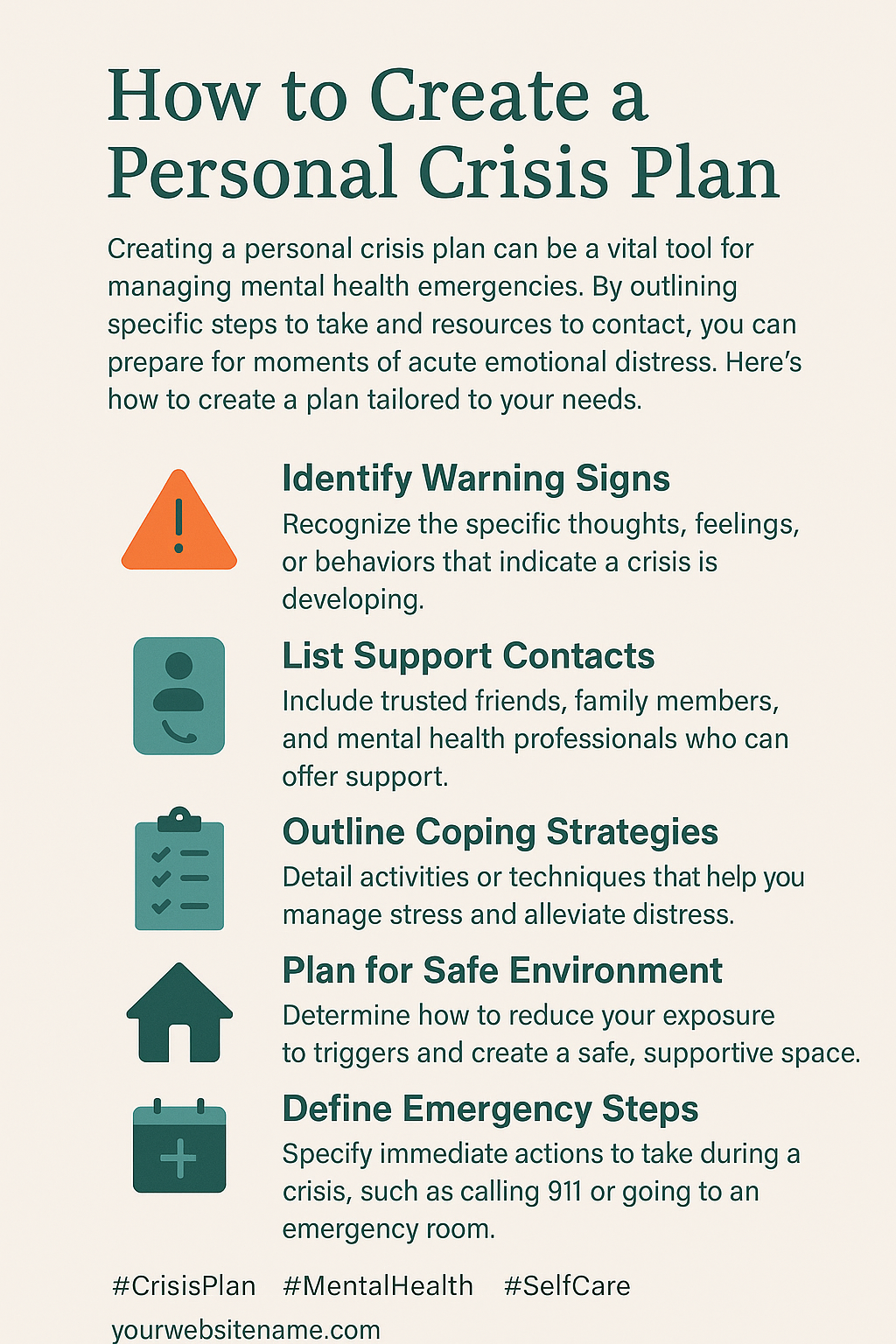
Question: How to create a personal crisis plan?
Answer: Creating a personal crisis plan can help you or a loved one navigate a mental health crisis, including suicidal thoughts or urges. Here’s how to develop one:
1. Identify Warning Signs
Recognize the emotions, thoughts, or behaviors that indicate a crisis is developing. Examples:
- Increased feelings of hopelessness
- Withdrawing from loved ones
- Increased substance use
- Thinking about self-harm or suicide
2. List Coping Strategies
Write down healthy ways to cope with distress without relying on others. Examples:
- Deep breathing, meditation, or grounding techniques
- Listening to music or engaging in a hobby
- Exercising or going for a walk
3. Identify Supportive People
List trusted friends, family, or support groups who can help during a crisis.
- Name and contact information of at least three people
- Consider professional support, like therapists or crisis hotlines
4. Create a Safe Environment
Remove access to anything that could be used for self-harm, such as firearms, medications, or sharp objects.
- Ask someone to hold onto dangerous items if needed
- Plan a safe place to go if home isn’t supportive
5. Emergency Contacts and Crisis Hotlines
Keep a list of immediate help resources:
- 988 Suicide & Crisis Lifeline (U.S.)
- Local crisis centers or mental health professionals
- 911 or emergency services if danger is imminent
6. Make a Plan for Seeking Help
Write down steps to take when you feel overwhelmed, such as:
- Try coping strategies.
- Contact a support person.
- Call a crisis hotline or therapist.
- Seek emergency help if necessary.
A crisis plan should be written down and easily accessible. Share it with trusted individuals so they can support you if needed.
Conclusion
Suicide risk among individuals with substance use disorders is a complex issue influenced by multiple factors, including mental health co-occurrence, social isolation, and demographic variables. Addressing this risk requires a comprehensive approach that integrates self-management techniques, strong family support, accessible community resources, effective government policies, social media campaigns, and cultural shifts towards greater understanding and empathy. By combining these strategies, we can reduce stigma, promote healthier coping mechanisms, and create an environment that encourages help-seeking behaviors. Ultimately, a holistic, multi-pronged approach is crucial in preventing suicide and supporting individuals on their journey to recovery.
Video: The Shocking TRUTH About Addiction and Suicide
Warning Signs That Addiction May Lead to Suicide
The RIGHT Way to Help Someone Suicidal
How a Crisis Plan Can Save Your Life