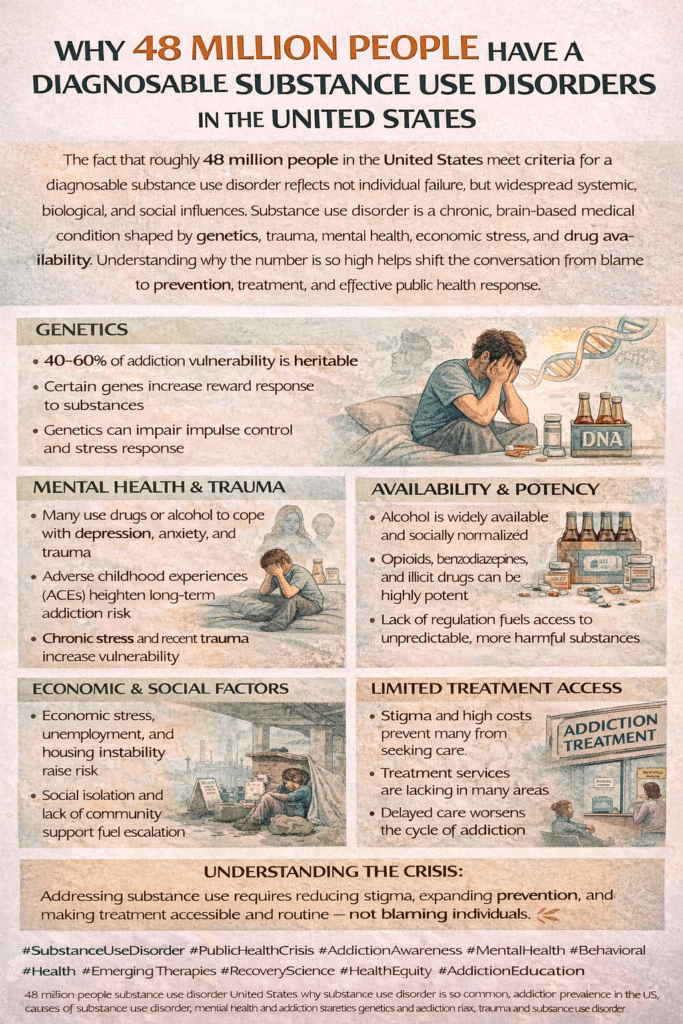
Substance use disorders touch millions of lives across the United States. With 48 million people living with a diagnosable substance use disorder (SUD), it’s an issue that’s woven deeply into the fabric of many communities. Understanding the reasons behind these numbers and what helps or hinders recovery sheds light on both the problem and the steps that really help people affected by SUDs.
The Scope of Substance Use Disorders in the US
A substance use disorder means having patterns of using alcohol or drugs that lead to health problems, trouble in daily life, or both. According to the 2022 National Survey on Drug Use and Health, nearly 1 in 5 Americans aged 12 or older fit this description. These numbers haven’t popped up randomly; the increase has slowly built up over the years, influenced by cultural changes, medical practices, stress, and accessibility of substances.
Alcohol ranks as the most commonly misused substance, followed closely by prescription painkillers, cannabis, and stimulants. Recent surges in opioid addiction, fueled first by prescription opioids and then by synthetic drugs like fentanyl, have made grim headlines for a reason. The impact stretches to emergency rooms, families, workplaces, and entire communities throughout the country.
Young people and adults alike face risk, though the patterns of which substances are most popular can mix it up across age groups. Substance use often starts in adolescence, with experimentation, peer influence, or attempts to handle stress—all of which set the stage for possible problems later.
Why Are So Many People Struggling With SUD?
No one chooses to end up with a substance use disorder. Multiple forces come into play, often combining in individual ways for each person.
- Genetics and Family History: People with close relatives who struggle with addiction are more likely to develop issues themselves. Genes and shared environments both play a role.
- Mental Health Conditions: Depression, anxiety, PTSD, and trauma in general are all linked with a higher risk for SUD. Sometimes, people use substances to deal with emotional pain or to feel temporary relief, and that cycle can be tough to break.
- Social and Environmental Factors: Peer pressure, social networks, stress at home or work, childhood neglect, and growing up in communities where substance use is common can increase a person’s risk. Lack of access to positive activities and safe environments can also worsen things. Socioeconomic difficulties and a lack of support can further increase these risks.
- Availability of Substances: It’s much easier to fall into a problem if alcohol or drugs are cheap and easy to get. The US has seen periods where doctors overprescribed medications or new drugs hit the streets, giving more people a chance to try and get hooked.
- Stigma and Denial: Sometimes people don’t seek help because they’re worried about being judged, or they don’t think their use is a problem, especially if those around them use too. Worries about privacy or legal consequences often prevent people from reaching out when they need to.
All these factors often mix together in complicated ways, making prevention and recovery uniquely challenging for each individual.
How the Brain Changes With Addiction
Substance use disorder isn’t just about willpower or bad choices. Repeated drug or alcohol use changes how the brain works, especially in areas that control judgment, decision-making, pleasure, and self-control. The longer someone uses, the more their brain gets wired to crave those substances just to feel normal.
People with SUD might keep using even when they really want to cut down, showing that addiction becomes a mental health challenge—one that often needs professional care, not just tough love. These brain changes can last even after someone stops using a substance, leading to cravings or even relapse. This is important for friends, families, and communities to understand, so that support can focus on long-term help rather than judgment.
Brain science research now shows that recovery is possible because the brain is plastic—meaning it can adapt and shift over time with effort, support, and treatment. But time, patience, and understanding remain critical during this healing period.
How Did We Get to 48 Million? Major Shifts Behind the Numbers
- Prescription Drug Waves: Through the 1990s and 2000s, opioids were widely prescribed, often without full awareness of the risks. Many people who started with painkillers later transitioned to illegal drugs.
- Increased Stress and Uncertainty: Stressful periods, such as the COVID-19 pandemic, economic downturns, and rising living costs, lead some to turn to substances to cope. Rates of alcohol and drug use rose during and after the pandemic, especially among adults.
- Cultural Changes: Changing attitudes about certain drugs, such as cannabis, becoming legal in more states, have influenced use rates. While legalization has positive outcomes, it sometimes leads to increased use and makes it seem less risky, especially for young people. Ongoing conversations about safe use and public health are important.
- Fentanyl and Synthetic Drugs: Illicit drug markets have changed, with synthetic opioids being much more powerful and dangerous. Overdose deaths have spiked, especially in the last decade, turning some SUDs deadly much more quickly. The fast rise of these substances has caught many off guard and raised the stakes on prevention efforts.
Beyond these big trends, things like changing laws, social media influence, and new ways of accessing substances online keep shaping the SUD landscape in the US.
Barriers That Stand in the Way of Recovery
- Lack of Access to Care: Not enough treatment centers or professionals, especially in rural or low-income urban areas, means people can’t get help when they want it. Long waitlists and limited resources make it harder to get started on the path to recovery.
- Cost and Insurance Hurdles: Treatment can be pricey, and not everyone has insurance that covers the care they need, whether it’s inpatient rehab, medication, therapy, or ongoing support. Even those with insurance may face high copays or coverage limits.
- Stigma: People worry about being labeled, losing jobs or custody, or being looked down on, which stops them from reaching out. The fear of discrimination or judgment sometimes outweighs the urge to seek help.
- Lack of Mental Health Support: Many people with addiction also battle depression, trauma, or anxiety. Without help for those issues, it’s tough to stay on track. Integrated mental health and substance use treatment is still lacking in many places.
A strong support system, empathy from others, and easy access to quality care all help people push past these barriers. But we still have a way to go as a country. Raising public awareness, increasing funding for treatment, and emphasizing compassion over punishment are all important steps for meaningful progress.
Steps to Prevent and Treat Substance Use Disorders
While SUDs impact millions, recovery and prevention are possible, and they work best when personal and community support come together. Solutions need to address the different roots of SUD and the various paths to healing.
- Prevention Programs: Schools, workplaces, and community groups offering honest, age-appropriate education about drugs and alcohol have proven to help lower rates of use, especially among teens. Interactive education, mentoring, and skill-building can all be tools for prevention.
- Early Intervention: Spotting trouble early, like catching risky drinking patterns or prescription misuse, gives people a better shot at steering clear of long-term problems. Doctors, teachers, and parents can make a difference by speaking up before substance use spirals out of control.
- Treatment Options: Effective treatment looks different for everyone. For some, it’s therapy or medication-assisted treatment (MAT) like Suboxone or methadone for opioids. For others, peer support, 12-step programs, or inpatient care is most helpful. The main thing is having options and a plan that fits each person. Ongoing support and follow-up can give people the best odds of making long-term changes.
- Building Community Support: Shame and isolation worsen SUD. Involving family, friends, or recovery coaches encourages people to stay in recovery and avoid relapse. Trained peers and support groups can be especially valuable. Whole communities can get involved through coalitions, public awareness campaigns, and making resources visible and accessible.
- Improving Laws and Policies: Public health approaches, such as expanding treatment funding, making naloxone available, or changing how courts and police respond to people with SUD, can help entire communities turn the tide. Redirecting resources from punishment to treatment and support is a proven way to make a difference over time.
Personalized prevention and treatment pave the way for stronger communities and brighter futures for those at risk or in recovery.
Frequently Asked Questions About Substance Use Disorders
Question: Can substance use disorders happen to anyone?
Answer: SUDs affect people of all backgrounds. Some are at higher risk because of family history or life circumstances, but anyone can be impacted.
Question: What signs might show someone needs help?
Answer: Warning signs include using more than intended, not being able to cut down, spending a lot of time getting or using substances, or failing to meet responsibilities at work, home, or school because of use. Withdrawal symptoms, sudden mood changes, and legal trouble can also signal a problem.
Question: Are there treatments that really help?
Answer: Yes, a range of treatments can help, from therapy and medication to support groups and lifestyle changes. What helps most varies by person and situation. Checking with a trusted healthcare provider or seeking out local resources is a smart move. Taking the first step by asking for help can make recovery possible.
Question: What should someone do if they or a loved one is struggling?
Answer: Reaching out to a doctor, counselor, or local support group is a strong first step. The Substance Abuse and Mental Health Services Administration (SAMHSA) offers a free, confidential helpline at 1-800-662-HELP (4357). There are also many websites and community organizations ready to support recovery at every stage.
Why Tackling SUDs Really Matters for Everyone
Every stat about substance use disorder in the US represents a real person, plus their friends and family. Addressing the reasons for SUD—like mental health, social situations, and the effects of drugs on the brain—makes a difference for whole communities. Supporting prevention, breaking down stigma, and improving access to good care offer hope for change.
Wrapping up, it’s clear that SUDs aren’t just numbers on a chart. They touch lives everywhere. By working together—supporting individuals, sharing resources, and speaking openly about recovery—we can help more people move toward healing. More resources and info for supporting yourself or a loved one can be found at SAMHSA and CDC Drug Overdose.
Video: 48 Million People Share This One Thing #SubstanceUseDisorder #Genetics