Mixing medications and alcohol is often overlooked until a problem arises, but the consequences can be severe. While having a drink while taking certain medications might seem harmless, the interactions can be unpredictable, sometimes leading to severe side effects or dangerous reactions. Even everyday combinations, like common over-the-counter drugs and alcohol, can catch people off guard, affecting everything from liver function to coordination, judgment, and heart health. In this guide, I’ll break down why it’s essential to pay attention, highlight which medication and alcohol combos are especially risky, and provide practical tips for staying safe if you’re managing prescriptions or over-the-counter medications while occasionally drinking. Understanding these interactions can help prevent accidents, protect your health, and make informed choices about your well-being.
Why Mixing Medications and Alcohol Can Be Risky
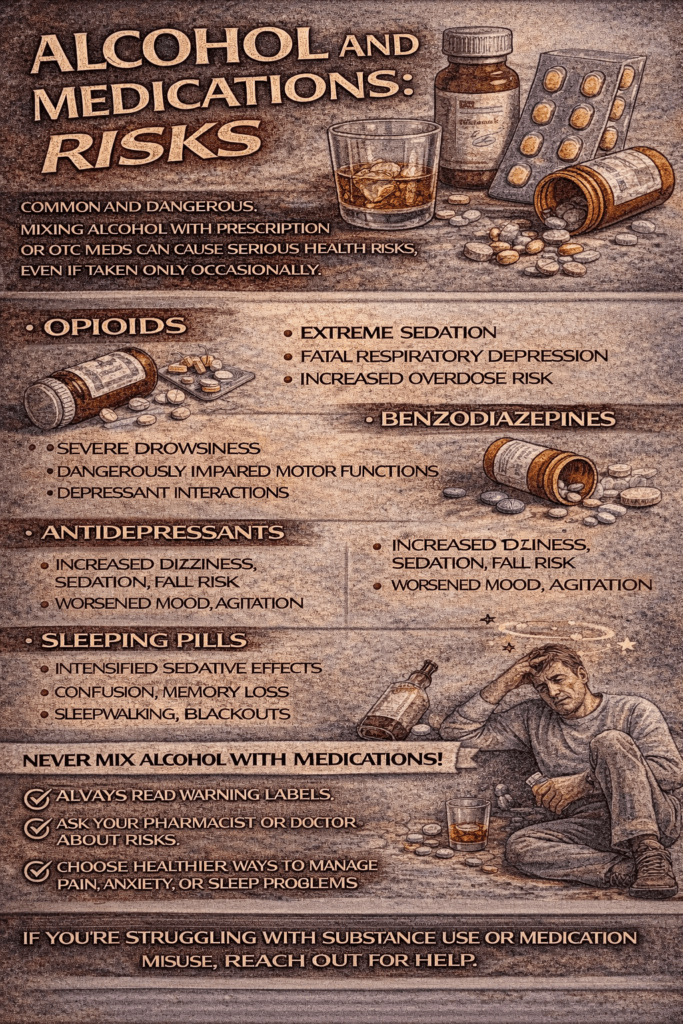
Medications each have their own science regarding how the body processes them. Tossing alcohol into the mix messes with this balance. Alcohol can make some medicines weaker, but it can also make others way stronger than intended. That goes for everything from painkillers to antidepressants to everyday allergy pills. Sometimes, the reaction doesn’t show up until you suddenly feel off at a party, which can get dangerous in a hurry.
Both alcohol and a lot of meds are broken down in the liver. When both hit your system together, your liver works overtime. This double-duty stresses your liver and can mess with how well your body breaks down. This means a med might stick around longer or not work at all. This is especially true for anyone with existing liver or kidney issues.
What Types of Medications React with Alcohol?
Some meds come with obvious warning labels, but not all do. I’ve found that some of the most common types taken daily are the ones where the mix is the most unpredictable. Here are the medication types where it’s essential to think twice before reaching for a drink:
- Pain Relievers (like acetaminophen or ibuprofen): Combining these with alcohol can hurt your liver or stomach, sometimes leading to ulcers, bleeding, or even liver failure if it’s a regular habit.
- Antibiotics: A few can spark reactions that leave you nauseous, dizzy, or with a pounding heart. Not every antibiotic interacts badly, but some, like metronidazole, are known for it.
- Antidepressants and Anxiety Meds: Alcohol can mess with how well your brain chemicals balance out, making anxiety or depression worse, and reducing your meds’ effect. Some meds can boost sleepiness or dizziness, so driving or working is much more difficult.
- Sleep Meds or Sedatives: Drinking on these can make you super drowsy, affecting coordination and memory. The risk for accidents increases, and breathing can slow down more than you think.
- Blood Pressure Meds: Alcohol can make you dizzy or faint by dropping your blood pressure extra low, especially after you stand up fast.
- Diabetes Meds: Drinking can make blood sugar drop really fast, which can be dangerous for anyone on insulin or pills that lower blood sugar.
- Allergy and Cold Meds (antihistamines, decongestants): The combo with alcohol can majorly increase drowsiness or make it harder to focus, even if you only had one drink.
How Alcohol Affects Medication in the Body
The science behind alcohol and medication interactions is all about metabolism. When both hit the liver at the same time, the liver prioritizes breaking down alcohol over meds, especially if you drink often. This means your medication can build up to higher-than-normal levels pretty quickly. On the flip side, some meds need the liver to turn them “on,” but alcohol can mess with that and leave you without the full benefit of your prescription.
Alcohol also bumps up side effects for a lot of meds, like making you sleepier, more forgetful, or even more uncoordinated than usual. This is especially true for anyone feeling slightly off when starting a new prescription.
One thing I always remind friends and readers: a reaction doesn’t just happen on hard liquor. Even beer or a glass of wine can cause trouble with certain meds. Reactions can hit on the same day or take a while to show up, depending on how your body handles the mix.
Common Reactions to Watch Out For
Most people expect to feel nothing or think, “What’s the worst that could happen?” when they mix a pill with a drink. Sometimes, it works out with no drama. But a lot of times, you might get:
- Nausea and vomiting
- Bad headaches
- Dizziness or feeling extra lightheaded
- Heart palpitations or chest pain
- Sleepiness or trouble staying awake
- Trouble breathing (especially with sedatives)
- Problems with memory and concentration
If any of these hit out of nowhere after drinking with medications, it’s time to slow down and maybe check in with a healthcare provider or pharmacist. Things like bad allergic reactions or trouble breathing are medical emergencies and need immediate attention.
Unexpected Drug-Alcohol Combinations to Keep in Mind
Sometimes it’s surprising which medications can trip you up when mixed with alcohol. For example, certain antifungal meds and even some anti-nausea pills don’t play well with alcohol, causing unpleasant or even dangerous symptoms. Another less talked about example is medication for motion sickness (like scopolamine), which can cause extreme drowsiness or confusion when mixed with drinks. Steroids, when combined with alcohol, can put extra stress on your stomach and increase the risk of ulcers. If you’re taking prescription migraine meds, drinking alcohol may not only reduce the effectiveness but can also bring on worse side effects or even trigger an attack. That’s why checking every prescription, over-the-counter remedy, and supplement for alcohol warnings can save you from a rough surprise.
Don’t forget about herbal supplements. Some, especially those for sleep or anxiety relief (like valerian root or kava), may make you even more drowsy or woozy when mixed with alcohol. This can be risky, especially if you need to stay alert, so always consider this if you use natural remedies in your daily routine.
A Few Scenarios Where Talking with a Professional Is Really Smart
I’ve had friends and readers send questions about everything from cough syrup combos to mixing the daily antidepressant with a weekend cocktail. Here are a few times I always suggest looping in a doctor or pharmacist before mixing:
- Starting a new prescription (because reactions sometimes only show up the first few times)
- Taking multiple medications at once
- If you have a health condition where your liver or kidneys are already under stress
- If you’re on meds that warn against operating machinery or driving
Doctors and pharmacists are super used to these questions and would rather help you avoid a problem than end up in urgent care because of a simple combo.
Everyday Tips for Staying Safe with Meds and Alcohol
I’ve found that a few habits make a huge difference when it comes to avoiding bad reactions:
- Check Labels and Ask Questions: Always read medication labels and ask your pharmacist what’s safe, even for short-term medications like antibiotics or cold pills.
- Pace Yourself: If you drink, keep it light. Small amounts are less likely to cause problems, especially if you’re on low-risk meds, but still pay attention to how you feel.
- Time Your Doses: Sometimes spreading your medication and a drink by several hours can lower risk, but it should always be checked with a professional first. Some combos aren’t safe at any distance.
- Stick to Your Treatment Plan: Don’t skip doses or stop meds early to drink. This can throw off your health plan and cause more trouble later.
- Know When to Skip the Drink: If you’re feeling sick, on antibiotics, or your meds make you tired or dizzy, skipping that drink for a few days is the safer option.
What If You Already Mixed Alcohol and Medication?
If you realize you drank after taking medicine, don’t panic. Most of the time, if you feel fine, all you need to do is be extra aware of changes in your body or mood. If you notice anything off, like a rapid heartbeat, severe dizziness, vomiting, or trouble breathing, don’t wait it out. Contact your local poison control or head into urgent care for a check-up. Better safe than surprised by a nasty reaction.
Frequently Asked Questions
There’s a lot of confusion about what’s really risky when it comes to alcohol and medications. Here’s what I get asked the most:
Can I have just one drink while taking antibiotics?
Answer: It depends on the antibiotic. Some, like metronidazole or tinidazole, can cause severe reactions with even a sip of alcohol. Always check with your doctor or pharmacist.
Is beer or wine safer than hard liquor with medications?
Answer: No type of alcohol is “safe” with certain meds. The alcohol itself is the problem, not the drink’s strength or style.
How long should I wait after finishing a course of meds before drinking again?
Answer: This depends on the medication. Some leave your system fast; some linger a while. Your pharmacist can give you a specific time frame for your prescription.
What’s the worst that can happen if I mix meds and alcohol?
Answer: Sometimes nothing happens, but sometimes you can get really sick. The risk runs from mild (like feeling off balance or sleepy) to life-threatening (like severe allergic reactions or dangerous changes in heart rhythm). It’s not something to gamble on without professional guidance.
Wrapping Up
Mixing medications and alcohol is a lot more common than most people realize, but the risks are also bigger than they seem at first. Being smart about what’s in your system, asking questions, and double-checking labels goes a long way. Your pharmacist is a great resource. They’ve helped me and plenty of others avoid dangerous mix-ups, and they’ll do the same for you.
If you have doubts, contacting a healthcare professional is a simple, safe move. Staying cautious with alcohol while on medication helps you stay healthier and feel better; you don’t have to be sidelined by something completely preventable. Whether you take meds long-term or occasionally, a little planning can make a big difference for your safety and peace of mind.
Video: Never Mix These 5 Drugs With Alcohol!