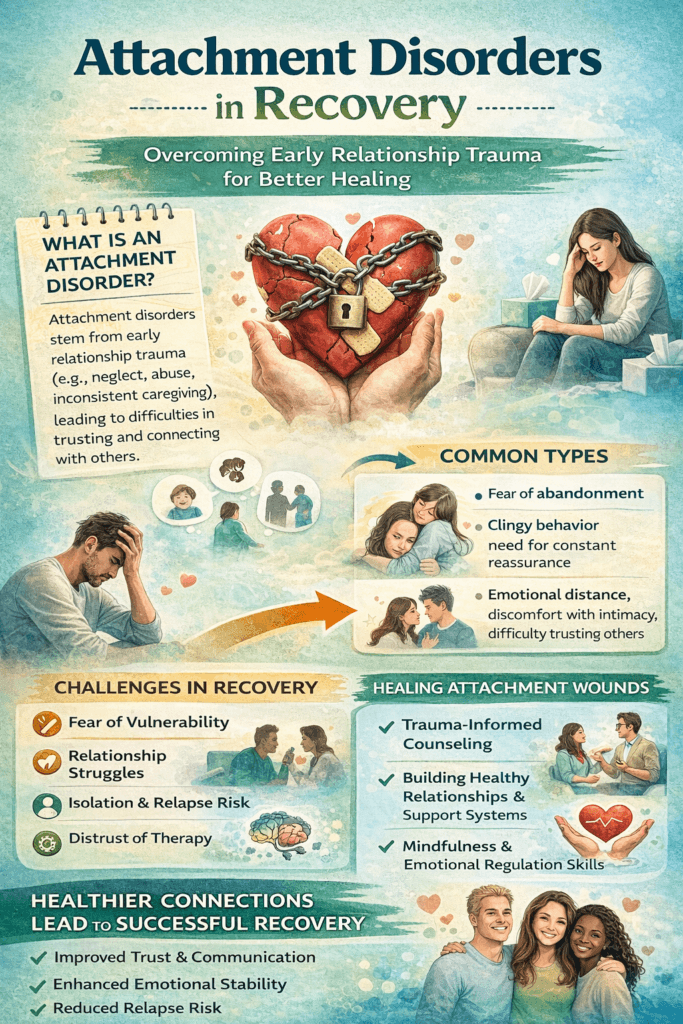
Attachment disorders come up more often than you might think in conversations about mental health and recovery. For anyone working towards emotional well-being, these patterns can shape the way relationships work, how support is received, and even the path to healing. Understanding what attachment disorders are and how they affect the recovery adventure can make a huge difference if you’re navigating tough experiences or supporting someone else.
What Are Attachment Disorders?
Attachment disorders usually show up in early childhood when the bond between a child and caregiver isn’t strong, secure, or consistent. These early relationships lay the groundwork for how we relate to others and regulate emotions as adults. When those first experiences go wrong, maybe due to neglect, trauma, or lots of sudden changes, attachment doesn’t always develop the way it should. As a result, people might find it hard to trust, connect, or feel safe in relationships.
The two main types most folks talk about are Reactive Attachment Disorder (RAD) and Disinhibited Social Engagement Disorder (DSED). RAD often leads to trouble forming close relationships, while DSED is marked by overly familiar behavior with strangers. Both can seriously influence how a person approaches future relationships and how they ask for or accept help down the road.
How Attachment Shapes Recovery
The impacts of attachment run deep, especially during recovery from any tough experience like addiction, complex trauma, or even a mental health diagnosis. When early bonds feel shaky or unreliable, trust doesn’t come easily later in life. Trust is pretty important when you’re working through tough changes or new emotions.
A person with an insecure or disorganized attachment style may struggle to believe that treatment providers, support groups, or even close friends really have their back. This can show up as resistance to therapy, pulling away from group work, or sabotaging relationships just when they get too close. Trust issues can become a recurring roadblock in the recovery process, even after progress is made.
Recognizing Signs of Attachment Disorders
Spotting the signs early can make things much easier. While only a trained professional can diagnose an attachment disorder, there are some things people commonly notice:
- Difficulty trusting others: Taking a long time to warm up or being suspicious of motives.
- Struggles with boundaries: Either being too distant or too close too quickly.
- Emotional numbness or outbursts: Finding it tough to control or even feel emotions in certain situations.
- Fear of abandonment: Worrying about being left, even without any clear reason.
- Avoiding closeness: Shying away from deeper connections and support, especially when stressed.
These patterns don’t disappear just because someone commits to recovery. They often pop up during stressful times, like when starting therapy, moving into a sober living environment, or facing emotional triggers. Being aware of these signs can help guide treatment and foster patience for yourself and anyone you might be supporting.
Attachment Styles and Recovery: What to Watch For
Attachment theory isn’t only about disorders. It also offers a helpful way to look at common relationship patterns, known as “attachment styles.” These styles can give you some clues about what might help or hinder your path in recovery:
- Secure attachment: Comfortable with closeness and independence, so reaching out for help usually isn’t too hard.
- Anxious attachment: Worries about being abandoned, so there’s often a need for extra reassurance.
- Avoidant attachment: Needs lots of independence, might avoid opening up or reject help even when it’s needed.
- Disorganized attachment: Flips between closeness and withdrawal, sometimes reacting unpredictably or with intense fear.
Attachment-related struggles can slow down recovery by making it tough to trust others, stick with support groups, or even acknowledge when something feels vulnerable or overwhelming. Recognizing your own patterns can be pretty helpful for tailoring recovery plans that actually stick. If your style isn’t secure, it doesn’t mean all hope is lost. It just points to certain challenges you might face, and knowing them can help you address them head-on.
Sometimes, even after understanding your attachment style, it can take time to adjust and feel comfortable in supportive environments. Recovery often involves unlearning habits and expectations formed in early relationships, so give yourself credit for each bit of progress, no matter how small.
Strategies For Managing Attachment Challenges in Recovery
Finding your way through attachment issues doesn’t mean progress is impossible. In fact, awareness is a real asset. There are practical strategies you can start using right away:
- Form Consistent Support Networks: Regular interaction with the same group of people (therapists, group members, mentors) helps build a sense of safety over time. Consistency is key to creating a sense of belonging and trust.
- Practice Open Communication: Small steps in honest sharing—even saying “I find it hard to trust right now”—can slowly break down barriers. Being open about your hesitations might also help others better support you.
- Work With Specialists: Therapists trained in attachment-focused approaches (like Emotionally Focused Therapy or Trauma-Informed Care) have strategies that really help. Don’t hesitate to ask about their experience with attachment challenges.
- Set Manageable Goals: Instead of expecting to “fix” attachment overnight, celebrate small wins, like showing up or reaching out for help. Recognition of progress fuels motivation and keeps you moving ahead.
- Mind-Body Connection: Practices like yoga, mindful breathing, or grounding help regulate emotions and make tough moments feel less overwhelming. Mindbody activities can provide a sense of stability when emotions get intense.
- Educate Yourself: Learning about attachment styles through books or reputable websites can empower you to spot patterns and understand your own reactions and those of others.
- Create Structure: Daily routines and predictable schedules give a sense of safety when other parts of life feel unpredictable.
I’ve seen firsthand how small steps add up, especially if you work alongside trusted professionals who understand attachment. Progress might not always feel fast, but with patience and the right support, things do move forward.
Common Challenges: What to Expect and How to Cope
When working on recovery alongside attachment wounds, a few themes tend to recur. Knowing about these ahead of time means fewer surprises and more realistic expectations:
- Fear of intimacy: Even with the intention to heal, old fears of closeness can quickly return. This is normal and often needs gentle, nonjudgmental support.
- Struggles with boundaries: Setting limits feels risky for many. Practicing saying “no” or “not yet” helps create more comfortable interactions over time.
- Setbacks following progress: It’s common for old patterns to show up when things seem to be improving. Recognizing these moments as part of the process makes it easier not to give up.
- Doubt in the process: Trust doesn’t build overnight, and skepticism about therapy or group support is normal. Each positive experience helps reinforce new beliefs.
- Feeling out of place: If you grew up in an environment that didn’t nurture attachments, joining a group or community can feel overwhelming at first. Over time, repeated positive interactions can boost feelings of belonging and safety.
Working with a therapist or a well-informed peer group can really help make these challenges less daunting. Remember, relapses into old patterns are a normal part of healing, not a failure. Gentleness with yourself is critical.
Helpful Resources and Approaches
Treatment options for attachmentrelated issues have come a long way. Some approaches I’ve found to be especially supportive include:
- Attachment-Based Therapy: Focuses on repairing early attachment wounds and building healthy relationship skills. These therapies use techniques designed to help you create new, more reliable ways of connecting.
- Trauma-Informed Counseling: Recognizes the way trauma affects attachment, creating a safer, more supportive environment for healing. Understanding the link between trauma and attachment can transform recovery approaches.
- Group Therapy: Offers real-time feedback and connection in a safe context, which can be tricky but very valuable for relearning trust. In groups, there’s an opportunity to experiment with new social skills and receive gentle feedback.
- Family Therapy: When possible, working on family relationships can help change old patterns and create better support networks. Involving key people from your life in the recovery process can strengthen those ties.
- Peer Support Groups: Groups that focus on shared experience can make you feel less alone and offer practical tips and encouragement.
- Creative Arts Therapies: Art or music therapy lets you express feelings nonverbally, which is often easier when words are hard to find.
Websites like Attachment Project and NIMH have more information and can point you towards therapists trained in these approaches. Tools like books, podcasts, and online communities focused on attachment and recovery are also worth checking out.
If you’re not sure where to start, your primary care provider or a school counselor can be a first point of contact. Many local mental health centers also offer group sessions or educational workshops.
Attachment Disorders in Everyday Life
Attachment issues don’t just affect therapy. They show up in lots of ways, from work relationships to parenting to friendships. For example, someone with avoidant attachment might prefer solo projects and struggle with asking for help, while someone with an anxious style might feel left out or worried about being replaced at work. Parents with an attachment issue may find it hard to connect or respond to their child’s needs, creating a new cycle without meaning to.
Once you notice these patterns, it becomes easier to handle them with a bit more compassion and flexibility, rather than falling back into frustration or self-blame. Recognizing the impact, without shame, is the first step toward breaking free from the cycle.
It’s helpful to remember: having an attachment disorder isn’t a reflection of your character or a life sentence. It’s a response to early experiences, and there are plenty of tools to help change old patterns. Change takes time, but every effort counts and every positive connection helps build a new foundation.
Frequently Asked Questions
Here are some questions that often come up about attachment and recovery:
Question: Can adults heal attachment issues from childhood?
Answer: Yes, adult brains are capable of growth and change, especially with support, therapy, and safe relationships.
Question: Do attachment disorders always come from trauma?
Answer: Not always. Sometimes they’re linked to ongoing stress, frequent separations, or inconsistent caregiving, not just traumatic events.
Question: Should I tell my therapist if I think I have an attachment disorder?
Answer: Definitely. Bringing it up can help your therapist understand your responses and tailor the treatment to what works best for you.
Question: How long does it take to see positive change with attachment work?
Answer: The timeline varies, but small improvements often show up within a few months of consistent effort, especially when supported by professionals. Be patient with yourself and celebrate progress.
Final Thoughts
Living with attachment disorder can affect every part of daily life and the entire recovery path, but these patterns aren’t set in stone. Awareness, support, and reliable guidance all play big roles in helping you develop healthier, more rewarding connections, both with others and with yourself. Each step, no matter how small, opens up more possibilities for growth, healing, and connection down the road.
Video: