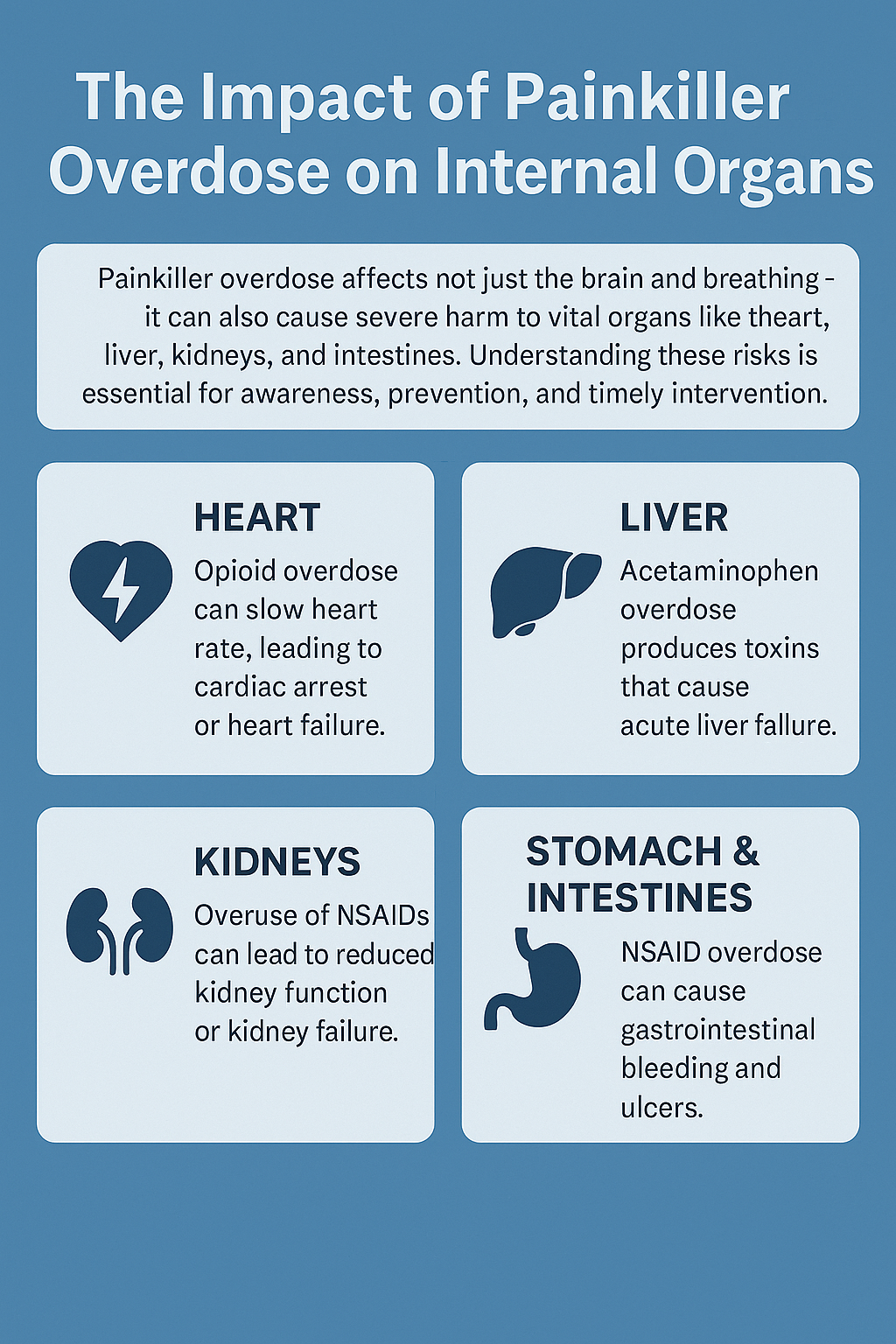
Painkillers often seem harmless—something we keep in the cabinet and reach for without a second thought. They’re widely available, frequently prescribed, and can feel like a miracle when pain hits. But when taken in higher doses than recommended, they can quietly cause serious harm to vital organs like the liver, kidneys, and heart. What starts as short-term relief can lead to long-term damage or even organ failure, especially with repeated misuse. Overdose doesn’t always happen suddenly—it can build up over time as toxins accumulate. Understanding these effects is key to protecting your health and using painkillers safely.
The Basics: How Painkiller Overdose Happens
Painkillers come in a couple of forms, but the most common you’ll see are over-the-counter meds like acetaminophen (Tylenol), ibuprofen, and prescription opioids such as oxycodone, hydrocodone, and morphine.
An overdose can be intentional or accidental. Sometimes people lose track of how much they’ve taken, especially when combining different medications. At other times, someone might take more in the hope of more substantial pain relief. The problem is that large amounts push organs way past their limits. The body can only handle so much before things go downhill.
According to the CDC, painkiller overdoses, especially involving opioids, are a leading cause of accidental poisoning. Even nonopioid painkillers like acetaminophen can be dangerous in high doses and definitely shouldn’t be shrugged off as harmless.
Your Liver: The Frontline for Processing Painkillers
The liver’s job is to break down most painkillers and get rid of toxins. Taking higher doses than suggested puts the liver under extra pressure. Acetaminophen overload, for example, is a serious risk and is actually one of the leading causes of sudden liver failure in many countries.
When you take too much acetaminophen, the breakdown products build up and start hurting liver cells. The symptoms might begin with nausea, loss of appetite, or tiredness, but things can spiral to jaundice (yellowing skin or eyes), confusion, or even coma when the liver stops working as it should.
Chronic painkiller use, even if you don’t technically “overdose,” can slowly damage the liver over time. This kind of damage isn’t always apparent at first, but it accumulates over ongoing misuse. Some people discover the issue only after running routine lab tests or noticing unusual tiredness and abdominal discomfort.
Your Kidneys: Filtration Gets Overwhelmed
Your kidneys function like high-end filters, removing waste and excess toxins from the blood. If you overload them, especially with NSAIDs (like ibuprofen or naproxen) or high doses of other painkillers, they can start to fail. Acute kidney injury can show up as reduced urine, swelling, and high blood pressure.
Repeated overdoses or heavy use can lead to chronic kidney disease. You might not notice changes until things get pretty serious, so it’s easy to let this slip by until the damage is advanced. If someone already has kidney problems, the risk climbs even higher. In my experience, talking with healthcare professionals, people are often unaware of these dangers and may overlook subtle symptoms like swelling or foamy urine that signal kidney issues.
Heart and Lungs: More Than Just a Side Effect
Painkiller overdose can affect your cardiovascular system, too. Opioids, for example, slow down the parts of your brain that control breathing. When taken in large amounts, breathing can get dangerously slow or even stop altogether. That is a medical emergency.
Some painkillers mess with your heart rhythm or raise blood pressure. In severe cases, they can trigger heart attacks or contribute to heart failure, especially if you already have underlying heart problems. Shortness of breath, chest pain, or a sudden loss of alertness are signs that require immediate medical attention. Sometimes, people taking combinations of painkillers and other medications can face exceptionally high risks due to unintended interactions.
Your Digestive System: Gut Trouble from Overdose
The stomach and intestines often react quickly when someone takes too many painkillers. Nausea, vomiting, constipation, and stomach pain usually show up. With repeated high doses, ulcers or bleeding in the stomach can develop, especially with NSAIDs.
Liver failure from acetaminophen overdose can also build up toxins that affect your digestion and appetite. These symptoms aren’t just uncomfortable; they’re signals that something might be wrong deeper down the line. People sometimes ignore these warning signs, assuming it’s a typical stomach bug, but persistent GI symptoms always warrant attention.
Brain and Nerves: When Overdose Hits Your Headspace
Opioids and other strong painkillers can cause confusion, dizziness, or even seizures when abused. Heavy use sometimes triggers hallucinations or makes you extra tired, or conversely, jumpy and restless. When organs like the liver or kidneys start to fail, toxic byproducts can affect the nervous system, leading to brain fog, personality changes, or more severe mental changes.
People who overdose sometimes pass out or fall into a coma. This isn’t just a risk in the moment; it can mean permanent brain damage if oxygen to the brain drops, especially with opioid overdoses that slow breathing way down. Even friends or family witnessing these changes may not always realize a medical emergency is happening until it’s nearly too late.
Why Painkiller Overdose is Dangerous, Even if You “Feel Fine”
A painkiller overdose doesn’t always come with dramatic, Hollywood-style symptoms. Sometimes the damage builds without obvious warning signs. For example, someone who takes a bit too much acetaminophen a few days in a row may not feel different at first, but liver damage is already in progress.
Other signs can be relatively mild, such as feeling tired, changes in urine color, or mild stomach pain. That’s why paying attention to how much you’re taking and not doubling up on meds with the same active ingredient is super important. It’s worth noting that kids and older adults are especially vulnerable to these subtle presentations, so families should stay alert to any new or unexpected symptoms.
Common Challenges Around Recognizing and Avoiding Overdose
- Mixing Medications: Many cold, flu, and pain medicines contain acetaminophen. Accidentally doubling or tripling your dosage is easier than you might think if you’re not checking labels.
- Hidden Medical Conditions: Not everyone knows they already have mild liver or kidney disease. If your organs aren’t at full power, even a “regular” amount of painkillers might be risky.
- Prescription Confusion: Opioid medications come in different strengths and sometimes have complicated dosing. Unclear instructions or poor communication raise the risk of taking too much.
- Social Pressure or Misinformation: Sometimes, well-meaning friends or online posts may share misleading tips about safe doses, making it harder for people to practice safe habits.
Mixing Medications
It’s really common for people to take more than one product for different symptoms. Stomach pain, a cold, or a headache can all prompt someone to reach for the medicine cabinet. I’ve found that a quick check of the active ingredients on the label helps me avoid doubling up on something like acetaminophen. Online medication checkers can also help you sort out which medications you’re taking and alert you to duplicates.
Preexisting Health Conditions
If you already have kidney or liver problems, it’s worth asking a doctor or pharmacist before taking any new painkiller. The safe “normal” dose could be different for you than for someone else, and certain underlying conditions can make painkillers more dangerous, even at standard doses. This is especially true for seniors, those with chronic illnesses, or anyone taking multiple medications.
Staying Safer: Actionable Tips and Real-Life Scenarios
- Read labels and instructions carefully. Even over-the-counter meds can be tricky, so double-check what’s in them and if you’re already taking something similar.
- Set a reminder for doses. It sounds basic, but having a phone reminder or sticky note helps if you’re managing more than one medication. Apps that track your medication schedule are excellent tools to help you stay organized and safe.
- Keep meds out of reach of kids or other family members. Accidental overdose is common in children who find and swallow pills—store painkillers in a locked drawer or high cabinet to prevent accidents.
- Talk to your doctor or pharmacist, especially before mixing meds, or if you’re unsure about the correct dose. Even if you think you know your medications, it’s always a good idea to double-check with a professional, especially if your health or medication regimen has changed.
- If you notice any unusual symptoms, contact a professional immediately. Trouble breathing, yellowing skin, extreme confusion, or severe stomach pain aren’t things to ignore. Early intervention can make a critical difference.
Another helpful tip: keep an updated list of all medications (prescriptions, over-the-counter pills, and supplements) and bring it to every medical appointment. This helps your healthcare team spot any interactions or risks.
Frequently Asked Questions
Here are some questions people often ask about painkiller overdoses and their effects on organs.
Question: How fast does liver damage happen after an acetaminophen overdose?
Answer: Liver damage can start as early as eight hours after an overdose. The risk increases the longer it takes to receive treatment. In some cases, even smaller overdoses repeated over several days can trigger severe liver problems, especially if you drink alcohol or have other health concerns.
Question: Are natural painkillers safer for organs?
Answer: Some natural remedies may be easier on the liver or kidneys, but they aren’t always proven to work, and they can interact with prescription meds. It’s a good idea to consult with a healthcare professional before making any changes to your treatment plan. Even herbal supplements can sometimes stress your organs or mix badly with regular medications.
Question: What should I do if I realize I took too much of a painkiller?
Answer: Call Poison Control or go to the nearest ER right away, even if you feel okay. Early treatment can significantly impact recovery. Don’t wait for symptoms to appear, since organ damage can start well before you feel sick. Bring the pill bottles with you so the medical team knows precisely what you took.
The Takeaway: Understanding the True Risks and Protecting Yourself
Painkiller overdose isn’t only about the short-term scare of feeling sick. It’s about the real risks it poses to vital organs, such as the liver, kidneys, heart, and brain. Recognizing the early warning signs of trouble, understanding how different medications affect your organs, and seeking professional advice can significantly lower your risk of long-term harm. Treat medications with respect, ask questions, and keep your health at the center of any choices you make around pain relief. Sharing this information with friends and family can also help keep everyone safer and more informed.
Video: Painkillers Can Seriously Damage Your Organs!