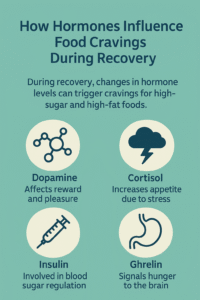
Food cravings can feel overwhelming and unpredictable, especially during recovery from addiction, illness, injury, or surgery. When the body is healing, it’s not just the mind seeking comfort—your hormones are shifting, too, and that can send strong signals to eat certain foods. I’ve found that understanding what’s going on inside my body helps me respond with awareness instead of frustration. Hormones such as cortisol, insulin, ghrelin, and serotonin all play significant roles in shaping appetite and cravings. Stress can spike cortisol and make you reach for sugary or fatty foods, while low serotonin may trigger cravings for carbohydrates to boost mood. Even changes in sleep, activity levels, or medication can disrupt hunger cues. Recognizing that these cravings often have a biological cause—not just a lack of willpower—can make it easier to manage them with patience and healthier choices. Here’s how hormones shape those urges during recovery and what you can do to keep them in check.
Why Hormones Matter in Recovery-Related Food Cravings
Hormones act as the body’s messengers, carrying signals from one organ to another through the bloodstream. When you’re recovering, your hormone levels can change pretty dramatically. Stress, pain, inflammation, and changes in your routine or medication can all disrupt the balance of key hormones, often leading to sudden cravings or shifts in appetite that may come as a surprise.
Some of the main hormones involved in food cravings during recovery include:
- Ghrelin: Known as the “hunger hormone,” ghrelin makes you feel hungry and is often higher when your body needs to repair itself.
- Leptin: This hormone signals fullness. Inflammation or disrupted sleep during recovery can make it harder for leptin to do its job, leading to more frequent cravings.
- Cortisol: Stress increases cortisol levels, which are associated with cravings for sugary or high-fat foods.
- Insulin: Changes in activity and diet during recovery can alter how your body uses insulin, which sometimes leads to erratic energy fluctuations and cravings.
- Serotonin and Dopamine: These “feel-good” brain chemicals can drop during tough times, making carb-heavy or comforting foods feel extra appealing.
Getting a sense of these hormones gives you clues about why sudden urges for chocolate, chips, or random food combos might pop up as your body bounces back.
Common Types of Cravings During Different Kinds of Recovery
Cravings won’t look the same for everyone, but I’ve noticed some recurring patterns depending on the type of recovery you’re moving through:
- After Surgery or Illness: Protein cravings can spike because your body is deep in repair mode. At the same time, you may crave salty foods if you’ve lost a significant amount of fluid or feel weak due to not eating enough. Sweet cravings appear as your body seeks quick energy to heal.
- During Substance Abuse Recovery: Carbohydrate cravings (especially for sweets) are very common. Your body is rewiring its reward systems and seeking ways to stimulate those “feel-good” chemicals again.
- Injury Recovery: Boredom, pain, or stress can set off cravings for comfort foods that distract from discomfort or help you cope with downtime.
These cravings are your body’s way of signaling its needs, or sometimes its attempt to self-soothe. Knowing this can help alleviate some of the guilt or confusion surrounding why you suddenly want that bag of gummy bears or a cheesy sandwich.
Significant Factors That Influence Cravings as Hormones Switch Up
Several factors contribute to fluctuations in your hormones (and, consequently, your cravings) during recovery periods. Here are a few main factors to keep in mind:
- Sleep Disruption: Poor sleep is a common occurrence during recovery, which can lead to increased ghrelin levels and decreased leptin levels. That combination can lead to late-night snacking or cravings for calorie-dense foods.
- Medications: Pain meds, steroids, antidepressants, and other needed drugs can change how your body handles hunger and fullness or even trigger new cravings.
- Pain and Stress: The body releases cortisol in response to stress or pain, driving cravings for comfort foods such as sweets, chips, and takeout.
- Physical Activity Changes: If you’re moving a lot less, your body may be confused about its new energy needs. Sometimes, the result is odd or fluctuating food cravings as your metabolism adjusts.
- Emotional Ups and Downs: Recovery is a rollercoaster, and emotions interact directly with dopamine and serotonin. Both brain chemicals are linked to appetite and cravings, so mood switches can nudge you toward eating as a pick-me-up.
Innovative Ways to Manage Food Cravings During Recovery
Cravings are a standard part of recovery, but I’ve found specific strategies helpful in making them less disruptive. Here are a few that I stick with:
- Balance Your Meals: Eating meals that combine protein, healthy fats, and whole grains helps keep blood sugar steady, which can tamp down sudden cravings.
- Stay Hydrated: Sometimes, I mistake thirst for hunger. Sipping water all day makes a huge difference.
- Get Consistent Sleep: Adhering to a regular sleep schedule helps maintain balanced hunger hormones.
- Plan Satisfying Snacks: Having snacks that contain fiber, healthy fats, or a bit of protein around helps keep cravings from spiraling. Try apple slices with peanut butter or plain Greek yogurt with berries.
- Find Non-Food Rewards: Picking up a favorite book, calling a friend, or taking a walk (if you’re able) can meet the need for comfort without always heading straight to the kitchen.
- Talk With a Pro: Registered dietitians or therapists can help you spot patterns, make lasting changes, or build positive habits if cravings start to feel tough to manage.
Extra Things to Watch Out for When Handling Hormone-Related Cravings
- Binge Eating: Recovery can sometimes trigger patterns where emotional eating turns into overeating. If you notice this, know that it’s not uncommon, and plenty of support is available.
- Undereating: Pain, nausea, or stress during recovery can make eating less appealing, even with cravings present. Your body still needs energy to heal, so finding easy-to-digest, appealing foods is crucial.
- Restrictive Diets: While it’s tempting to eliminate certain foods, allowing yourself to eat a variety (including those that satisfy cravings) in moderation can help lower stress and may reduce obsessive cravings over time.
Hormones That You’re Most Likely to Notice
A handful of hormones stand out for their impact on cravings, especially during recovery:
- Cortisol: A significant contributor to stress eating, cortisol often prompts you toward sweet and salty snacks.
- Ghrelin and Leptin: These are your main hunger and fullness signals. When they get out of balance, cravings become a lot tougher to ignore.
- Serotonin: During tough recovery periods, low moods and pain can reduce serotonin levels, leading to an increased craving for carbohydrates such as bread, pasta, and sweets in the brain.
Learning to spot which hormones might be behind your cravings can help you sort out what kind of self-care or snack will genuinely help.
What About Hormones and Specific Food Types?
Sometimes, certain hormones are linked with cravings for particular foods. For example:
- Sweet Cravings: Usually tied to low serotonin or a drop in dopamine, these cravings grow strong in the late afternoon or evening, particularly if you’re tired or stressed.
- Salty Cravings: These may occur when your body needs a quick energy boost or a better electrolyte balance, sometimes triggered by cortisol surges during stress.
- Rich or Fatty Cravings: These foods tend to comfort and satisfy the appetite. Both cortisol and low serotonin can prompt your brain to crave fatty, comforting snacks during rough recovery days.
Knowing why you’re staring down the ice cream or chips can help you stumble upon a balanced way to indulge—or reach for something more nourishing that’ll actually scratch the itch.
Frequently Asked Questions About Hormones and Food Cravings During Recovery
How long do hormone-related cravings last after surgery or illness?
Cravings can last for weeks to a couple of months, depending on your recovery, sleep habits, and how you’re dealing with stress. As you heal and routines even out, hormone levels usually settle and cravings ease up.
Can medications make cravings worse?
Yes, certain medicines like steroids or antidepressants can pump up appetite or trigger new cravings as a side effect. If it’s all getting to be a bit much, check in with your doctor—they may be able to adjust your care plan or offer advice that helps.
Is it better to ignore cravings or try to satisfy them?
Trying to ignore cravings totally will usually make them stronger. Choosing to satisfy them with smaller portions or healthier versions of your favorite foods works better, helping you avoid overdoing it later on.
Should I be worried if my cravings feel out of control?
If cravings are so intense that they’re affecting your emotional health or making recovery harder, talk to a healthcare professional or registered dietitian. They can help you sort through what’s typical and where to get extra support.
What I’ve Learned About Steering Through Hormone-Driven Cravings
Hormones play a significant role in shaping food cravings throughout recovery. They’re influenced by stress, pain, routine changes, and the ups and downs that come with the healing process. Picking up on which hormones are running the show and using a few practical strategies makes it easier to roll with cravings, instead of letting them throw you off track. Paying close attention to your body’s signals can help you identify your comfort zone, heal more smoothly, and navigate recovery without guilt or confusion. If you feel stuck, reaching out for support is always a good idea. Remember, you don’t have to navigate it all alone.
Video: The Shocking Truth About Hormonal Cravings During Addiction Recovery