Skin lesions can pop up for a bunch of reasons, and using certain drugs is one that often surprises people. I’ve spoken with folks who found rashes, sores, or weird bumps after starting a new prescription or after experimenting with recreational drugs. It can be anything from a harmless blotch to something you really want to get checked out. Here, I’ll break down why skin lesions can show up when you’re using drugs, the types you might notice, how to spot the difference between a minor issue and something worrisome, and share some pointers on what steps to take if you notice changes in your skin.
Why Do Drugs Cause Skin Lesions?
Any drug you put in your body, whether prescribed, over the counter, or recreational, can mess with your skin in different ways. Some medications can cause side effects such as rashes or other skin problems. Others can trigger allergic reactions, make you more sensitive to sunlight, or disrupt your immune system. With recreational drugs, skin reactions can come from the drug itself or any stuff cut into it by dealers, which sometimes includes chemicals that aren’t exactly skin-friendly.
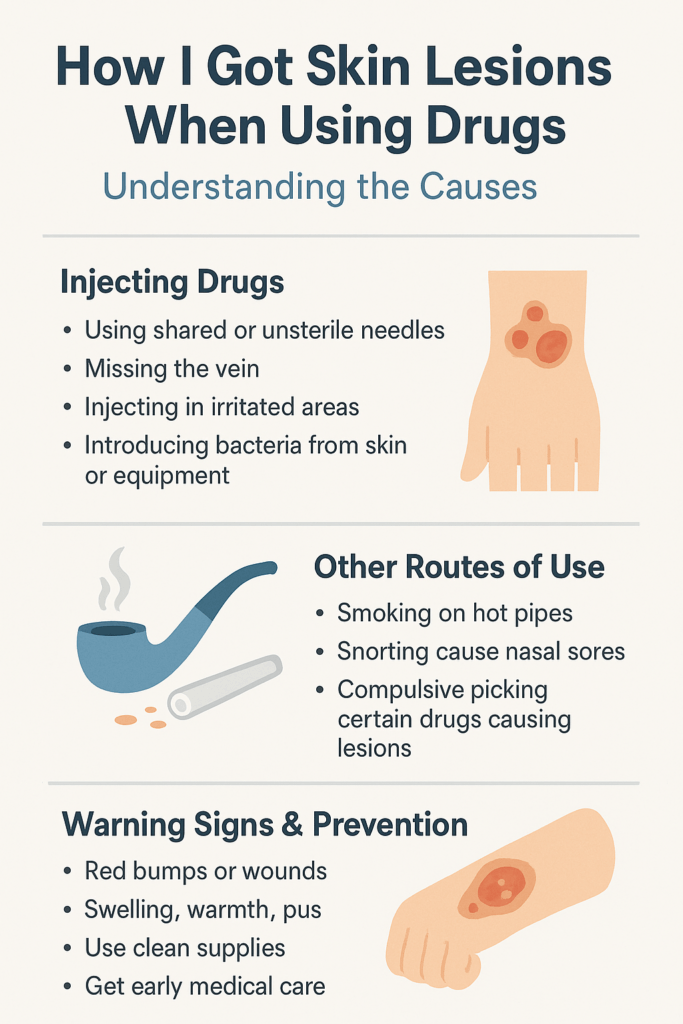
A few reasons you might see skin lesions from drugs include:
- Allergic Reactions: Some people’s immune systems don’t agree with certain medications, so they react by breaking out in hives, rashes, or red patches.
- Toxic Reactions: Some drugs or their breakdown products are harmful to the skin, leading to blisters, peeling, or sores.
- Direct Contact: If you inject or touch certain drugs, they can irritate or burn the skin right where they land.
- Lowered Immunity: Some drugs lower your body’s defenses, so bacteria and viruses sneak in and cause skin infections or sores that won’t heal.
Common Types of Skin Lesions Linked to Drug Use
Skin lesions can show up in a bunch of ways. Here are some you might see when drugs are involved:
- Rashes: These can be flat, raised, red, or itchy. Some look like tiny dots, others are more like big patches.
- Hives (Urticaria): These itchy welts pop up suddenly and can come and go pretty fast. They’re often a sign your immune system is reacting to a medication.
- Blisters: Some drugs can make your skin blister or peel, especially when there’s a severe reaction like Stevens-Johnson syndrome, which is actually pretty serious.
- Vasculitis Lesions: This means the blood vessels get inflamed, causing red or purple spots or patches, sometimes called purpura.
- Necrosis (Dead Skin): Injecting drugs, especially under less-than-clean conditions, can kill the skin or underlying tissue, causing ulcers or black, dead areas.
- Pigment Changes: Some drugs can make your skin lighter or darker in spots, especially if they affect hormones or your immune system.
Drugs Most Commonly Linked to Skin Problems
Some drugs and medications are more often associated with skin-related complaints. Here’s what I see most often:
- Antibiotics: Penicillin, sulfa drugs, and a few others can cause rashes or allergic reactions in some people.
- Anticonvulsants: Medications like phenytoin or carbamazepine can be harsh on the skin, sometimes leading to severe reactions.
- NSAIDs: Common pain relievers, like ibuprofen, can trigger rashes or hives in some cases.
- Street Drugs: Cocaine, heroin, meth, and designer drugs sometimes lead to skin infections, burns, or ulcers, depending on how they’re used and what else they’re mixed with.
- Blood Thinners: Drugs that thin the blood, such as warfarin, can sometimes cause bruises or purple spots under the skin.
- Corticosteroids: Taking steroids over long periods thins the skin, so it bruises, tears, and sometimes gets discolored.
Spotting the Difference: Mild vs Serious Lesions
Not every skin change needs a doctor’s appointment, but some are definite red flags. Mild drug-related rashes usually show up as pink or red spots that itch but don’t bleed, blister, or ooze. These rashes might fade on their own after a few days, especially if you stop the drug.
On the flip side, some lesions are signals that something pretty significant is happening inside your body. Watch for:
- Blisters or sores in your mouth, eyes, or genitals
- Large, peeling areas of skin
- Purple patches (“purpura”) that don’t blanch when pressed
- Ulcers that don’t heal or start to smell bad
- Any sudden, widespread rash with fever or joint pain
If you spot any of these symptoms, getting checked out right away is a good idea. Some of these could be early signs of severe allergic reactions or blood vessel inflammation that need attention fast.
What to Do If You Notice Skin Lesions
When your skin changes after taking a new drug or using something off the street, it’s tempting to ignore it and wait for things to clear up. I usually recommend taking a careful look at what’s going on:
- Stop using the drug or medication if you can safely do it and let your doctor know.
- Take photos of the lesions to track changes.
- Check the rest of your body for more spots, blisters, or swelling.
- See if you have any other symptoms, such as fever, trouble breathing, or pain.
- If you keep feeling worse or if the lesions get bigger or start bleeding, make an appointment with a healthcare provider, especially if you’re having symptoms that aren’t just on the skin.
Stuff That Can Make Skin Lesions Worse
Certain things can make drug-linked skin lesions feel worse or heal more slowly:
- Underlying medical problems: If you already have diabetes, immune system issues, or skin conditions, you might heal more slowly or get more infections.
- Poor wound care: Scratching, picking, or ignoring skin sores makes them worse.
- Mixing drugs: Combining medications or street drugs can lead to unpredictable reactions, including nastier rashes or blisters.
- Dirty needles or gear: Reusing needles or sharing drug equipment spreads bacteria and viruses, which easily turn minor sores into big infections.
Tips to Minimize Risk
Not all drug reactions are preventable, but you can do a few things to lower your chances of having problems with your skin:
- Let your doctor know about any drug or food allergies you have.
- Ask about common side effects whenever you start a new medication.
- If you’re using recreational drugs, avoid injecting or using equipment that isn’t sterile. It’s way safer for your skin and the rest of you.
- Catch problems early by checking your skin regularly for new spots, blisters, or other changes.
- If you notice something weird, don’t wait to ask a pharmacist or doctor about it, especially if you have other symptoms like a fever.
Frequently Asked Questions
Here are some common questions folks ask about skin lesions from drug use:
Question: Are all drug rashes dangerous?
Answer: Most drug-linked rashes are mild and clear up when the drug is stopped, but there are exceptions. A doctor should check out blisters, large, spreading rashes, and any sores, along with other symptoms.
Question: Why do some people get skin problems with drugs and others don’t?
Answer: Every person’s immune system and skin are different. Genetics, other medical conditions, and how your body metabolizes the drug all play a role.
Question: Is it safe to use a drug again after I had a skin reaction?
Answer: Even if the skin reaction was mild, repeating the drug could bring on a worse problem. Always check with your healthcare provider before starting it again.
Final Thoughts
Skin lesions that pop up after using drugs can be minor or point to something bigger happening in your body. Learning what’s normal and what’s worth worrying about makes it a lot easier to handle whatever comes up. Always reach out to a healthcare provider if you’re not sure. Catching issues early is significant for your health, skin, and peace of mind.
If you want to get a better sense of what different skin lesions look like, there are resources online from trusted health organizations. These can help you figure out whether what you’re seeing matches a common reaction or might need a closer look. And remember, photos tell a story—so taking pictures can help you and your doctor track changes over time. Don’t hesitate to reach out even if the change seems minor at first. Your skin can be a window to your overall health, so keeping an eye on it is never a wasted effort.
Video: Needle Infections That Turn Into Abscesses #medical #drugawareness