Pain is something just about everyone deals with at some point, but for a lot of people, pain sticks around a lot longer than they’d like. Long-term pain management isn’t only about popping a pill and moving on; it’s a complicated approach that often mixes medications, therapies, and regular check-ins. I’ve talked with people who’ve lived for years managing chronic pain, and what stands out most are the day-to-day side effects that can pop up along the way.
Understanding Long-Term Pain Management
Pain that sticks around for three months or more is usually called chronic pain. Common conditions include arthritis, back pain, nerve pain, and even certain headaches. These issues don’t just go away on their own, so doctors and specialists often turn to ongoing pain management plans. That can mean taking medications for months, or even years, alongside options like physical therapy, counseling, or alternative treatments.
Medications are a prominent part of this, but pain management is typically much broader. Some folks use a mix of nondrug therapies, gentle exercise, acupuncture, counseling, or even meditation techniques alongside their regular meds. Doctors keep an eye on long-term risks and help people adjust their plans to fit their daily lives. But even with a careful approach, some side effects can feel tough to handle.
Main Types of Pain Management Treatments
There isn’t really a one-size-fits-all answer when it comes to managing pain over the long haul. I find most people start with safer options and only bump up to stronger treatments if things aren’t working out.
- Nonsteroidal Anti-inflammatory Drugs (NSAIDs): These reduce inflammation and are great for things like arthritis or muscle aches, but they can upset the stomach over time.
- Acetaminophen: Super common for headaches or everyday pain, but too much can be heavy on the liver.
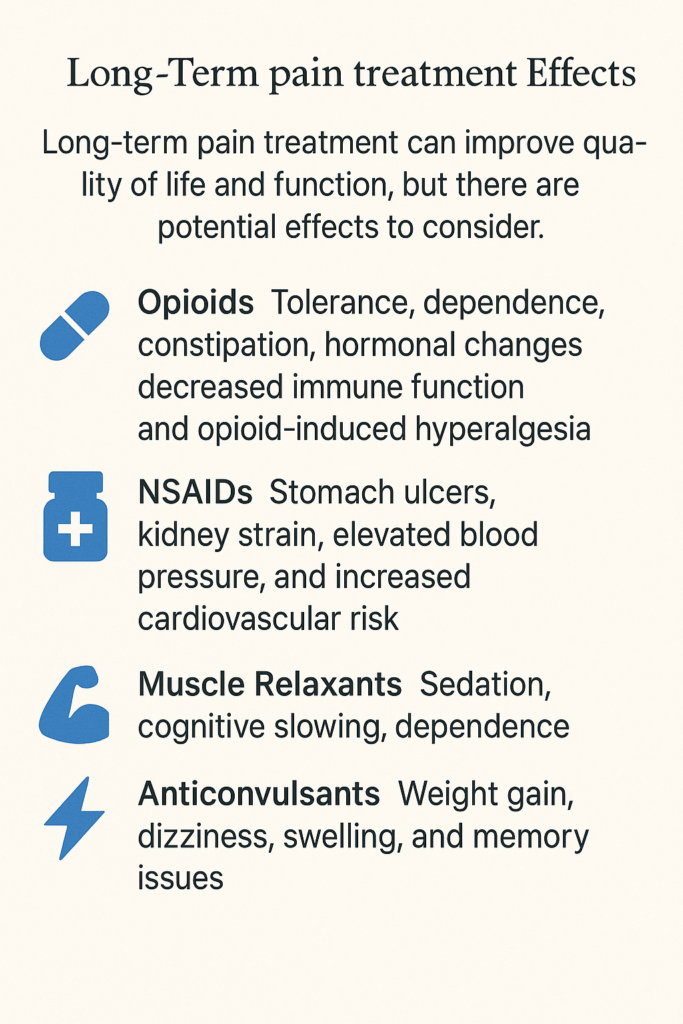
- Opioids: Reserved for more serious, long-lasting pain. While these can help, they come with risks of dependency and other side effects.
- Antidepressants & Anticonvulsants: Often prescribed for nerve pain or other chronic issues, not just depression or seizures.
- Topical Treatments: Creams or patches applied to the skin for targeted relief.
Physical therapy, counseling, stress reduction, and specific lifestyle changes are also part of a solid approach. Each method has its own quirks regarding side effects.
Common Side Effects of Long-Term Pain Medications
Taking something for pain every day can come with some annoyances. Some are mild and go away with time, but others stick around and need attention. Here are a few side effects I hear about the most:
- Digestive Issues: A lot of pain meds, like NSAIDs or opioids, can mess with your stomach. People mention nausea, indigestion, constipation, and sometimes ulcers or bleeding with more prolonged use of certain meds.
- Drowsiness or Fatigue: Some painkillers make people feel tired or foggy. This can affect driving, concentration, or just getting through the day.
- Dependency and Withdrawal: Opioids may lead to dependence if used regularly. Stopping suddenly can cause withdrawal symptoms like sweating, restlessness, or anxiety.
- Liver and Kidney Effects: Regular use of drugs like acetaminophen can tax your liver, while NSAIDs might stress your kidneys in the long run. Blood tests are often part of regular check-ups for people on these meds.
- Changes in Mood: Some people notice irritability, low mood, or even depression, especially with certain medicines or if pain itself wears them down emotionally.
- Sexual Health Issues: Meds like opioids can reduce libido or cause dysfunction. It’s not always talked about, but it’s a real effect for some people.
- Swelling and Weight Changes: Some drugs can cause swelling in the legs or rapid weight gain, which may indicate fluid retention.
Beyond those, some pain medications can also cause dry mouth, increased sensitivity to sunlight, ringing in the ears, or even affect balance. This can add more layers to manage, especially for older adults or anyone already juggling other health concerns. Adjusting when you take medication or switching to a different formulation sometimes tones down these less common problems, but always do this with medical guidance.
Challenges to Watch Out For
Long-term pain management isn’t always just about the physical side effects. People tell me about other hurdles too, like feeling disconnected from friends because it’s harder to socialize, struggling to keep up with work, or worrying about what others think.
- Tolerance: Over time, the body may become accustomed to a drug, so it may no longer work as well, and more may be needed for the same effect. This can be tricky, given both the pain relief and the side effects.
- Drug Interactions: When someone’s taking meds for other health issues, like blood pressure or diabetes, mixing pain treatments can cause extra headaches. Sometimes, one drug cancels out another or increases risks.
- Cost and Access: Medications, physical therapy, or alternative treatments can get pricey. Some insurance plans have restrictions that make it tough for folks to get what works best for them.
- Emotional Fatigue: Constantly dealing with both pain and medication management can leave someone emotionally drained. This may lead to anxiety, frustration, or even burnout, particularly if pain gets in the way of sleep. Finding healthy distractions and connecting with others who understand the struggle can help lighten the burden a bit.
Digestive Issues
Constipation stands out as the number one complaint for people on opioids. Over-the-counter remedies help sometimes, but others need prescription meds to keep things moving. With NSAIDs, stomach pain and heartburn are common, and anyone with a history of ulcers needs to be extra cautious. Doctors often suggest taking these with food or adding a stomach-protective medication if someone is at higher risk.
Drowsiness and Foggy Thinking
Opioids, and even some medicines meant for nerve pain (like gabapentin or amitriptyline), can make it tough for folks to think clearly or stay alert. People often learn to take their meds before bedtime, adjust their schedules, or mix things up if side effects interfere too much. Planning activities when you’re most alert, and asking about nonmedication options, can help you stay active and involved.
Emotion and Motivation Changes
Living with chronic pain is already stressful, but pain meds can sometimes make it harder to stay motivated or upbeat. For some, the emotional side of pain can be heavier than any physical symptom. Having a support network and talking through changes with a doctor or counselor makes a big difference. Therapies aimed at improving coping strategies, or even joining pain management support groups, have helped a lot of folks keep their spirits up even on tough days.
Tips for Managing Side Effects
If you’re dealing with pain long-term, it’s totally normal to feel frustrated by side effects. I always tell people there’s no shame in talking about what’s going on — lots of solutions exist, even if it takes a little trial and error.
- Stay in Touch with Your Doctor: Regular updates help your provider adjust your plan. Bring up new symptoms right away.
- Keep a Side Effect Log: Writing things down helps spot patterns that can point to what’s causing the trouble. Consider noting your activities, meal times, and moods along with medication use—you might notice trends that aren’t obvious at first.
- Ask About Dosage Adjustments: Sometimes a smaller dose or a different schedule can help reduce side effects like drowsiness or tummy upset.
- Mix in Non-Drug Strategies: Gentle stretching, mindfulness, physical therapy, or heat and cold packs work for many folks and reduce the need for higher doses of meds. Even light daily movement or creative hobbies can boost your well-being.
- Review All Medications: Check in with your pharmacist or doctor to be sure nothing is interacting poorly. Don’t forget to include nonprescription meds and supplements, as these can sometimes complicate your primary therapy.
Small lifestyle changes—like setting up a consistent sleep routine, staying hydrated, or eating more fiber—can make a big difference with some side effects too. It helps to celebrate little victories along the way, and to ask about community programs that offer pain management classes or peer support.
Open conversations make it easier to find a pain management plan that supports your life better, not just your symptoms. Building a relationship where you feel heard and respected by your care team makes treatment a little less challenging.
Living Life with Long-Term Pain Management
Pain that doesn’t go away tends to creep into every corner of life. People share stories about missing family events, skipping hobbies, or even stepping back from careers they once loved. Over time, most folks pick up tricks for balancing medication side effects with activities they care about. For some, that’s choosing lower doses and dealing with more discomfort to avoid heavy sedation or digestive issues. Others find their own blend by adding therapy, gentle exercise, better sleep habits, or social groups focused on healthy living with pain.
It’s worth remembering: the “right” plan looks different for everyone. For reliable information on medications and pain treatment, the Mayo Clinic (https://www.mayoclinic.org) and the CDC (https://www.cdc.gov/drugoverdose/patients/index.html) both share advice that aligns with what real-world patients experience. Ask your provider if there are local support groups or online communities where you can swap tips and encouragement, too. Staying curious and open to new approaches, such as occupational therapy or holistic pain management programs, can add value when things feel stuck.
- Setting Small Goals: Tackling one day at a time can make things feel less overwhelming. Tracking your achievements, no matter how small, helps maintain hope and motivation.
- Support Networks: Staying in touch with friends, family, or support groups can help with mental health and motivation. Even a quick phone call or online message can provide a boost on tough days.
- Exploring Alternatives: Tapping into yoga, meditation, or alternative therapies like acupuncture can give some people an extra tool in their toolkit. Your pain specialist or primary care provider may have resources or referrals to programs in your area.
Frequently Asked Questions
Q: Is it possible to avoid all side effects with long-term pain medications?
A: Avoiding every side effect can be tough, but working closely with your healthcare team can minimize the worst ones. Being proactive about reporting new symptoms helps a lot.
Q: What should I do if my medication suddenly stops working?
A: Losing the effect of your pain relief could be a sign of tolerance, a new health issue, or other changes. Always check with your doctor before changing how you take your meds.
Q: Are there any long-term risks of staying on pain meds for years?
A: Yes, especially with opioids and NSAIDs. These might affect your kidneys, liver, stomach, or mental clarity over time. Regular monitoring and open conversations with your provider are key.
Q: How do I talk to my family and friends about my pain management?
A: Being honest about your experience helps your support network better understand your needs. Even sharing a simple explanation of your treatment can open up meaningful conversations and reduce misunderstandings.
Final Thoughts
Managing pain for the long haul involves trade-offs, but with the proper support and a good team, it’s totally possible to live a whole, meaningful life. Everyone’s path will look a bit different, and tackling side effects is just part of the adventure. If you’re weighing your options, it pays to keep track of what does or doesn’t work—your real-life experience is the most valuable guide you have. Keep asking questions, keep reaching out for help, and remember you’re not alone.
Video: What Happens to Your Body on Long-Term Pain Medication 💊 #sideffects