Barriers stopping people from getting help for opioid addiction can make recovery feel out of reach. Laws, policies, and social attitudes all play a part, and even though science has come a long way, these challenges still impact real lives every day. I’ve checked out the different legal blocks that keep folks from the treatment they need, how they came together in the first place, and how things could work better for those trying to recover.
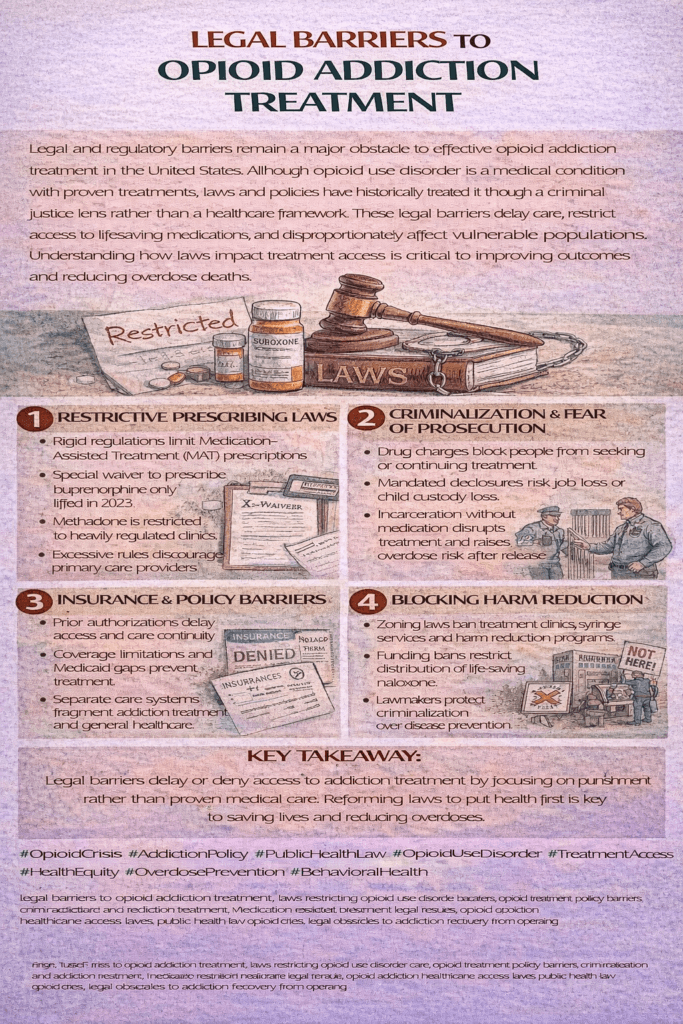
Common Legal Barriers Facing Opioid Addiction Treatment
Legal barriers matter because they shape who actually receives treatment, how easy it is to access treatment, and whether someone feels safe reaching out for help. These barriers come in a bunch of forms and show up at every stage, from making it hard for doctors to write prescriptions to creating tricky insurance hurdles that slow things down for patients.
Opioid addiction treatment isn’t about a single medicine or clinic. Effective plans usually include medications like methadone, buprenorphine, or naltrexone, plus therapy and support. Legal restrictions, though, have limited access to these proven options. Even as we learn more about what works, rules and regulations sometimes lag behind, and the results have a direct impact on real people’s lives.
Rules focused on punishing drug use instead of supporting recovery have also played a part. For years, the law treated drug addiction as a crime rather than a health problem. Some of these old attitudes linger in policies today, and this kind of approach can discourage folks from seeking help, even when treatment is available.
Understanding How Laws Limit Medication-Assisted Treatment
Medication-assisted treatment (often called MAT) is supported by extensive research. The catch is, legal restrictions often get in the way. Some common blocks include:
- Provider Certification: Some medications, especially buprenorphine, need special waivers or certifications for providers to prescribe them. Those rules make it harder for regular doctors to offer help, especially in rural or underserved areas.
- Dosing and Clinic Regulations: Medications like methadone are only available at licensed clinics. Patients usually need to show up in person every single day, at least in the beginning. That can be tough for people with jobs, childcare needs, or unreliable transportation.
- Prescription Limits: Some laws set strict limits on how much medication can be prescribed or for how long. Insurers and Medicaid plans might also impose additional restrictions, creating more red tape for patients and providers.
For instance, even after federal changes relaxed the buprenorphine waiver requirements, many communities still don’t have enough providers implementing these changes. When regulations or red tape stick around, people pay the price—sometimes with their health or even their lives.
How Insurance Rules Cause Extra Struggles
Even when the law doesn’t block treatment, insurance policies sometimes do. Licensed treatment providers share that getting prior authorizations or fighting step therapy requirements can eat up hours every week and slow down or stall patient care.
- Prior Authorization: Before someone can start medication, insurance plans might require approval, which isn’t always a fast process. Delays can lead to relapse or put people at risk.
- Step Therapy: Some insurers make patients try and “fail” on cheaper or older treatments before covering what doctors originally recommend, even if those alternatives are less effective.
- Covered Medications: Not every plan covers all forms of MAT, so patients sometimes face out-of-pocket expenses or have to switch medications, even if the medication they were taking was working well.
Navigating these insurance obstacles can be overwhelming for patients. Many clinics employ staff whose main job is to work with insurance companies to get patients the medications and therapy they need to stay on track. While some states have started passing laws to limit prior authorization for addiction treatments, change isn’t happening everywhere equally.
Stigma and Discrimination Backed by Law
It’s not just prescription policies that create hurdles. Zoning laws and local opposition can block new clinics from opening, especially those that offer methadone or needle exchange programs. Some neighborhoods push back on any plan to bring treatment services nearby, arguing it will hurt property values or increase crime. As a result, patients might have to travel for hours just to get their daily dose of a prescribed medication.
Former prisoners or people with certain criminal records also run into blocks. Some laws make it tough to get support when someone has past convictions, limiting their access to proven treatment once they’re out. This hits hard in communities already dealing with high overdose rates.
Examples of Discriminatory Legal Practices
- Prohibiting MAT in Recovery Housing: Some sober housing programs refuse to admit people using MAT, and state or local rules sometimes allow this.
- Parental Rights and MAT: In some states or counties, courts use participation in MAT as evidence against parents in custody cases, despite evidence-based guidance that MAT is effective and safe.
- Employment Discrimination: People who use MAT can face job discrimination, and sometimes there’s little they can do unless state law offers extra protection.
On top of that, stigma from healthcare providers or within communities can make individuals hesitant to reach out for help. Combating stigma will take ongoing education, advocacy, and changes in both law and practice.
Challenges in the Criminal Justice System
The intersection between drug laws and the penal system creates its own set of problems. Policies in jails and prisons often cut off access to MAT, even despite federal guidance laying out why continued treatment is important. For people inside, forced withdrawal can be painful and dangerous, increasing the risk of overdose after release.
- Jail and Prison Exclusions: Many lockups refuse to offer opioid addiction treatment, relying instead on “detox” through forced withdrawal.
- Lack of Referral After Release: Many correctional systems don’t establish referrals or connections to community-based care upon release. This break in care is a big reason why the weeks after release are so risky for fatal overdoses.
Recent lawsuits and federal court rulings have started to challenge these practices, and some facilities are making MAT available to inmates. There is still a long way to go, but progress is happening.
How Federal and State Laws Shape Access
Federal laws, like the Controlled Substances Act or the Drug Addiction Treatment Act, set up the framework, but states have a lot of say in what really happens. Some states have loosened restrictions, making it easier for providers to get certified or for patients to access MAT from their primary care doctor. Others have stuck to stricter rules, putting in place many checks that can slow everything down.
One example is how the federal government previously required a special “X waiver” for doctors to prescribe buprenorphine. While recent changes have dropped the waiver, the impact of years of restrictions still lingers, especially in places that don’t have enough willing or trained providers. States differ widely: in some, patients can get MAT at local clinics or even through telemedicine, while in others, choices are limited by local rules or tight reimbursement policies.
Best Practices and What’s Actually Working
In places where laws and rules have changed for the better, I’ve seen some pretty encouraging results. Making MAT easier to access through primary care, allowing pharmacies to dispense certain medications, or funding harm reduction programs all seem to help. A few simple moves have made big changes, like:
- Opening up telemedicine for MAT prescriptions, especially in rural areas (which became possible during the COVID-19 pandemic in many places)
- Eliminating prior authorization for MAT in state Medicaid programs
- Funding mobile clinics to reach people where they are
- Banning discrimination against people using MAT in housing and employment laws
Additionally, supporting programs that train more healthcare providers to recognize and treat opioid addiction can help fill gaps in access. States that have invested in public information campaigns to reduce stigma are seeing signs that more people are willing to start treatment and stick with it.
Common Questions About Legal Barriers and Opioid Addiction Treatment
I’ve put together answers to some frequent questions people have about why treatment access can feel so limited and what’s being done to fix it:
Why are there so many restrictions on opioid addiction treatment medications?
The rules come from a mix of concerns, including the risk of diversion (people selling meds instead of taking them), old laws built around the war on drugs, and worries about misuse. Many of these rules are being reevaluated as new research shows they can do more harm than good by keeping people from proven care.
How are insurance companies involved in creating barriers?
Insurance companies add delays and complications through requirements such as prior authorization, step therapy, and limits on covered medications. While these rules are meant to manage costs, they sometimes block access to timely, proven treatment.
What’s happening to improve access to treatment?
Changes like removing the buprenorphine waiver requirement, passing state laws to protect against MAT discrimination, and expanding telemedicine options have all helped. Advocacy groups and some medical associations are pushing for further improvements nationwide.
Key Takeaways for Patients, Advocates, and Families
When someone is ready for treatment, steering through these legal and insurance barriers is often the toughest part. Connecting with advocacy groups (such as the Legal Action Center or the Harm Reduction Coalition) and knowledgeable healthcare providers can make a difference. Staying up to date on changing rules in your state can help you or your loved one find the best options available.
- Speak up for better policies: Get involved with local or state reform efforts. Voices from people who have direct experience with treatment matter a lot to lawmakers.
- Document barriers: Keeping track of paperwork and communication with insurers or government agencies can help if you need to file an appeal.
- Reach out for legal help: Some organizations offer free or low-cost legal advice specifically for people facing discrimination in treatment, housing, or employment because of opioid addiction or MAT use.
Legal and policy issues can feel overwhelming when you just want care that works, but change is possible. A lot has happened in the past few years, and things are moving in the right direction as more people speak up and share their stories. Even with progress, knowing what’s in the way is the first step to overcoming it. That’s something I see getting better every day.
Video: Criminalization Stops People From Seeking Addiction Help #opioids #treatment