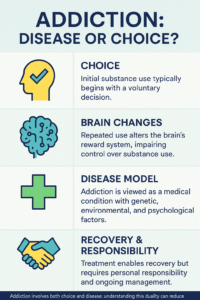
The question of whether addiction is a disease or a choice has fueled ongoing debate across science, medicine, and society. For decades, people have wrestled with how to define addiction—some viewing it as a moral failing or lack of willpower, others recognizing it as a complex brain disorder shaped by genetics, environment, and trauma. In my exploration of this topic, I’ve seen how much confusion and frustration this divide can cause, especially for those directly affected by addiction or supporting someone who is. Understanding addiction isn’t just an academic exercise—it’s the foundation for compassion, effective treatment, and lasting recovery. In this discussion, we’ll unpack the science behind addiction, the arguments on both sides, and what current research reveals about how much of it comes down to biology, behavior, and choice.
Understanding Addiction: What Does It Involve?
Addiction isn’t just about substances like alcohol, prescription pills, or illegal drugs. It also covers certain behaviors such as gambling. What links all these forms of addiction is a persistent urge or compulsion to engage in a substance or activity, even when it leads to adverse effects. People who struggle with addiction often feel trapped, with their need to use or participate overriding logic or personal intentions.
Addiction usually involves three main areas:
- Physical Dependence: The body adapts to a substance, and stopping it leads to withdrawal symptoms.
- Psychological Dependence: The mind needs the substance or activity to cope with stress or emotions.
- Compulsive Behavior: Individuals struggle to control their use, even when it leads to real problems at home, work, or in relationships.
It’s not as simple as deciding to smoke a cigarette or have a drink. Repeated patterns, changes in the brain, and environmental factors all play together, making addiction a very complex topic. Growing research has shown that things like early childhood trauma, ongoing stress, or peer pressure can set the stage for addiction before someone ever makes their first choice.
Addiction doesn’t discriminate. Anyone can be affected—regardless of age, career, background, or personal strength. For instance, a high-powered executive, a student, or a stay-at-home parent can each wind up struggling with substance misuse. The need to use or engage repeatedly is often driven by factors beyond what friends and family can see on the surface.
Is Addiction a Disease?
Many leading medical groups like the American Medical Association and the World Health Organization consider addiction a disease, specifically a chronic brain disorder. Over time, addiction actually changes how the brain’s reward and stress systems work. These changes can last for months or even years after someone stops using a substance.
When looking at addiction as a disease, here’s what stands out:
- Brain Chemistry Shifts: Substances like drugs or alcohol change dopamine levels, a neurotransmitter in pleasure and motivation. This makes seeking out the substance feel like a top priority to the brain.
- Genetic Factors: Studies show that genetics play a role in who may develop an addiction. Some families experience higher rates, which hints at inherited susceptibility.
- Long-term Progression: Addiction often develops over time, with repeated use making the brain and body more dependent.
Treating addiction as a disease can encourage healthcare providers and society in general to approach it with more empathy and support, rather than shame or judgment. This view removes much of the “blame game” and highlights the absolute need for medical treatment and counseling options.
If someone suffers from diabetes or high blood pressure, we don’t blame them for needing medication or support. Similarly, thinking of addiction as a medical condition helps make sure people get treatment instead of judgment. Plus, this approach encourages research into better therapies and long-term recovery tools.
Is Addiction a Choice?
Some people firmly believe that addiction is a result of personal choices; essentially, the outcome of bad decisions or poor willpower. In this view, not everyone who tries a substance gets addicted, which means there’s some choice involved.
Here are some points for the “choice” side:
- Initial Use: The first time someone smokes, drinks, or tries a drug is typically a personal decision. Nobody is born using substances—they choose to start.
- Self-control and Habits: People can control or resist certain behaviors early on.
- Recovery Stories: Many people recover from addiction by changing their behavior and taking responsibility for their actions.
However, it’s important to remember that the idea of choice gets smaller as dependency and brain changes set in. What might start as a decision can mix into something more challenging to control. Personal responsibility definitely plays a role in seeking help, but calling addiction only a choice tends to oversimplify it.
Stories of successful recovery are inspiring and show that change is possible. But it’s also true that relapses are common—not because someone is weak, but because the brain’s wiring has been transformed by long-term substance exposure. Talking openly about the weight of choice and compulsion helps reduce judgment and supports better outcomes.
What Science Says About Addiction
Neuroscience research really helps paint a clearer picture here. I’ve read studies using brain scans to show that addiction makes real, physical changes in the brain’s structure and function. For example, the brain’s reward center gets rewired to crave the substance, while the areas that control judgment and self-control are weakened.
Key findings from research:
- Changed Brain Pathways: The brain adapts to repeated drug or alcohol use, making cravings and compulsion much stronger than ordinary urges.
- Influence of Stress and Environment: Trauma, high stress, and unstable home lives can increase the risk of addiction; factors nobody chooses to have.
- Relapse Doesn’t Equal Failure: Cravings can return even after years, showing how lasting brain changes are. This is similar to other chronic diseases like diabetes, where symptoms can flare up if not managed carefully.
While addiction involves a set of decisions at the start, the ongoing cycle is driven by changes that create a powerful pull beyond simple willpower. Scientists are continuing to track down links between lifestyle, brain circuits, and addiction. This has led to breakthroughs in medication-assisted recovery and more effective approaches to therapy for people at all stages of the process.
Why the Debate Matters
How we view addiction—disease, choice, or a mix of both—directly impacts how people are treated in healthcare, at work, or even within families. If addiction is framed as a disease, people might be more supportive and open to treatment options. They’re less likely to judge and more likely to provide practical support, such as helping someone find a good rehab program or addiction specialist.
If addiction is seen strictly as a choice, stigma gets stronger. People experiencing addiction might be blamed or even punished instead of being offered help. This kind of response can stop someone from seeking support out of fear or shame.
There’s also a practical side: Health insurance coverage, public treatment funding, and even criminal justice policy depend heavily on how addiction is classified. Disease framing means more support for programs and coverage of recovery options.
The language we use matters, too. When the public and policymakers use understanding terms, it helps facilitate more compassionate solutions. Supporting education on what drives addiction can help families and communities offer better resources.
Common Misconceptions About Addiction
I’ve noticed several myths pop up repeatedly whenever addiction comes up in conversation:
- You Can Always Stop If You Want: The reality is that many people with addiction want to stop but can’t, at least not without support, medication, or therapy.
- Addiction Is a Sign of Weakness: This myth ignores the genetic risk factors and actual changes in the brain that come from addiction.
- Only Certain Types Get Addicted: Addiction doesn’t care about background, job, age, or economic status. It affects people from all walks of life.
Challenging these misconceptions leads to more helpful and fair support for everyone dealing with addiction. More awareness campaigns, open dialogue, and real-life stories make it easier for people to ask for help without facing much blame or embarrassment.
Thinking About Recovery and Treatment
Most recovery programs combine medical treatment, professional counseling, and community support. Medication can ease withdrawal and reduce cravings, while therapy helps untangle the causes behind addiction.
- Medications: Certain drugs can help normalize brain chemistry during recovery, making it easier for people to stay sober.
- Behavioral Therapy: Talking with a counselor helps people learn how to handle cravings, manage stress, and rebuild a healthy lifestyle.
- Support Networks: Groups like Alcoholics Anonymous or SMART Recovery connect people with others dealing with similar situations, which is pretty encouraging.
Recovery takes time, and there can be slips along the way; this isn’t a sign of failure. Ongoing support, practical tools, and a nonjudgmental attitude from family and friends help greatly. Some people discover new interests or strengths during recovery, boosting self-esteem and motivation.
Besides formal treatment, things like having a steady routine, setting small goals, and celebrating milestones go a long way in recovery. Involving loved ones, finding healthy activities, or learning new coping skills can strengthen the foundation for lifelong change. More workplaces and communities are now offering second-chance programs, which help remove some of the barriers that people in recovery face.
Frequently Asked Questions
I get a lot of questions when this topic comes up, so here are my answers to some of the most common ones:
Question: Can someone ever fully recover from addiction?
Answer: Many people live healthy, whole lives after addiction, but the risk of relapse can remain. Staying connected to treatment and support helps a lot with long-term recovery. Support systems and positivity make a big difference in continuing to build a new life free from substance misuse.
Question: Is there a “cure” for addiction?
Answer: There isn’t a fast or one-size-fits-all cure, but addiction can be managed successfully with the right mix of medication, therapy, lifestyle changes, and support. The process might look different for each person, but progress is always possible.
Question: Why do some people get addicted and others don’t?
Answer: Genetics, brain chemistry, childhood experiences, and the environment all play a part. No single factor tells the whole story. Even two people with similar backgrounds may react differently to the same substance or event due to genetics and unique stressors.
Final Thoughts
The disease or choice debate leaves out the fact that addiction is complex, involving both willpower and very real changes in the mind and body. Judging people with addiction doesn’t help. Understanding, empathy, and access to real treatment options do much more to support those trying to break free.
If you or someone close to you is struggling, reaching out to a healthcare provider or support group can put you on a better path. There’s no simple answer, but there are real ways forward.
Video: Is Addiction a CHOICE or a Disease