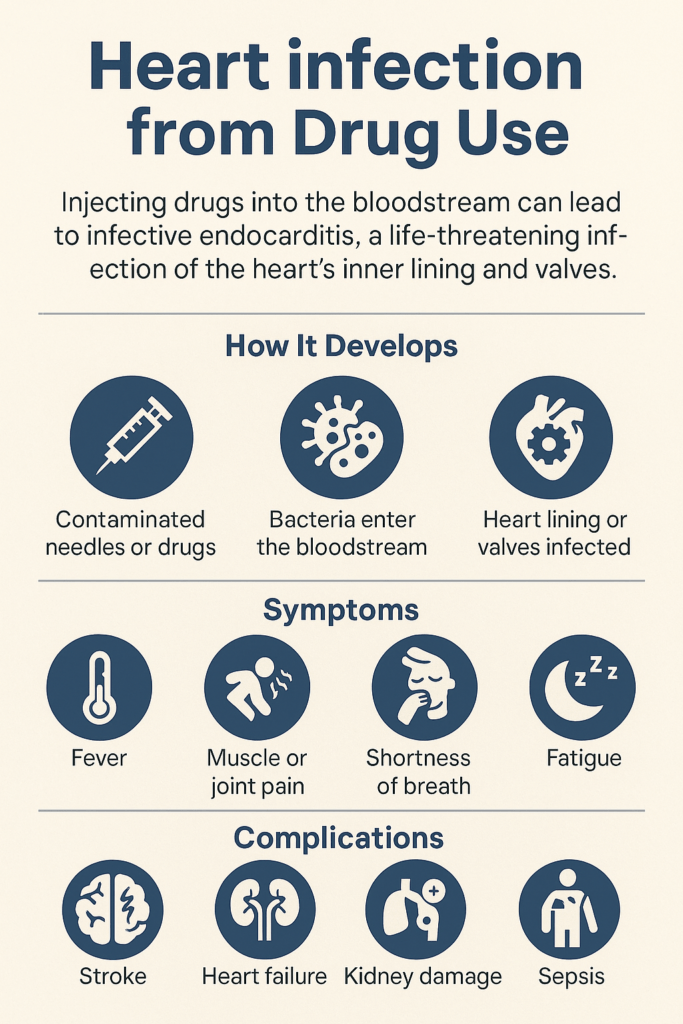
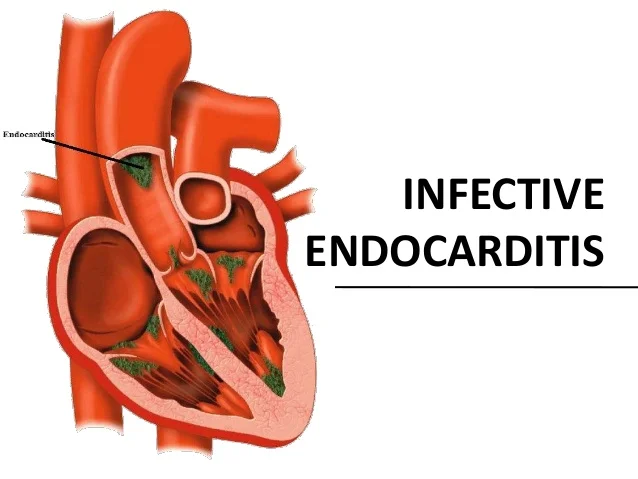
Infections of the heart caused by drug use often catch people by surprise, mainly because they’re not as widely discussed as other drug-related health risks. Yet for individuals who use injectable drugs—or who care for someone who does—these infections are a very real and serious concern. Conditions like infective endocarditis, where bacteria enter the bloodstream and attach to the heart’s inner lining or valves, can develop quickly and lead to life-threatening complications if not recognized and treated early. What makes these infections even more challenging is that their symptoms can be subtle at first, easily mistaken for something minor or unrelated. In this article, I break down what heart infections related to drug use actually are, how and why they develop, the warning signs to watch for, and what treatment typically involves. You’ll also find practical prevention tips and guidance on where to seek reliable help or more information—so you can better understand the risks and protect yourself or someone you care about.
How Drug Use Can Lead to Heart Infections
People often hear about infections tied to sharing needles or using unclean equipment for drug injection. This is where most heart infections linked to drug use start. Bacteria from contaminated needles or skin can travel directly into the bloodstream, and from there, the heart is dangerously close. When these bacteria reach the heart, they can latch onto the heart valves or inner lining; this is what doctors call infective endocarditis.
Other types of drug use (like snorting) don’t usually lead straight to heart infections, but drugs that affect the immune system, blood flow, or heart tissue can still increase the risk of other heart-related problems. Injecting drugs is by far the main pathway for bacteria to hitch a ride to your heart.
Some of the most common bacteria involved include Staphylococcus aureus (often called staph), streptococci, and occasionally fungi. These germs enter the bloodstream, sometimes multiple times a day if someone injects. It’s why having clean needles and preparation areas is super essential for harm reduction. Drug users may sprinkle or snort certain substances, but they rarely reach the level of direct bloodstream risk like injections do.
Understanding the Risks and Background
Heart infections like infective endocarditis have become more common over the past decade, especially as the opioid epidemic has increased the use of injection drugs. This condition doesn’t just show up in people with other heart problems; perfectly healthy hearts can be at risk if exposed to certain bacteria this way.
What’s wild is that heart infections from drugs don’t care about age, background, or general health status. I’ve seen younger people in their 20s and 30s affected, sometimes with no pre-existing medical problems. According to the CDC, drug-related infective endocarditis now accounts for almost a third of all endocarditis cases in some U.S. hospitals (CDC source), and the rates are rising pretty steadily in areas struck by the opioid crisis.
Prevention programs that offer clean syringe exchanges and easy access to addiction support services have been shown to drop these infection rates, so the link between harm reduction and healthier hearts is real. Unfortunately, the stigma surrounding drug use can still limit access to these vital services in some places, but continued advocacy is starting to help.
Signs and Symptoms to Watch For
Heart infections from drug use aren’t always apparent at first. They might feel like a bad flu at the start, but things get worse pretty quickly. Here’s what to keep on your radar if you or someone you know uses injection drugs:
- High fever and chills: These are among the earliest warning signs and sometimes the only ones at first.
- Tiredness and weakness: People often feel super wiped out, even with good rest.
- Shortness of breath: If infection affects the heart’s valve function, blood flow to the rest of the body drops.
- Chest pain: Not always there, but some notice chest pressure or pain.
- Night sweats: Waking up drenched or feeling weirdly sweaty without explanation.
- Unexplained weight loss: A little at first, but it can really add up.
- Swelling in hands, feet, or belly: This means the heart is struggling to pump blood properly.
Tiny red or purple spots on the skin, fingers, or eyes (called petechiae) can also appear as the infection worsens. Any combo of these is worth checking out with a healthcare professional, especially if injecting drugs is part of the picture. You should also watch for confusion, sudden fatigue, or worsening shortness of breath, since these can signal urgent complications.
Common Causes: Bacteria and Drug Use Habits
Dirty needles aren’t the only risk. Even if someone uses a clean needle, if the skin wasn’t cleaned with alcohol or the drug itself was prepped in a less-than-clean cup, bacteria can sneak in. Sharing cookers, filters, or water increases the risk of nasty germs reaching the bloodstream.
The most common drugs involved include heroin, fentanyl, methamphetamine, and even prescription opioid painkillers when injected. While any injected drug can carry this risk, longer-term injecting and sharing equipment raise it even higher.
Mixing drugs (like injecting speedballs, meaning heroin and cocaine together) can lead to even higher risks, as these often involve more frequent injections, higher rates of risky behavior, and faster breakdown of the immune system. Repeated use damages veins and soft tissues, too, making it even easier for bacteria to get in.
Other Health Factors That Play a Role
Specific underlying issues can make matters worse. Pre-existing heart valve problems, artificial heart valves, and weakened immune systems mean bacteria don’t have to work as hard to get established. For people living with HIV, diabetes, or those already on antibiotics, symptoms might be harder to spot up front.
Regular doctor visits can help catch early warning signs, especially for people with chronic health issues. Recognizing new symptoms quickly is one of the best ways to prevent serious outcomes.
How Doctors Diagnose and Treat Heart Infections
First up, diagnosis almost always starts with a blood culture to check for bacteria or fungi in the blood. Doctors will usually order an echocardiogram (an ultrasound of the heart) to look for clots or bacteria growing on the heart valves. Sometimes, additional tests such as CT scans or MRIs are used to determine whether the infection has spread to other organs.
If you catch a heart infection early, powerful antibiotics can sometimes clear it up before things get rough. But treatment usually means an extended hospital stay, often at least 4 to 6 weeks of IV antibiotics. If heart damage occurs, such as a damaged valve, surgery may be needed to repair or replace the affected area. Some hospitals are starting to pair infection care with addiction counseling from the very start, since treating both issues together gives better long-term results.
The hard truth is that treating heart infections linked to drug use is expensive, complicated, and challenging. It’s not just about getting rid of the infection. People often need help with withdrawal, ongoing substance use, or addiction support at the same time. Hospitals may coordinate with addiction specialists and community programs before someone goes home to limit the chances the infection comes back.
Complications That Happen with Heart Infections
Heart infections aren’t just uncomfortable; they can cause permanent heart damage or even be life-threatening. Some of the more serious problems include:
- Heart valve destruction: Bacteria can quickly eat through healthy heart valves, disrupting blood flow and making the heart work harder.
- Blood clots (emboli): Chunks of bacteria can break loose and travel to the brain, lungs, or other organs. This can lead to strokes, organ infections, or even death if not treated quickly.
- Heart failure: The strain on the heart may become too much, leading to swelling, fluid buildup, and a significant drop in energy and function.
- Persistent infections: If the same risky behaviors continue, repeated infections can really wear out heart tissue over time.
Why Quick Action Matters
Getting early treatment matters a lot here. The earlier a severe infection is caught, the less long-term damage, pain, and downtime someone is likely to face. Even if withdrawal is a worry, hospitals can help safely manage symptoms during treatment. Studies also show that patients treated quickly usually need less aggressive heart surgery and have a better chance of full recovery.
Tips for Reducing Risk and Staying Safe
Nobody’s perfect, and stopping all drug use can be tough, so practical steps really do help. Harm reduction programs, like clean needle exchanges, do more than hand out supplies; they also connect people to healthcare, support, and testing for other infections. These groups may offer HIV or hepatitis testing, provide wound care kits, or have nurses who can answer health questions confidentially.
- Use new, sterile needles every time if you inject drugs.
- Clean the skin with an alcohol pad before every injection.
- Never share cookers, filters, or water with others.
- Ask for supplies at local syringe service programs or pharmacies if possible.
- Stay up to date on regular health checks, especially if you notice a fever or weird skin changes.
- Reach out for support; harm reduction centers don’t judge, and their info can be super helpful even if you aren’t ready to quit entirely right now.
It’s also a good idea to let your doctor know if you’re using injection drugs so they can check for early signs of infection and give the proper care without stigma. Staying connected to trustworthy people and being honest with health providers can make for much safer outcomes.
Frequently Asked Questions
These are questions I hear a lot about heart infections and drug use:
How fast does a heart infection develop from injecting drugs?
Symptoms can appear in just a few days or creep up over a few weeks. Fever, chills, and weakness are the most common first clues, but early signs are sometimes easy to miss. Repeated injections speed up the process, and certain types of bacteria can worsen it more quickly.
Is it possible to recover fully after getting a heart infection from drug use?
Recovery is possible, especially with early treatment and changes in how drugs are used. If heart damage is severe, some folks need surgery. Working with doctors and addiction specialists together has been shown to improve outcomes and lower the risk of future infections.
Are only people who inject drugs at risk?
Injecting increases the risk the most, but rarely, taking other drugs that suppress the immune system or damage heart tissue (like certain potent stimulants or steroids) have also been linked to heart infections. The vast majority occur with injected substances, though. If you’re using any substance long-term and notice odd symptoms, it’s best to check in with a healthcare provider just in case.
Final Thoughts
Heart infections tied to drug use aren’t always talked about, but they’re essential for anyone who’s using or has loved ones at risk. Knowing the signs and understanding where the danger comes from can save lives. Harm reduction, regular health checkups, and strong support networks all work together to protect your heart, even when life or habits feel tough to manage. Remember, good information and the right tools go a long way toward lowering risk.
If you think you or someone close to you might have a heart infection, or you want more info about safer drug practices, local harm reduction groups, healthcare clinics, and trustworthy online pages like the National Harm Reduction Coalition are really good starting points. Paying attention now can mean a lot fewer tough days down the road. Don’t hesitate to get in touch with these resources—they’re there to help, no matter your current situation or goals.
Video: Bacterial Endocarditis From One Mistake #warning #health