Infection linked to drug use tends to fly under the radar, but it’s a risk that packs a punch. Many people focus on overdose and dependency, but infections tied to drug use cause serious complications and can even be deadly. When I got into the research behind these risks, I realized how much awareness can change outcomes for people who use drugs, whether that use is prescribed or not. Here, I’ll break down what infections from drug use involve, how they happen, why they’re often overlooked, and what can make a difference in preventing them.
How Drug Use Can Lead to Infections
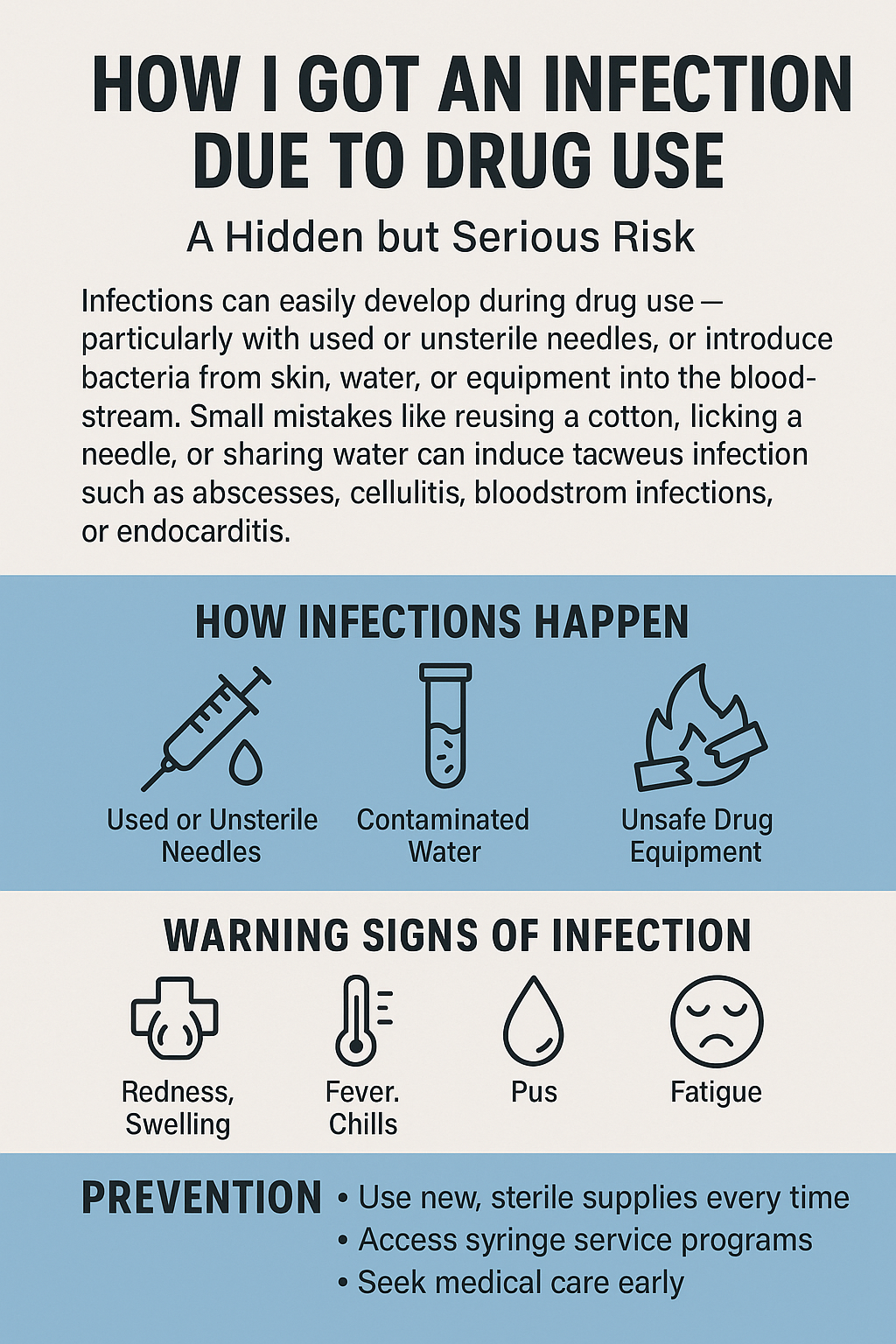
Using drugs isn’t just about what the substance does to your brain or body; it’s also about how people use them. Infections happen most often when drugs are injected, but even snorting or smoking can open doors to bacteria and viruses.
Drugs like heroin, methamphetamine, and even prescription painkillers used outside of medical supervision often get injected with shared, reused, or unclean needles. This creates a quick entryway for various pathogens into the bloodstream. But even non-injecting use, like smoking crack or snorting pills, can damage the lining of the nose, mouth, or lungs, allowing germs to settle in.
According to the Centers for Disease Control and Prevention (CDC), people who inject drugs are 22 times more likely to get HIV than those who do not. Other infections, like hepatitis C, skin abscesses, and even heart infections, are common as well (cdc.gov).
The Most Common Infections from Drug Use
Not all infections from drug use look the same. Some hit quickly and go away with treatment, while others linger for years or can be tough to get rid of. Here are some of the most common types I see mentioned in healthcare and health advocacy:
- HIV: Sharing needles is the most significant driver for HIV spread in drug-using communities. This infection attacks the immune system and can lead to AIDS if untreated.
- Hepatitis B and C: Hep B and C both spread through blood contact, especially with nonsterile needles or equipment. Hep C in particular is stubborn; many people with it don’t know until it’s seriously harming the liver.
- Skin and Soft Tissue Infections: These include abscesses, cellulitis, and ulcers. Redness, swelling, and pain are pretty much the signature symptoms. They often need both antibiotics and, sometimes, surgery to drain the pus.
- Endocarditis: This is an infection of the inner lining of the heart or its valves, primarily seen in people who inject drugs. Bacteria latch onto the heart, causing severe complications and sometimes requiring open-heart surgery or lifelong antibiotics.
- Lung Infections: Inhaled drugs damage lung tissue, upping the risk of pneumonia and fungal infections. Weak immune systems from drug use make these worse.
It’s important to note that some infections can also increase overall drug risks. For example, hepatitis C is a leading cause of liver failure and transplantation among people who inject drugs. Many of these conditions develop quietly, so people might not know there’s trouble brewing until they’re seriously ill. Ongoing research continues to expose more about how infectious complications from drug use develop and what trends are changing in different populations.
Why These Infections Often Get Overlooked
People are more likely to spot an overdose than a slowly developing infection. Several things contribute to these infections sneaking by unnoticed:
- Stigma: Many people who use drugs may avoid doctors out of fear of judgment or legal trouble. When infections do develop, they sometimes wait too long before getting help.
- Poor Access to Healthcare: People who are homeless or living in poverty are less likely to see a doctor regularly, which means minor issues turn into major ones.
- Overlapping Symptoms: Early symptoms such as fever, aches, or redness are easy to ignore or mistaken for withdrawal or other conditions.
- Compounded Health Issues: Many who use drugs already have weakened immune systems or other health problems. These complicate diagnosis and make infections harder to treat.
The subtle nature of some infections makes it challenging for both users and healthcare providers to catch them quickly. On top of that, self-treatment or relying on home remedies can delay professional care, which sometimes allows infections to spread or worsen before the person seeks help.
Quick Guide: Steps to Reduce Infection Risk in Drug Use
Reducing the risk of infection isn’t complicated, but it does require some planning and awareness. Here are real-world steps that make a difference for anyone using drugs:
- Use Clean Needles and Equipment: Always use sterile needles, syringes, and drug-prep equipment. Needle exchange programs provide these supplies and can also offer safe disposal options.
- Don’t Share Supplies: Sharing anything that comes into contact with blood, including cookers, cottons, and even rinse water, can spread germs.
- Practice Hygiene: Wash your hands before injecting. Clean the injection site with alcohol wipes. These small moves slash the risk of bacteria entering the skin.
- Regular Testing: Checking for HIV, hepatitis, and other common infections helps catch problems early. Many community clinics offer confidential or even free testing.
- Wound Care: Pay attention to redness, swelling, or drainage at injection sites. Get medical care for any signs of infection, even if they seem small at first.
These simple actions, supported by public health groups and many harm reduction programs, really change infection rates in communities. On top of that, seeking educational pamphlets or seminars from trusted sources can offer new tips on staying safer.
Barriers and Challenges to Staying Infection-Free
I’ve noticed that even people who know infection risks face curveballs that make prevention a challenge. Here are the most common hurdles:
- Access: Not everyone has a needle exchange program nearby, especially in rural areas. Some pharmacies limit syringe sales, making it harder to get clean gear.
- Legal Restrictions: In some places, carrying needles—even unused ones—can bring legal trouble, which pushes people toward unsafe reuse or sharing.
- Poverty and Homelessness: Without stable housing, it’s tough to keep things clean or visit a clinic. Food, shelter, and safety take priority over infection prevention for many.
- Stigma and Discrimination: When you feel judged by the doctor, you’re less likely to go back for a wound or fever. Some people push through infections until it’s too late to avoid the ER.
Additional challenges include language barriers, mental health struggles, or misinformation about what causes infections. Peer support groups can sometimes bridge these gaps, offering practical help and guidance in safe environments.
Common Myths About Infections and Drug Use
Lots of information gets mixed up when it comes to infection and drug use. Here are a few myths I keep hearing, and what’s actually true:
- “You only get infections if you inject drugs.”
Infections can pop up with any drug use, including snorting, smoking, or even prescription misuse. Any opening in the skin or lining of the nose gives bacteria and viruses a green light to move in. - “If the needle looks clean, it’s safe to use.”
Even if something looks clean, it can carry invisible germs. Only new, unopened equipment is truly sterile. - “If there’s no fever, it’s not an infection.”
Plenty of infections start with redness, a sore, or swelling, often without a fever. Keeping an eye on any changes at injection sites really matters.
Some also mistakenly believe that using alcohol or heat alone will sterilize reused supplies. While cleaning supplies are better than nothing, they are not foolproof, and pathogens can survive and be transmitted regardless of how “clean” something looks.
Frequently Asked Questions About Drug-Related Infections
Questions about infection risks and drugs pop up a lot. Here are some I hear most often, along with practical answers.
Question: Can prescription drug use also lead to infections?
Answer: Yes. Crushing and injecting prescription pills (like opioids or stimulants) exposes you to the same risks. Fillers and binders in the pills can make things even worse, clogging veins and raising infection odds.
Question: Are needle exchange programs legal in the US?
Answer: It varies by state. Many states allow them, but some limit what they can offer or where they can operate. Local harm reduction groups or health departments usually know what’s available in your area (cdc.gov).
Question: How can families or friends support someone at risk of infection?
Answer: Staying open, nonjudgmental, and learning about harm reduction makes a real difference. Help with finding clean supplies, medical care, or information on safer practices can go a long way.
Question: Are infections only a problem if you use drugs long-term?
Answer: No, infections can happen even after a single use, especially if shared equipment or unsafe practices are involved. Long-term use increases overall risk, but new users are not immune to these complications.
What Can Help Lower Infection Rates in Communities?
Addressing infection due to drug use isn’t only a personal issue. It shapes entire neighborhoods and cities. There’s good evidence that public health moves make a difference:
- Expanding Needle Exchanges and Safe Consumption Spaces: These programs have been shown to lower infection rates by providing clean equipment and a judgment-free place for safe use.
- Education and Outreach: When accurate info about infection risk is shared, especially by peers or trusted members of the community, more people use safer practices.
- Supportive Healthcare: Health providers trained in harm reduction tend to spot and treat infections sooner, with less stigma. This builds trust and better outcomes.
- Law and Policy Changes: Making clean supplies more available, decriminalizing possession, or allowing supervised sites helps people stay healthier and lowers emergency room visits in the long run.
Increasing awareness and giving people tools to protect themselves works. Some communities have slashed rates of HIV and hepatitis by more than half after expanding needle programs and supportive care options (harmreductionjournal.com).
Programs that provide support for mental health, stable housing, and addiction treatment can also help reduce infection rates. By meeting people where they are, rather than expecting rapid change or abstinence, more folks get the help they need early—before complications take over.
Taking Infection Risk Seriously, One Step at a Time
Infection due to drug use is one of those hidden dangers that can have significant consequences. Being open and practical about the risks, without shame or fear, leads to better decisions and healthier communities. Small changes, like using new supplies and taking early signs of infection seriously, really do prevent suffering and save lives.
Support systems, clearer information, and caring healthcare matter more than judgment. If this topic hits close to home for you or someone you care about, plenty of resources are available to help take steps toward safer use and better health. Don’t hesitate to check in with local clinics, harm reduction groups, or online support communities for up-to-date advice and practical tools.
Video: 5 Things You Don’t Know About Infection Risks in Drug Use