Seizures caused by drug use can be alarming, unpredictable, and incredibly confusing for anyone who experiences or witnesses them. When they happen, people often wonder what’s going on in the brain, why certain substances can provoke such a severe reaction, and which drugs carry the highest risk. Understanding this connection is important because seizures aren’t just a temporary scare—they can signal serious changes in brain activity. They may lead to long-term complications if the underlying cause isn’t addressed. I created this guide to break down the science in a clear, approachable way and to share insights that make the topic easier to understand. By exploring how drugs trigger seizures, what substances are most commonly involved, and the warning signs to watch for, you’ll have a better grasp of the risks and how to respond safely.
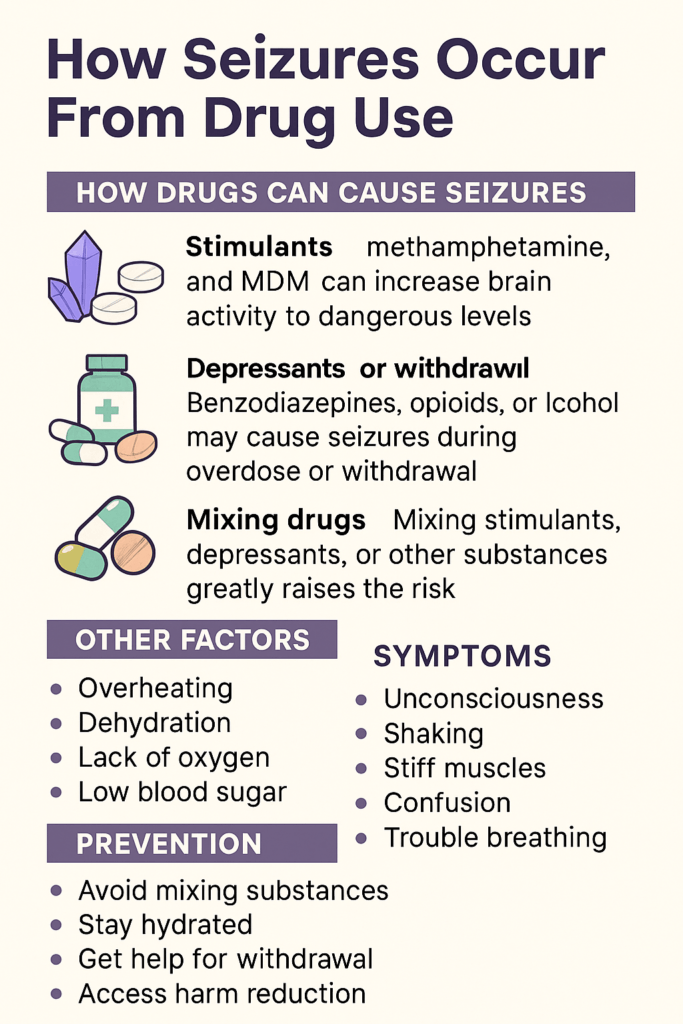
What Causes Seizures From Drug Use?
Drug-induced seizures can happen when substances disrupt the brain’s electrical signals. Usually, those signals are finely timed and controlled. But drugs, whether prescribed, over the counter, or illegal, can mess with the balance of chemicals (neurotransmitters) that guide those signals. When this happens, brain cells can start firing unpredictably and all at once. That sparks a seizure.
Certain drugs make the brain extra sensitive to seizures. Stimulants like cocaine, methamphetamine, and even high doses of caffeine can overstimulate nerve cells. On the other hand, depressants or sedatives (such as benzodiazepines or alcohol) can put the brakes on the brain’s activity. If they’re stopped suddenly after heavy or long-term use, the nervous system goes into hyperdrive, increasing the risk of seizures.
How Drugs Disrupt Brain Chemistry
The brain relies on a careful balance between ‘exciting’ chemicals (such as glutamate) and ‘calming’ chemicals (like GABA). Many drugs mess with this balance by either flooding the brain with neurotransmitters or blocking their regular action. Here’s how a few common categories can lead to seizures:
- Stimulants: Drugs such as cocaine, amphetamines, ecstasy, and bath salts push the brain into a hyperactive state. Overdose or repeated use can overwhelm nerve cells and tip the balance toward uncontrolled firing, raising the chances of a seizure.
- Depressants and Sedatives: Benzodiazepines and barbiturates calm the brain, but abruptly stopping them (or alcohol after extended heavy use) can lead to rebound overactivity, which is a common cause of withdrawal seizures.
- Opioids: While opioids (like heroin, fentanyl, or oxycodone) are usually known for slowing breathing, they can also trigger seizures, especially in overdose situations or when mixed with other drugs.
- Hallucinogens: Drugs like LSD or PCP rarely directly cause seizures, but they can increase the risk if taken alongside stimulants or by people with underlying neurological problems.
- Certain Prescription Drugs: Some medications used to treat depression, anxiety, or even allergies (like bupropion or diphenhydramine) have been linked to seizures, especially at high doses or if combined with other substances.
Long-term or repeated exposure to these drugs not only raises seizure risk but can also make the brain more vulnerable to other triggers, like stress and illness. It’s important to realize that the effects on brain chemistry can last even after stopping the drug, especially in people with other health problems.
Common Signs and Symptoms of Drug-Induced Seizures
Seizures from drug use often look just like seizures from any other cause. People may suddenly lose consciousness, have shaking movements of the arms and legs, stare blankly, become rigid, or experience odd sensations or confusion. Here are a few things I’ve noticed from first-hand experiences and stories I’ve heard:
- Convulsions (Jerking movements): The most recognized symptom.
- Loss of awareness: Some people blank out or stop responding for a short time.
- Muscle stiffness: The body may go rigid before the jerking starts.
- Odd tastes, smells, or sensations: Some seizures begin with strange sensory experiences.
- Sudden confusion or fear: Especially in so-called “focal” seizures.
After a drug-induced seizure, people are usually confused, exhausted, or sore. This recovery period is sometimes called the “postictal state.” Family and friends might feel anxious or helpless during this time, so knowing what to expect can help everyone involved.
Drugs That Most Commonly Cause Seizures
While almost any substance has the potential to trigger a seizure if abused, some stand out as being higher risk. I’m sharing a quick rundown based on research and things I’ve learned over the years:
- Cocaine and Crack Cocaine: Known for causing seizures even in small doses for some users, especially when taken in a binge or mixed with alcohol.
- Amphetamines (Crystal Meth, Adderall): Big doses or rapid use can bring on seizures, especially if combined with dehydration or lack of sleep.
- Alcohol: Seizures are unlikely while drinking, but two situations increase the risk: alcohol withdrawal (especially after days of heavy drinking) and binge drinking episodes.
- Benzodiazepines (Valium, Xanax): The danger surfaces mainly with sudden withdrawal after prolonged or high-dose use.
- Tramadol and some antidepressants (like bupropion): These can cause seizures even at recommended doses, but especially when mixed with other meds or alcohol.
- Novel Psychoactive Substances (NPS): “Designer drugs” (like synthetic cannabinoids or cathinones) can be unpredictable and often come with a risk of seizures.
Certain over-the-counter medications, when misused, also land on this list. Even seemingly harmless drugs, if taken in very high quantities or mixed with other medicines, can be risky.
Why Some People Are More Prone to Drug-Induced Seizures
Not everyone who uses these drugs will have a seizure. Some people have a genetic tendency that makes their brains less tolerant to disruption. Medical conditions, like epilepsy, brain injuries, or infections, also raise seizure risk. Sleep deprivation, dehydration, and mixing multiple substances (especially mixing uppers and downers) make things even riskier.
I’ve heard from a few people who had their first seizure after a night of sleep deprivation, lots of caffeine, and a smaller amount of stimulant drugs than usual. It just goes to show that even low doses combined with certain factors can be dangerous. Age and existing health problems can matter too, making some folks more vulnerable than others.
Reducing the Risk: Simple Safety Steps
While the best bet for avoiding drug-induced seizures is not using high-risk substances, there are some practical steps for harm reduction. If you or someone you know uses substances (medically or otherwise), it’s essential to keep these tips in mind:
- Don’t suddenly stop sedatives or alcohol: If you’re planning to quit, talk to a doctor about a slow taper; it really lowers withdrawal seizure risk.
- Avoid mixing substances: Combining drugs, especially with alcohol, increases the dangers.
- Stay hydrated and rested: Dehydration and sleep loss make seizures more likely, especially with stimulants.
- Stick to prescribed doses: Some prescription meds (like bupropion or tramadol) carry seizure risk even in people without a history; take them as directed and talk to your doctor before combining anything new.
Remember, harm reduction isn’t about encouraging use; it’s about keeping people safer. In a harm reduction approach, it’s also essential to have a support system and know when to seek emergency help (for example, if a seizure lasts more than five minutes or if the person doesn’t regain consciousness).
Common Challenges With Drug-Induced Seizures
- Unpredictable reactions: New or unfamiliar substances can cause unexpected seizures, even when used infrequently.
- Legal risks: Some people hesitate to get emergency help after a drug-induced seizure because they’re worried about legal trouble. But medical safety always comes first.
- Stigma and mental health: After experiencing a seizure, it’s normal to feel anxious or embarrassed, especially if it happened during substance use with others. Finding support can really help with recovery.
Support groups, counseling, and honest conversations with medical professionals can help tackle these challenges. Educating friends and family about the risks and signs of seizures goes a long way toward preventing harm and encouraging an open dialogue about recovery.
Managing Withdrawal Risks
Withdrawal from sedatives and alcohol is one of the leading causes of seizures among people with a substance use history. Withdrawal seizures can develop several hours to a few days after stopping use. Medical detox programs are helpful because they provide supervision, prevent complications, and can use medications to reduce seizure risk. If you or a loved one wants to quit, connecting to professional addiction or medical services is a smart move.
Health and Lifestyle Factors
Staying healthy overall reduces risk. Getting enough sleep, eating regular meals, drinking enough water, and managing existing health conditions all help keep the brain steady, even if you’re exposed to a seizure risk from drugs or medications. Physical activity, stress management, and routine health checkups can give you an added layer of protection against many seizure triggers.
Drug Use, Seizures, and Long-Term Health
One seizure triggered by drug use doesn’t always mean someone will develop epilepsy. But repeated seizures, or brain injuries related to overdose or falls during seizures, can raise long-term risks. I’ve seen people recover completely after a single drug-related seizure with no long-term effect, while others faced ongoing health challenges or needed continued care. That’s why getting a thorough checkup after any seizure is essential, even if you feel okay right afterward.
- Memory issues: Some people notice lasting memory or concentration problems after repeated seizures.
- Mood and mental health: Anxiety, depression, or embarrassment sometimes follow a seizure event—connecting with mental health resources is helpful.
Suppose you’re worried about potential future risks. In that case, keeping detailed notes on any episodes, medications, and triggers will help your doctor identify patterns and recommend the safest course of action for your long-term wellness.
Frequently Asked Questions
Question: Can any drug cause a seizure, or are only some risky?
Answer: Almost any drug, at high enough doses or if combined with other factors like dehydration or poor sleep, can raise seizure risk. Some drugs are riskier than others (like stimulants and abrupt withdrawal from depressants), but individual reactions can vary.
Question: Are seizures from drug use life-threatening?
Answer: Most single seizures stop on their own, but prolonged seizures, repeated seizures without regaining consciousness, or seizures that happen in risky situations (like swimming or driving) can be dangerous. Emergency help is needed for seizures lasting longer than five minutes or for breathing problems.
Question: What should I do if someone has a seizure after using drugs?
Answer: Keep them safe by moving objects out of the way, gently turning them onto their side if possible, and not putting anything in their mouth. Call for emergency help right away if the seizure lasts longer than a few minutes, or if it’s their first seizure.
Wrapping Up: Main Takeaways
Understanding how seizures happen from drug use can help people make safer choices, look out for warning signs, and know when to get help. The best way to avoid a seizure is to steer clear of substances that put your brain’s natural rhythms at risk, but watching out for withdrawal and mixing of drugs is just as important. If you’re worried about seizure risks, it’s always smart to talk to a doctor or addiction expert, ask questions, and keep yourself or friends safe if something feels off. Staying informed means you’ll be ready to make better choices for your health and peace of mind.
Video: How Seizures Occur From Drug Use