HIV transmission can seem like a distant issue if it hasn’t touched you or your community directly. Still, the way it spreads from drug use to the broader population is a public health topic that actually affects many people. The process isn’t always as straightforward as people think. Understanding the steps involved can help with awareness, prevention, and support efforts. Here, I’ll lay out how HIV passes from people injecting drugs into the general population and what that really means for public health.
The Link Between Injection Drug Use and HIV Spread
The relationship between drug use and HIV is bigger than just sharing needles. While sharing syringes is definitely risky, more factors at play push HIV from high-risk groups into the community.
People who inject drugs (often called PWID in research) can transmit HIV through several routes. Besides direct needle-sharing, there’s also risk tied to sexual activity, sharing drug-preparation equipment, and having partners or close contacts outside their immediate drug-using network. Once HIV takes hold in these smaller groups, it’s easier for the virus to enter new circles.
Numbers show why these matters: according to the CDC, people who inject drugs account for about 10% of new HIV diagnoses in the United States each year. Globally, the stats can look even higher in places with less access to clean needles or prevention programs (source).
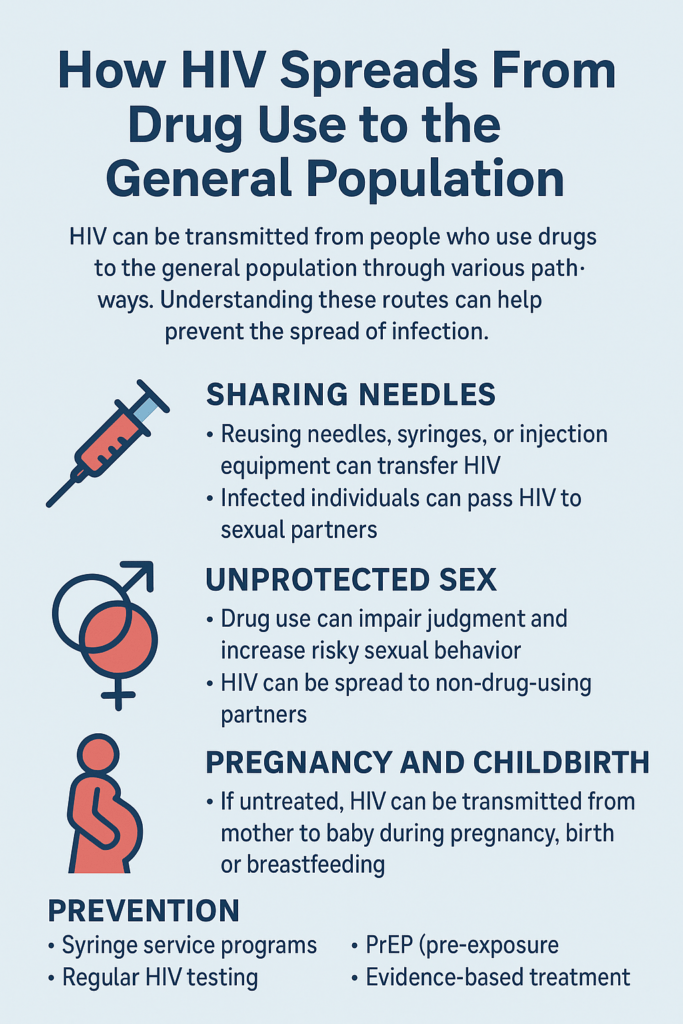
How HIV Moves from Drug Use to the Larger Community
HIV doesn’t just stay confined to people who inject drugs. Here’s how it works its way into the general population:
- Needle Sharing: The most direct route. If someone who is HIV positive shares a syringe with someone else, the virus can move quickly.
- Sexual Transmission: Drug use, especially with certain substances, lowers inhibitions and can lead to risky sexual behavior, like having unprotected sex. If a person who injects drugs has sex with a partner outside their network, the virus can move to new people easily.
- Bridge Populations: Sometimes, people who use drugs have partners or spouses who do not use drugs. These “bridge” partners become one of the fastest ways HIV steps into the general public.
- Mother to Child Transmission: If a woman who uses drugs contracts HIV and then gets pregnant, the virus can pass to the baby during pregnancy, birth, or breastfeeding unless preventative steps are taken.
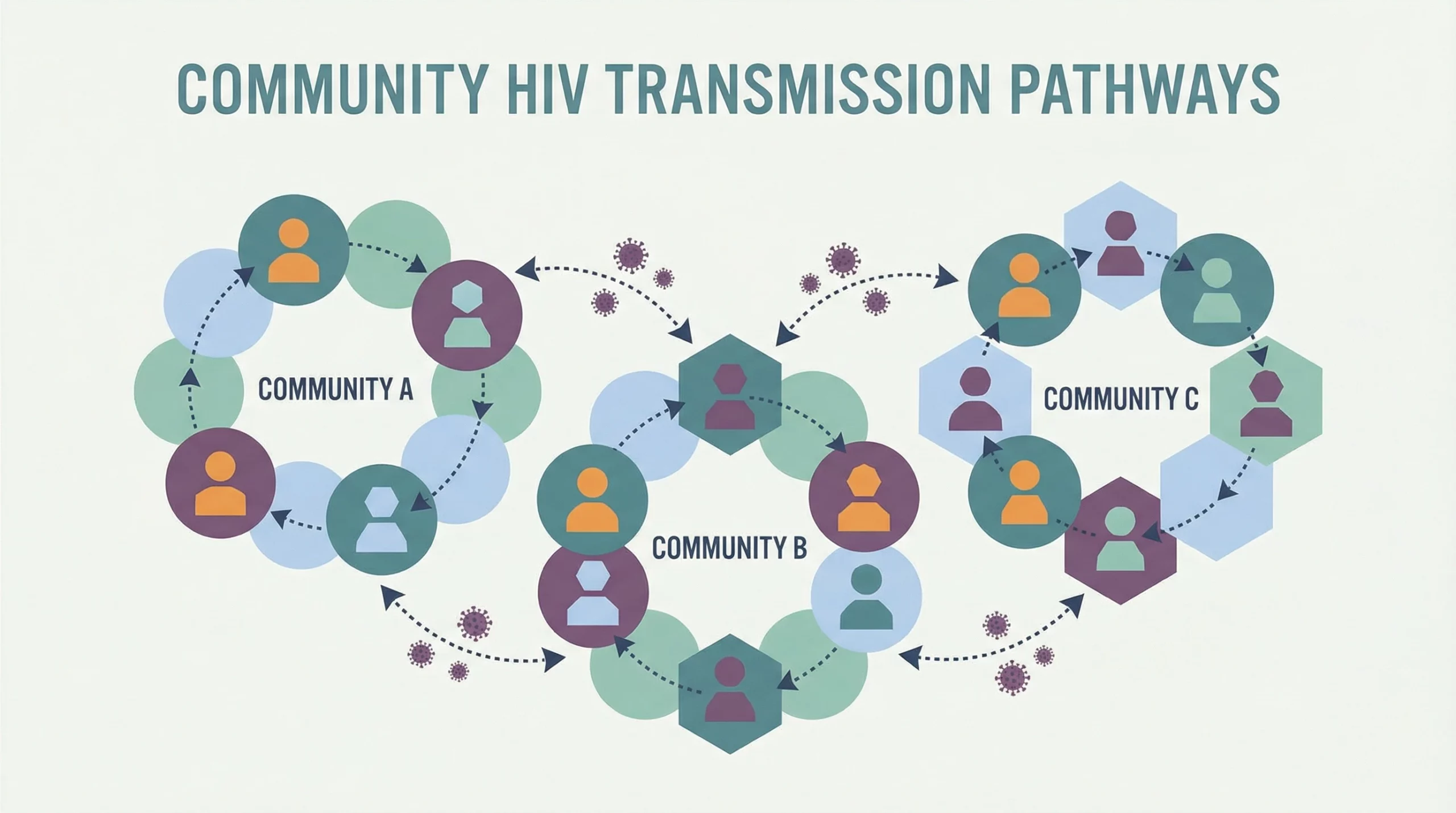
In many communities, this web keeps expanding. Once HIV shows up in new groups, it can be passed between people who have never used drugs, creating fresh challenges for prevention and outreach. The ripple effect demonstrates why holistic public health approaches—including education, community resources, and access to care—are so critical.
What Makes Drug Use a High-risk Factor For HIV?
Some factors make people who use drugs really vulnerable to contracting and spreading HIV. Here’s why:
- Frequent Needle Use: The act of injecting drugs means there are more opportunities for exposure to infected blood.
- Lack of Access to Clean Needles: In areas where needle exchange programs aren’t available, people end up sharing and reusing needles much more, increasing the risk.
- Social Margins: People who inject drugs often face housing problems, stigma, poverty, or a mix of all three, making it harder to get health care, information, or support.
- Mixing Drug Use and Sex Work: Some turn to sex work to support their drug use, adding another layer of HIV risk and yet another way the virus can spread to wider circles.
These factors make infections that start within drug-using communities tough to contain without public health strategies. It’s not just about risky decisions—often it’s about a lack of resources, support systems, and education. Lifting those at the most significant risk can, in turn, boost community health as a whole.
Prevention and Harm Reduction Strategies
There’s a lot of talk about “harm reduction” for a reason; it works. These approaches meet people where they are, offering safer options if someone can’t or won’t entirely stop injecting drugs. Practical prevention steps include:
- Needle and Syringe Exchange Programs: These organizations give out clean needles and take back used ones, helping prevent needle-sharing.
- Opioid Substitution Therapy: Medications like methadone or buprenorphine help reduce the need for risky injection practices.
- HIV Testing and Counseling: Regular testing can help people know their status so they can protect themselves and others.
- Condom Distribution: Making condoms easy to get, especially where drug use and sexual risk overlap, puts a dent in sexual HIV transmission.
- Education: Outreach that explains how HIV spreads, how to use equipment safely, and what support is available can go a long way.
Countries with strong harm reduction programs see much lower rates of HIV spread from drug use. Resources like the CDC’s Syringe Services Program info can give more background. Supportive medical care, mental health services, and housing aid also help those at risk avoid the spiral of unsafe drug use, homelessness, and untreated sickness. A well-rounded support system truly makes a difference.
Common Challenges in Stopping HIV Spread
Despite all the prevention options, several barriers get in the way:
- Stigma and Discrimination: Feeling judged or punished keeps some people from seeking care, testing, or harm reduction supplies.
- Legal Barriers: Needle exchange programs are not available in all regions and, in some cases, are even illegal, which complicates outreach.
- Lack of Funding: Many programs operate on tight budgets, limiting the number of clean pieces of equipment and the education they can provide.
- Complex Lives: Many people struggling with addiction have issues like unstable housing or mental health needs, making it harder for them to focus on prevention. The daily challenge of survival can overshadow even the most critical health choices.
Getting more support for harm reduction, ending stigma, and making testing and prevention truly accessible are critical steps in controlling HIV’s spread from drug use to the broader community. Collaborations between health services, law enforcement, and social programs can help smooth the way for more effective solutions. Raising awareness and speaking up for sensible policy can help communities move forward.
Practical Example: The “Bridge Person”
Picture this: A person who uses injection drugs is in a relationship with someone who does not use drugs. If the first person becomes HIV positive and has unprotected sex with their partner, HIV can now enter the partner’s social and sexual networks. It’s details like these that turn individual risk into a genuine community issue. Once the virus gets into broader social groups, tracking and controlling its spread becomes much more complicated.
How the Virus Moves Beyond Drug Users
Once HIV enters the general community, it doesn’t always come from needle sharing. In many cases, sexual transmission among people who never use drugs is actually one of the biggest drivers for further spread. That’s why HIV testing, education, and open conversations matter for everyone, not just people in high-risk groups. A commitment to openness, compassion, and learning can help break cycles of misunderstanding and fear.
Frequently Asked Questions
How can HIV prevention in drug-using communities help public health overall?
Prevention steps like syringe exchange, testing, and education make it much harder for HIV to hitch a ride into wider social circles. Fewer infections in high-risk groups lead to fewer infections everywhere. In this way, efforts focused on drug-using communities have an outsized positive effect on overall public health.
Is it possible to get HIV from being near someone who uses drugs?
HIV can’t spread through casual contact, such as hugging, sharing food, or spending time in the same space. The virus is only transmitted through blood and sexual fluids, and (much less often) from mothers to infants. Every day interactions with someone who uses drugs are not a risk for HIV.
What is “harm reduction” and why do experts support it?
Harm reduction provides people with tools and knowledge, like clean needles, safe spaces, and nonjudgmental support, to reduce their risk of infection when they inject drugs. It’s recognized by most health experts, including the World Health Organization, as a practical way to slow HIV. Approaching drug use with support and information, rather than punishment, helps keep communities healthy and safe.
What I Take Away from the Big Picture
HIV’s adventure from a needle in one person’s arm to a larger community isn’t random or mysterious. There are clear, well-known paths, and with innovative strategies, the risks can be limited. Knowing the main drivers of this transition helps communities, families, and health systems step in with prevention, testing, and care before problems grow out of control.
Harm reduction makes a real difference. Practical programs, such as clean needle distribution, medication-assisted therapy, and robust HIV testing, make communities healthier and reduce the risk for everyone—not just those who use drugs. More information is always a good thing, so I’m a strong supporter of open, judgment-free conversations about these topics. Supporting harm reduction and public health efforts benefits everyone, especially when backed by compassion and reliable information. Making these tools and conversations part of everyday life can slow HIV’s spread, level up safety, and build healthier communities for everyone.
Video: From injection sites to families HIV’s real risk #transmission #health #facts