Hepatitis is a group of diseases that mess with the liver, and drug use is sadly one of the fastest ways these viruses can spread. If you’re curious about how hepatitis actually gets passed on among people who use drugs, you’re not alone. Many folks assume it’s only about sharing needles, but there are actually a few ways these viruses can move from one person to another. I want to give you a clear, real-world overview of the risks, how infection happens, and what people can do to protect themselves.
Understanding Hepatitis: A Quick Overview
Hepatitis refers to inflammation of the liver, usually caused by a virus. The three most common types connected to drug use are hepatitis A, hepatitis B, and hepatitis C. Hepatitis C is ubiquitous in people who inject drugs, but hepatitis B is also a risk. Each type causes its own set of problems and spreads in a slightly different way. What they all have in common is the way they affect the liver and how easily they move in certain situations.
Hepatitis B and C can both become chronic, lingering in the body for years and quietly damaging the liver. Hepatitis A is less likely to hang around, but can still cause nasty symptoms and sometimes, more serious issues. Knowing the differences between these viruses helps a lot when talking about risks around drug use. Notably, hepatitis B can be prevented with vaccination, which is a key public health tool in minimizing the risks for those who use drugs. On the other hand, hepatitis C does not have a vaccine, making risk reduction even more critical for this group.
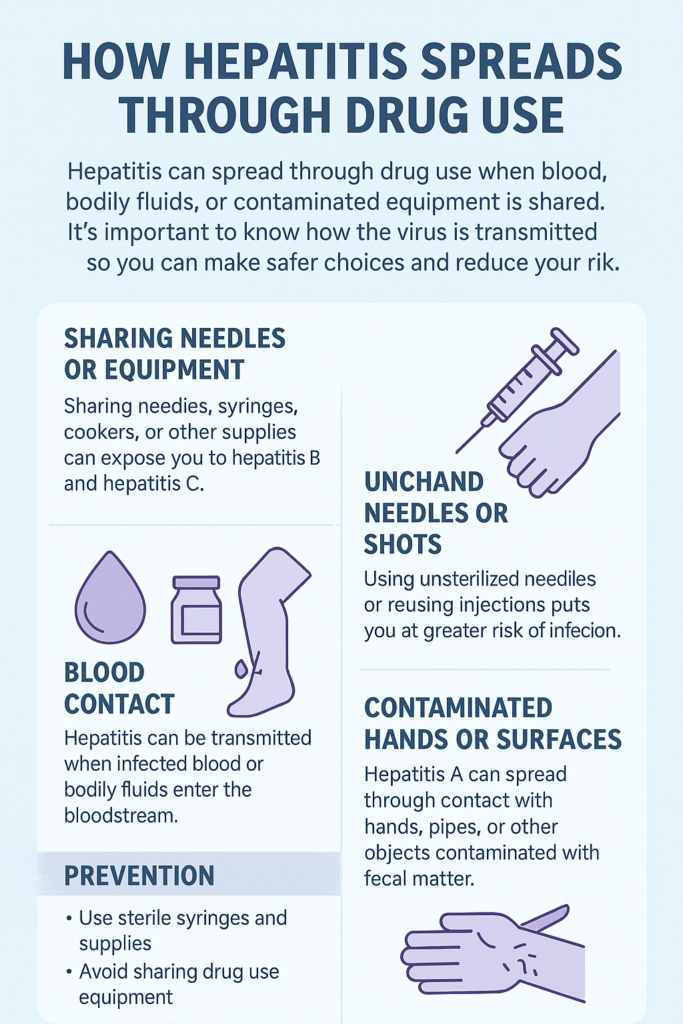
How Hepatitis Viruses Spread Through Drug Use
The main way hepatitis moves from person to person in the context of drug use is through contact with infected blood. Here’s how it often happens:
- Sharing Needles and Syringes: When someone with hepatitis uses a needle, tiny amounts of their blood can stay on or in the needle. If another person uses that same needle, the virus can enter their body, too.
- Reusing or Sharing Drug Preparation Equipment: It’s not just the needles that matter. Items such as cookers, cotton, water, and even tourniquets can become contaminated. These little pieces of equipment are often overlooked, but they’re a top way for hepatitis B and C to spread.
- Sharing Straws or Tubes for Snorting Drugs: Hepatitis C can also move between people through shared straws or tubes for inhaling drugs. Tiny damage in the nose or mouth can let the virus slip in, especially if someone using the same straw is infected.
These risks don’t only apply to people who inject drugs. While injection is the highest-risk activity, people who snort or smoke drugs can also be exposed to blood or to surfaces with blood droplets. Hepatitis B has another route, too: it moves through bodily fluids like semen or saliva, but blood is still the primary concern with recreational drug use. Surfaces where drug equipment is handled may not always appear contaminated. Still, invisible droplets can pose real dangers to anyone who comes into contact with them and has open cuts or sores.
Key Factors That Increase the Risk
Some situations make the risk of getting or spreading hepatitis even higher among drug users:
- Limited Access to Clean Supplies: Not being able to find new, affordable supplies like needles or cookers easily leads people to reuse or share.
- High Frequency of Use: People who inject drugs multiple times a day have more opportunities to be exposed to the virus.
- Using in Groups or Social Settings: Drug use isn’t always a solo activity. Groups often share tools, sometimes without realizing the risks or simply due to habit.
- Lack of Information: Not everyone knows all the ways hepatitis can spread. Sometimes, it’s just not clear that even things like water and little bits of cotton can carry the virus.
When these factors pile up, entire communities can see a significant spike in hepatitis infections related to drug use. Much of the transmission happens because of a mix of personal choices, the availability of resources, and the harsh realities of addiction. Add to that the fact that drug use often coincides with unstable housing or limited health care, and it’s easy to see why rates can be so high in specific environments. People facing stigma or discrimination are less likely to seek out support or education, which can also cause risks to skyrocket.
What Makes Hepatitis C So Widespread Among People Who Use Drugs?
Of all the hepatitis viruses, hepatitis C is the one most tightly linked to injection drug use. Research shows that well over half of people who inject drugs long term wind up with hepatitis C, and this virus is responsible for most new infections in this group.
Hepatitis C is really good at getting from one person to another through blood-to-blood contact. Even a tiny, invisible drop of blood can carry enough virus to infect someone. The virus also survives outside the body for hours or even days, turning used equipment into a real hazard. This explains why outbreaks can happen so quickly in communities where sharing is common and supplies are limited. On top of that, hepatitis C is often silent in the early stages, so people might not even know they have it and can pass it along without realizing it.
Simple Steps That Help Lower the Risk
Some practical things can make drug use a lot safer when it comes to hepatitis:
- Always Use New, Sterile Needles and Equipment: Never reuse or share needles, syringes, cookers, or cottons. Needle exchange programs are super helpful for this.
- Don’t Share Water, Tourniquets, or Swabs: Even water for mixing drugs or cleaning tools should be single-use.
- Practice Safe Snorting: If snorting, use your own straw or tube every time. Please don’t share or set it down on surfaces that might be contaminated with blood.
- Get Vaccinated for Hepatitis A and B: These vaccines can keep you protected since there’s no vaccine for hepatitis C.
- Know the Risks and Get Tested Regularly: Testing helps catch hepatitis early so it doesn’t quietly damage your liver over time.
Many communities offer free or low-cost testing, and needle exchanges don’t just supply clean gear; they usually also provide hepatitis vaccinations. It’s a brilliant idea to ask about the options when you visit, or check online to find the nearest program. If you’re unsure about your risk, regular blood tests can give peace of mind and help spot an infection before it causes significant harm.
Common Barriers Facing Drug Users
Most people assume that not sharing is easy, but the reality is a bit more complicated. Here are some barriers I see come up again and again:
- Stigma and Fear of Judgment: Some folks avoid needle exchanges or medical care because of how they’ve been treated before. This keeps them from getting tested or finding clean supplies.
- Poverty or Homelessness: If you don’t have a safe, private place to use drugs, clean supplies and good hygiene are way harder to come by.
- Limited Health Education: Not everyone knows about all the different ways hepatitis can spread. Public health messages might not reach everyone, and information overload can make it hard to pick out the key points.
- Laws Limiting Access: Some communities make it hard to get clean needles, and in some places, it’s even a crime to carry them without a prescription.
These challenges don’t mean there’s no way to stay safer; they show why well-planned support programs can make such a difference. Even if someone wants to use clean equipment every time, legal or financial barriers often get in the way. Lifting those barriers is one of the most important ways to boost community health and help prevent the spread of hepatitis.
Why Harm Reduction Strategies Work
Harm reduction is about practical, real-world ways to make things safer, not perfect. Needle exchange programs, mobile testing, education efforts, and even supervised injection sites have been shown to help slow the spread of hepatitis in communities with high rates of drug use. By making it possible always to get new gear and to get regular check-ups, these approaches help more people avoid infection and keep others safer, too. They create a supportive environment, reduce the stigma associated with drug use, and often serve as pathways to additional health care and support services. Community-based harm reduction models are now being adopted in many cities, providing a lifeline for folks seeking help and knowledge without fear of punishment or shame.
Real-World Examples of Hepatitis Prevention in Action
I’ve seen some approaches work exceptionally well in neighborhoods where hepatitis C used to be everywhere:
- Community Needle Exchanges: These programs allow people to get clean supplies without fear of judgment and offer testing and vaccines in the same spot.
- Peer Education Teams: Folks with lived experience go out and talk to others about hepatitis, safe use, and where to find free help.
- Integrating Care: Some clinics offer hepatitis C treatment alongside addiction care, so folks don’t have to bounce between places for help.
- Mobile Health Vans: These bring health services—including testing, clean gear, and vaccinations—directly to people in need, making it easier for those with transportation or mobility issues to access care.
When these supports are in place, the rate of new infections drops a lot, and people are more likely to get treatment if they do catch hepatitis. On top of that, building trust within these neighborhoods helps reduce stigma, lifts those most at risk, and creates a safer space for open conversations about both drug use and health care. Everyone needs to know that success stories are out there, and harm reduction is absolutely making a difference.
Frequently Asked Questions
How soon can hepatitis show up after being exposed to shared drugs?
Hepatitis C and B can take a few weeks to a few months to show up in blood tests. That’s why regular testing matters, even if you feel fine.
Can you get hepatitis just by touching surfaces with dried blood?
Hepatitis B and C can live on surfaces for hours or days. If that blood gets into a cut, crack, or sore on your skin, there’s a chance of infection.
Are there symptoms right away if I get hepatitis from drug use?
Most people don’t notice symptoms for a while, especially with hepatitis C. Some feel tired or sick, but many only find out when they get tested.
Staying Safe and Reducing Stigma
Hepatitis spreads easily in communities dealing with drug use, but there are really effective and practical ways to lower your risk. It’s never just about individual choices; support makes a huge difference, and small changes in habits or access to supplies go a long way. If you’re curious or worried, don’t hesitate to ask for a test or pick up clean gear. It’s about taking care of yourself, your friends, and your community. Solid information, honest conversations, and supportive services are all part of the solution. Everyone deserves access to tools and resources that help keep them healthy, no matter their circumstances. By working together, we can help make hepatitis much less of a threat for folks who use drugs and the wider community.
Video: How Hepatitis Spreads Through Drug Use