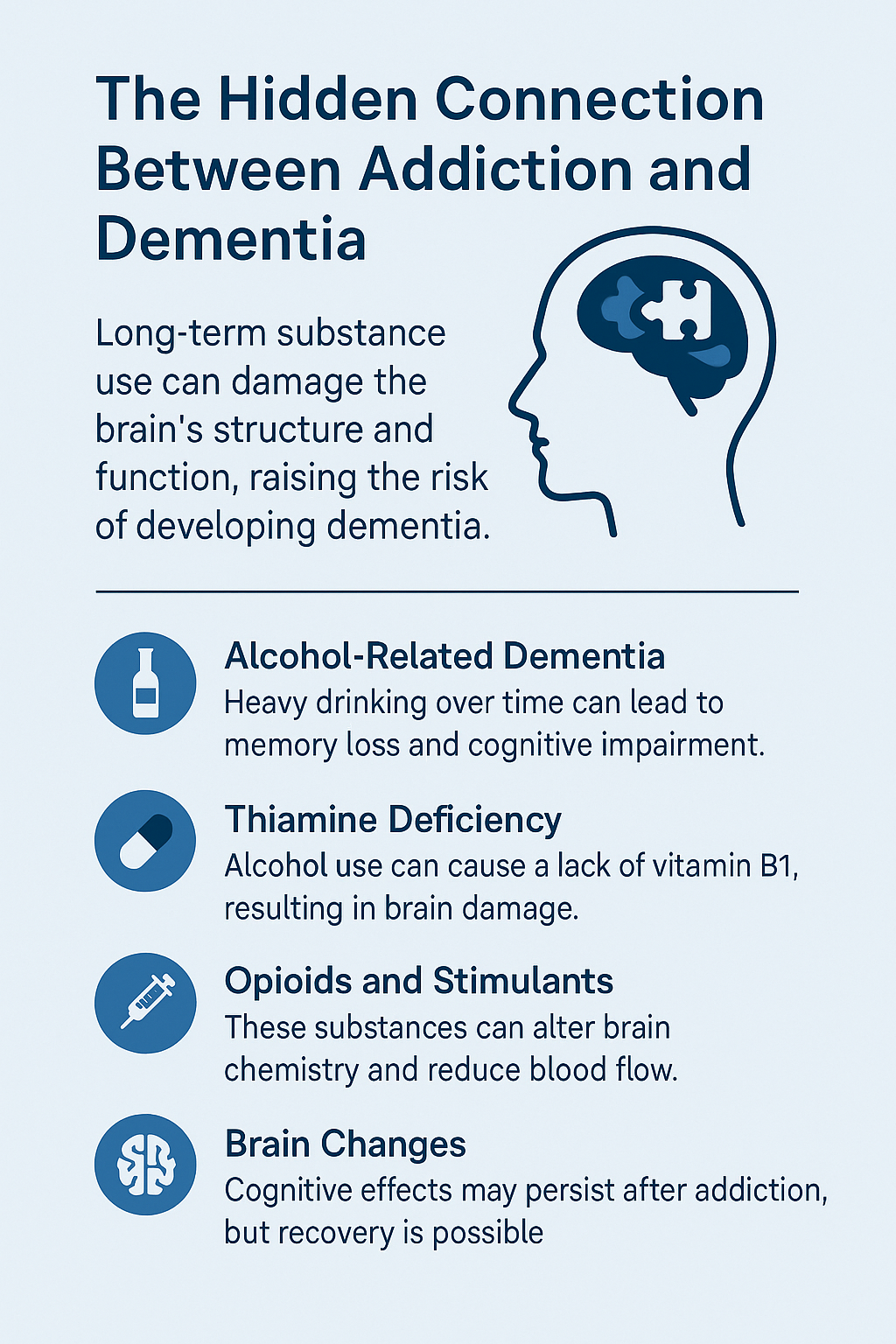
Addiction can affect much more than just mental health or physical well-being. It also plays a significant role in long-term brain health. Over time, addiction has been linked to brain changes that stick around and go beyond temporary fogginess or short-term memory lapses. Something many people don’t realize is that addiction and substance abuse, especially when they continue for years, can actually raise the risk of developing dementia later on. If you or someone close to you is dealing with addiction, getting a handle on this link is really important for protecting brain health.
How Addiction Impacts the Brain
Brain health often takes a hit with ongoing substance use. When someone is dealing with addiction—whether it involves alcohol, drugs, or other substances—those substances directly impact the brain’s structure and how it works. With repeated exposure over time, brain cells (neurons) begin to function differently, and specific brain regions may lose their usual mode of communication.
Scientifically, substances can mess with the brain’s normal flow of chemicals. For instance, dopamine, the chemical that drives motivation and reward, gets knocked out of balance by drugs or alcohol. Areas such as the hippocampus, which is essential for forming and retaining memories, or the frontal cortex, which handles judgment and planning, can shrink or lose connections to other brain regions.
These changes often begin slowly, manifesting as everyday forgetfulness or difficulty with focus. But as years go by, the brain’s ability to bounce back gets weaker. This is when the risk for dementia grows—when a brain can’t defend or fix itself well, it becomes more likely to develop serious memory and thinking troubles. For more details, check out resources from the Alzheimer’s Association.
Types of Addiction Linked to Dementia
Not every form of addiction has the same impact on dementia risk, but some are more widely connected to it based on research and what healthcare professionals see. Here are the main substances that tend to be trouble spots when it comes to raising dementia risk:
- Alcohol: Chronic heavy drinking is a significant cause of brain damage and forms of dementia like Wernicke-Korsakoff syndrome. Alcohol can cause the brain’s gray and white matter to shrink and make it harder for neurons to send messages efficiently.
- Prescription Drugs: Abusing prescriptions—especially sedatives, opioids, or anticholinergic drugs—leads to memory loss and confusion, two early warning signs of long-term problems. Long-term benzodiazepine use is a well-proven risk factor.
- Illicit Drugs: Drugs like methamphetamine, cocaine, and heroin can actually change the brain’s structure and speed up cognitive problems. These substances are often neurotoxic, meaning they directly damage or kill brain cells.
- Tobacco: Having a nicotine addiction can damage blood vessels, which cuts off blood flow to the brain. Less blood and oxygen mean brain cells are more likely to get damaged over time.
The connection between addiction and dementia doesn’t come down to the substance alone. How much is used, how often, and for how long all play a role. There’s no one-size-fits-all timeline either, since factors like genetics, age, basic health, and mixing substances (like alcohol with drugs) matter too.
Addiction, Dementia, and Everyday Symptoms
Early dementia signs aren’t always obvious, especially when addiction is involved. Common early symptoms can easily be confused with side effects of addiction, such as being forgetful, mood swings, or making bad decisions. Some signs to keep an eye on include:
- More frequent memory gaps—forgetting names, places, or recent talks
- Having trouble with simple tasks or following instructions
- Getting lost in places that should be familiar
- Struggling with money or solving daily problems
- Unexpected mood changes or pulling away from social events
I’ve come across stories where a person’s sudden forgetfulness or a shift in their personality was first blamed on substance use, but later, it turned out to be early-stage dementia. Hearing from a professional early on can significantly help plan care and support.
Short-Term and Long-Term Risks
Addiction impacts the brain right away, but the real trouble comes with time. Short-term changes may include blackouts, confusion, or clumsy movements, but with repeated use, these can evolve into long-lasting brain problems. Let’s break it down:
- Short-term risks include blackouts, poor decision-making, forgetfulness, and impaired coordination.
- Long-term risks include chronic inflammation, nerve damage, a smaller brain size, and a steady increase in risky actions, which can lead to brain injuries or ongoing blood flow problems.
Withdrawal episodes—especially with alcohol or benzodiazepines—are also hard on the brain. Every withdrawal adds new stress, and the damage piles up over the years. Even after quitting, the brain sometimes can’t completely heal, which keeps the dementia risk high even decades down the road. Scientific studies back this up.
Factors That Make Dementia More Likely in Addiction
Not everyone who struggles with addiction ends up developing dementia, but some things do push the risk higher:
- Family background—having a close relative with dementia or Alzheimer’s disease
- Other health issues, like diabetes, high blood pressure, or depression
- Poor eating habits or little exercise, which cut the brain’s natural repair abilities
- Mixing multiple substances puts added stress on the brain
- Living alone or lacking a social support system
Age also plays a role. The older someone is when they keep using substances, the bigger the impact on their brain. However, starting at a young age—such as during the teenage years—can also cause significant damage, as the brain is still developing at that stage.
What Can Help Lower the Risk?
The best way to help head off dementia risk is to move away from addiction. Even if completely stopping seems impossible, cutting down helps. Here are a few practical moves that have been shown to support brain health, whether someone is still in recovery or wants to protect their mind:
- Stay connected to others—talk with friends, family, or support groups to keep the brain busy.
- Eat a diet good for the brain (lots of leafy greens, nuts, and fish)
- Get regular exercise, which can boost mood and increase blood flow to the brain
- Try to get enough sleep—sleep loss can make memory issues much worse
- Find experts who can help put together a plan to cut down or quit substance use
Treatment options, such as counseling, medication-assisted therapy, and cognitive behavioral methods, can provide a boost. The sooner someone reaches out for help, the better their chances are of protecting their brain health in the long run.
Real-World Example
One story stands out to me: a man who began drinking heavily in college kept it up through his 50s. When he finally quit, he was already dealing with regular memory problems and confusion. With the right help and lifestyle adjustments, he managed to prevent things from getting worse, but it required significant effort. His story makes it clear—the risks are real, but positive change is possible nearly any time.
Why Early Awareness Matters
Spotting problems early and getting a sense of the connection between addiction and dementia can really turn things around. Writing off memory slips as just a natural part of aging or making excuses while someone’s still using is easy, but being curious rather than critical helps people reach out for help before significant problems arise.
There are community resources, hotlines, and clinics that are all good places to start if you’re unsure. I recommend checking SAMHSA’s National Helpline as a confidential first step. Conducting research helps families make informed decisions about treatment and prevention.
Frequently Asked Questions
Here are some of the most common questions I hear about addiction and dementia:
Can quitting addiction reverse dementia?
It depends on how far things have gone. Some early symptoms, like mild memory loss, can get better after stopping the substance and starting a brain-healthy lifestyle. Once dementia gets to an advanced stage, though, reversing it is rare—but treatment can help slow it down.
Does every type of addiction make dementia more likely?
The danger is most significant with alcohol, some prescription drugs, and illegal substances. Tobacco mainly affects blood flow to the brain, which can still lead to dementia. Behavioral addictions like gambling usually don’t hurt the brain directly, but added stress can still weigh on mental health over time.
How soon will dementia signs pop up after many years of addiction?
Symptoms sometimes show up years—or even decades—after quitting. It depends on how much was used, for how long, and on genetic and lifestyle factors. Staying active in protecting your brain health is a good plan, no matter your past.
Protecting Brain Health Moving Forward
Knowing that addiction can raise dementia risk isn’t just about looking back at past decisions. It’s more about making fresh choices for the future. Taking little steps and taking early action really do make a difference in keeping your mind sharp and improving your overall quality of life.
If you’re concerned about yourself or someone close to you, reaching out or getting more info is always a smart move. Maintaining your brain health can require patience, support from your community, and, at times, professional assistance—but positive change can occur at any stage.
Video: Can Addiction Really Cause Dementia?