Gaps in opioid addiction treatment continue to leave far too many people without access to care that could change—or even save—their lives. Opioid use disorder is a chronic, relapsing medical condition that requires timely, individualized, and ongoing support, yet many people encounter obstacles at nearly every step of the treatment process. These barriers can include limited availability of providers, long wait times, insurance restrictions, stigma, and lack of coordinated care. In this discussion, I take a closer look at where these gaps exist, why they persist, and how systemic, geographic, and policy-related factors make it harder for individuals to receive treatment when and where they need it most. Understanding these challenges is a critical step toward improving access, reducing overdose deaths, and supporting long-term recovery.
Overview of Opioid Addiction Treatment and Why Access Matters
Treatment for OUD goes way beyond just stopping drug use. It’s an all-in-one process, typically involving medications such as methadone, buprenorphine, and naltrexone, counseling, peer support, and other services. These options have strong evidence behind them and can cut overdose risks, reduce relapse, and support lasting recovery.
The trouble is, not everyone has a smooth path into care. According to the Substance Abuse and Mental Health Services Administration (SAMHSA), only about one in five people with OUD actually receives specialized treatment. That figure highlights how significant these gaps are and how much room there is for improving the treatment system. When access is restricted, people are more likely to face medical, legal, and personal consequences of untreated opioid use, and communities shoulder both public health and economic burdens.
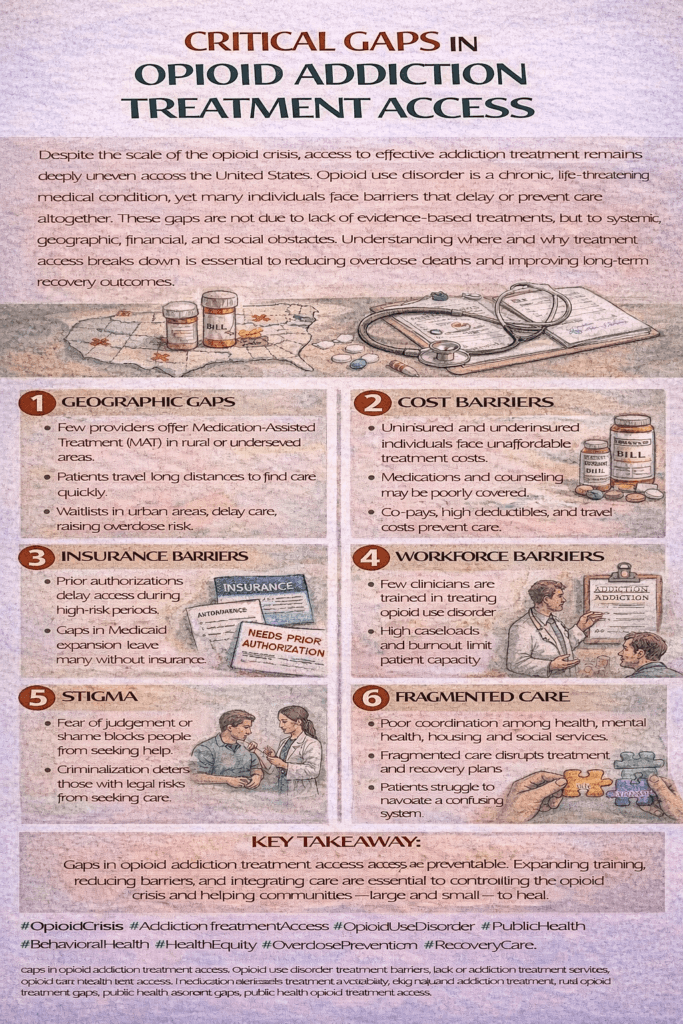
Main Barriers to Opioid Addiction Treatment Access
Several common themes come up when talking with individuals, families, and providers about what gets in the way of treatment. Here are some reasons that access is out of reach for so many:
- Stigma: Judgment and misunderstanding around addiction discourage people from seeking help and can influence how they are treated by the healthcare system.
- Regulatory and Policy Hurdles: Federal and state regulations can limit the availability of specific medications, set strict requirements, or cap the number of patients clinics and doctors can treat.
- Geographical Gaps: People living in rural or underserved areas are more likely to have few, if any, local options for evidence-based addiction care.
- Insurance and Cost: High costs, limited coverage, and administrative red tape around insurance make it hard to get and keep treatment.
- Workforce Shortages: There aren’t enough providers trained and willing to deliver OUD care, especially in certain areas of the country.
These aren’t just minor inconveniences; they result in months or even years of unmet need for treatment and support, sometimes with tragic outcomes.
How Gaps Show Up in Real Life
Practical obstacles pop up throughout the process, from the moment a person decides to seek help to maintaining progress. Some patient stories really bring these issues into focus. I’ve spoken with people who waited weeks for an appointment, only to find the closest clinic was hours away. Others said their insurance denied coverage for medication, or limited counseling services to just a couple of visits, which clearly isn’t enough for a long-term, chronic health condition.
The opioid crisis hasn’t hit every community equally. Small towns and rural regions often have the highest overdose rates but the fewest providers. Some counties have no clinics at all. Transportation and privacy concerns also arise in small towns; everyone seems to know when someone is seen at a treatment center. That fear can push people away from care, even when it’s technically available. On top of these, lack of childcare and worries about employment or legal issues often act as invisible but powerful obstacles to seeking treatment.
Medication-Assisted Treatment (MAT): Availability and Challenges
Medication-assisted treatment (MAT) includes the use of FDA-approved medications together with counseling and behavioral therapies. MAT is widely recognized as the gold standard, backed by substantial research, but its availability can be spotty across the U.S. Some of the leading challenges are:
- Provider Limits: Doctors need extra training and a waiver to prescribe buprenorphine, and there’s a cap on how many patients some can treat concurrently.
- Clinic Shortages: Methadone can only be given out at certified opioid treatment clinics, which are far more common in city centers than in rural ones.
- Regulation Overload: Strict federal and state rules make it harder for new clinics or providers to open in areas that have unmet needs.
- Out-of-Pocket Costs: Even when treatment is technically available, co-pays or fees can keep people from adhering to their care plans.
Some states have expanded telemedicine and loosened restrictions, especially after the COVID-19 pandemic, but these solutions are playing catch-up in many locations. Continuous efforts are required to reach the populations that need services most.
The Role of Stigma in Limiting Treatment Seeking
Stigma doesn’t just make people feel bad; it also changes whether they reach out for help. Many people with OUD worry about being judged by healthcare providers, employers, or their neighbors. Some even share that their healthcare experiences were so negative that they avoid clinics altogether. I’ve met individuals who delayed seeking treatment for years simply because they feared what others would say. This hesitation increases risks for overdose and serious medical complications.
Stigma is also found in policy, like when insurance providers attach more requirements or restrictions to addiction care than to other chronic illnesses. There’s a strong need for more public education and for healthcare providers to be more open-minded and supportive when discussing OUD and recovery treatment.
Insurance Roadblocks and Out-of-Pocket Expenses
Insurance coverage for OUD treatment is uneven, even though mental health and addiction parity laws are supposed to protect patients. Some insurance plans still place tough limits on the amount, type, or length of addiction care you can get. Others require preauthorization or try to shuffle people into less effective treatments to cut costs. Patients spend hours wrestling with paperwork and appeals, only to get hefty bills they can’t pay.
Medicaid and Medicare have opened opportunities for many, but eligibility and covered services vary by state. High deductibles and copayments discourage people from seeking care, particularly in states that haven’t expanded Medicaid.
Provider Shortages and Service Gaps
Even with more clinics and providers entering the field, there are far from enough trained in addiction medicine. Some estimates indicate that more than 1 million people need help, compared with those who can actually access OUD care. Rural America faces tough odds in finding a provider who can prescribe needed medications, especially if folks rely on public transportation or have work or family responsibilities that make traveling challenging.
Staffing shortages remain an issue inside clinics as well. Many locations are stretched thin, juggling large caseloads, high turnover, and staff burnout. This situation can leave people waiting weeks just to get an assessment, which isn’t ideal when dealing with a fast-changing condition like OUD.
Examples of Policies and Solutions Worth Checking Out
Several efforts are beginning to close these gaps. More states and clinics are rolling out telemedicine options, letting patients connect with providers online and reducing both travel and wait times. Since early 2020, temporary rule changes have allowed some clinics to offer medication refills through telehealth, making it easier for patients to stick to their plans.
Other positive steps include expanding Medicaid wherever possible, deploying mobile treatment units that bring care directly to communities, and altering scope-of-practice laws to allow nurse practitioners and physician assistants to provide care. These options mean that medical help is moving closer to where people live and work.
Peer recovery coaches and certified addiction counselors play a pivotal role, too, especially where medical staff are in short supply. Their lived experience carries valuable weight, helping to break stigma and inspire trust among those reluctant to enter formal care. Community support networks are being built up to fill the gaps, offering assistance not just with treatment, but also with housing, employment, and lifestyle changes.
Frequently Asked Questions
Questions about opioid treatment access come up a lot. I’ll answer a few of the most common ones below:
How do I find treatment in an area with few providers?
Start by looking up SAMHSA’s treatment locator or checking your state’s resources online. Some hotlines and local organizations can help you connect with telemedicine or mobile programs if travel is an obstacle.
Is medication-assisted treatment safe to use for a long time?
MAT is both safe and effective for long-term use. Research shows that the longer someone stays on treatment, the better their recovery and the lower their risk of overdose.
Will my insurance cover opioid addiction treatment?
Certain coverage depends on your plan, so check for equality in mental health benefits and call your insurer for the latest list of what’s covered and which providers are in-network. Medicaid covers a wide range of options in most states.
What should I do if I’m running into waitlists or denials?
If you’re stuck on a waitlist, don’t give up. Ask about other medication options, peer recovery support, or telehealth, and keep calling for cancellations. Getting on multiple waitlists can help speed things up. Sometimes, local community health centers or support groups may offer advice or fast-track options for urgent cases.
Looking Ahead: Where Change Is Still Needed
Major improvements in opioid addiction treatment access come down to a few key elements: lowering stigma, boosting the availability and scope of providers, making insurance coverage more reliable, and supporting recovery through every phase. Projects such as mobile clinics, telemedicine, and flexible provider qualifications can help break down these barriers, but real progress demands steady funding and policy adjustments that prioritize people in need.
Ultimately, creating a system that centers on dignity, practicality, and day-to-day support will help more folks get into, and stick with, treatment. Efforts to strengthen community support, fine-tune insurance rules, and offer patient-centered care are all part of the puzzle. Tackling these access issues is challenging, but with ongoing commitment, meaningful change is within reach for individuals and entire communities facing the opioid crisis.
Video: The Gap Between Needing Help and Getting It #AddictionTreatment #OpioidCrisis #Recovery