Alcohol consumption and fatty liver disease are linked much more closely than many folks realize. It’s not just about drinking too much once in a while; it’s about how regular alcohol intake can gradually change your liver and start causing problems long before you notice any symptoms. If you’re wondering how alcohol affects your liver and want to know what to watch out for, this guide has you covered.
What Is Fatty Liver Disease and Why Does It Matter?
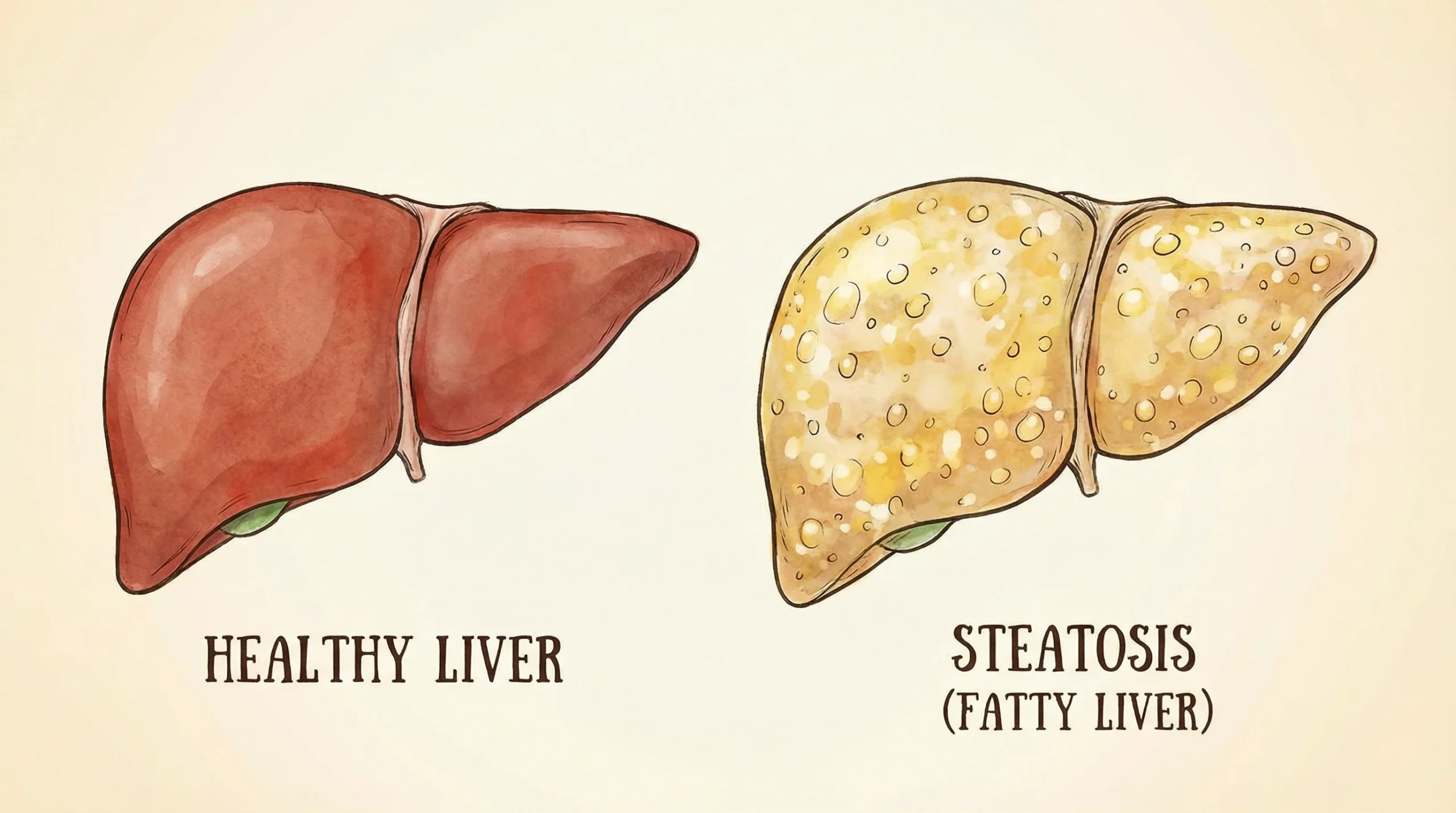
Fatty liver disease happens when too much fat builds up in your liver cells. The tricky thing is that your liver is a hardworking, resilient organ, so it often gives no obvious warning signs at first. Over time, though, this buildup can disrupt how your liver works, leading to more serious issues if left unchecked.
There are two main types of fatty liver disease: alcohol related fatty liver disease (AFLD) and nonalcoholic fatty liver disease (NAFLD). Alcohol related fatty liver disease is, as you might guess, directly tied to drinking habits. Nonalcoholic fatty liver disease happens in people who drink little or no alcohol, and it’s generally linked to things like obesity, diabetes, or high cholesterol. But today, let’s focus on how drinking affects your liver and where those risks actually start.
How Alcohol Impacts the Liver
Your liver has the tough job of handling toxins in your bloodstream, and alcohol is right at the top of that list. When you drink, your liver breaks down alcohol using special enzymes. One byproduct of this breakdown is acetaldehyde, which is pretty toxic. Over time, repeated exposure to acetaldehyde and other related chemicals causes inflammation and damage. Fat starts to build up in your liver cells, and this can set the stage for fatty liver disease.
It’s important to understand that the effect is dose-dependent. The more you drink, and the longer you keep it up, the riskier it gets for your liver health. According to the CDC, heavy drinking is considered eight or more drinks a week for women, and 15 or more for men. But even lower levels can be enough to trigger fatty changes over time in some people.
Signs and Progression of Alcohol Related Fatty Liver Disease
One of the most frustrating things about fatty liver disease is how silent it can be in the early stages. Some folks only find out from a blood test or imaging scan done for another reason. Still, sure warning signs could pop up as things progress:
- Tiredness or feeling weak: Your liver handles tons of energy-related tasks, so when it’s under stress, your energy dips.
- Upper right belly pain: Some people feel discomfort or ache under their ribs where the liver sits.
- Unexplained weight loss: As the liver struggles, you might lose weight without trying.
If fatty liver keeps getting worse, it can move on to more serious stages like alcoholic hepatitis (inflammation and swelling) or cirrhosis (scarring of the liver). Each stage carries bigger health risks, and if untreated, it can be life-threatening.
How Much Alcohol Is Too Much for the Liver?
Not everybody’s liver responds the same way to alcohol. Genetics, gender, body weight, and underlying health conditions all affect how alcohol hits you. Here’s a general idea folks find helpful:
- Men who drink more than 2–3 standard drinks a day, or women who have more than 1–2, are already running an increased risk.
- Daily or nearly daily drinking adds up much quicker than occasional, moderate use.
- Binge drinking, meaning lots of drinks in a short time, can be especially damaging.
Some research even hints there’s no completely safe level of alcohol for liver health. If you already have liver issues, cutting alcohol out entirely is usually recommended.
Other Risk Factors That Make Alcohol More Dangerous for Your Liver
Drinking isn’t the only thing raising your risk. These factors can make your liver more sensitive to alcohol’s effects or speed up disease progression:
- Obesity: People carrying extra weight are more likely to develop fatty liver even with moderate drinking.
- Diabetes or high cholesterol: These conditions stress the liver, and combined with alcohol, damage can ramp up quickly.
- Genetics: Family history plays a role. Some folks process alcohol less efficiently due to their genetic background.
- Hepatitis B or C: Pre-existing liver infections increase your vulnerability.
Practical Steps for Lowering Your Risk
If you’re drinking and want to keep your liver as healthy as possible, these changes can really help:
- Cut back or stop drinking: Even reducing your intake can slow down or even turn around early-stage fatty liver. Complete abstinence gives the most significant benefit, especially for those already at risk.
- Eat a balanced diet: Focus on plenty of fresh veggies, lean proteins, and healthy fats. Avoiding many fried foods and added sugars helps your liver process nutrients and recover.
- Stay active: Exercise isn’t just good for your heart and weight—it also improves how your body processes fat and can actively lower liver fat stores.
- Manage health conditions: Keep things like blood pressure, cholesterol, and blood sugar in check. This lightens the load on your liver and can keep disease from getting worse.
- Regular checkups: Blood tests and doctor visits are super crucial for catching liver issues before they get serious. If you’re a regular drinker, chat with your doctor about whether liver function tests are a good idea for you.
Some folks also find joining community programs or online forums helpful for staying on track with these changes. Sharing your goals and progress can help you stay motivated as you improve your liver health.
Challenges When Trying to Change Drinking Habits
Cutting back on drinking can sometimes be trickier than it sounds. Social settings, work culture, stress, and old habits all play a role. Here’s how I’ve seen people handle these roadblocks:
- Setting clear limits: Keeping track of how much you drink helps you stay honest with yourself. There are handy apps for this, or just jotting it down in your phone works too.
- Finding alcohol-free alternatives: There are loads of great-tasting nonalcoholic beers and cocktails now that make socializing easier without feeling left out.
- Talking to friends or family: Letting folks know you’re cutting back often leads to more support and fewer offers to drink. Some people even join in with you!
- Getting professional help: If quitting feels impossible on your own, healthcare providers can help you make a plan or point you toward support groups or counseling.
Sticking with your goals is tough, but it helps to remind yourself why you’re doing it and to celebrate your wins along the way. Even small changes can set you up for better long-term health.
The Role of Early Detection and Regular Screening
Most people with early fatty liver disease don’t feel any different. That’s why regular health checkups can make a real difference. Blood tests for liver enzymes, ultrasounds, or even newer imaging tools can detect liver fat before it leads to more serious problems. In my experience, catching things early means you have way more options to turn things around.
If you have risk factors like regular drinking, obesity, or a family history of liver problems, letting your doctor know is always wise. They might recommend extra monitoring or lifestyle tweaks to keep things in check.
What to Ask Your Doctor About Alcohol and Fatty Liver Disease
If you’re unsure where you stand, or you want to check on your risk, here are a few conversation starters for your next appointment:
- Am I drinking at a level that could hurt my liver?
- Should I get regular liver function tests?
- What changes would help my specific health situation?
- How can I spot symptoms early if they start to appear?
Bringing these questions to your doctor opens the door to personalized advice and keeps you ahead of potential issues.
Frequently Asked Questions
Question: Can fatty liver disease be reversed if I stop drinking?
Answer: In many cases, yes. Early fatty liver disease can often improve or go away entirely when alcohol use stops and healthy habits are started. More advanced diseases like cirrhosis may be permanent, so catching and acting early is what matters most.
Question: Are there any symptoms to look out for?
Answer: Early-stage fatty liver usually comes with no symptoms. Later stages may bring tiredness, right-sided abdominal pain, or yellowing of the skin or eyes. Most people find out through blood work or imaging during a checkup.
Question: Is occasional drinking safe for the liver?
Answer: Occasional small amounts are less risky than regular or heavy drinking. However, for people with other liver risks or a history of liver disease, avoiding alcohol altogether is safest.
Takeaway for Healthy Liver Habits
Building healthy drinking habits and staying aware of your liver’s health can lower your chances of developing fatty liver disease or help you recover if you’ve already started down that path. With a few mindful choices, it’s possible to keep your liver in good shape and enjoy life with fewer worries about long-term health effects.
Watching your alcohol intake, getting regular checkups, and making small everyday changes all add up. Your liver is tougher than you think, and it really appreciates a bit of care now and then. A healthy liver helps keep the rest of your body running smoothly, so each positive choice is a victory for your overall well-being.
Video: Fatty liver from alcohol: signs you’re already damaged #shorts #health #warning