Tobacco use remains one of the most complex and controversial health issues of our time, surrounded by decades of research, marketing influence, and evolving public opinion. While the link between smoking and deadly cancers—like lung, throat, and pancreatic—has been proven again and again, conflicting information and social normalization still cloud the truth. It’s not just about statistics; behind every number are real people whose lives have been changed or lost. Research continues to show that chemicals in tobacco smoke damage DNA, weaken the body’s ability to repair cells, and trigger the development of cancer over time. Despite widespread awareness, many underestimate the long-term risks or believe that occasional smoking isn’t harmful. By cutting through misinformation and looking at what science and lived experiences reveal, we can better understand how smoking quietly fuels some of the most aggressive cancers—and why prevention and education remain so vital for our health and our communities.
How Smoking Affects the Body: A Quick Breakdown
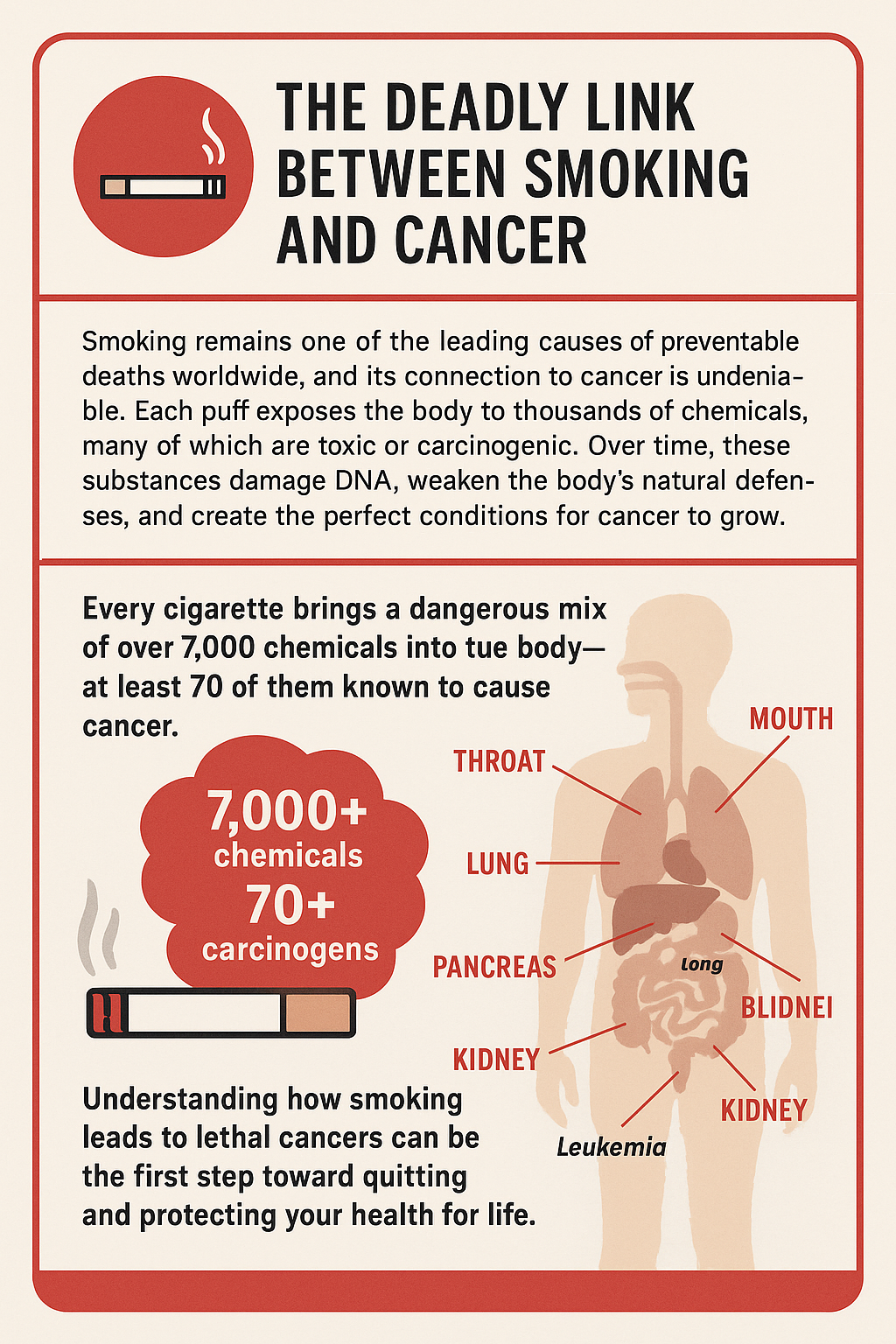
Lighting up a cigarette isn’t just about nicotine. More than 7,000 chemicals get into your body, and at least 70 of them are known to cause cancer. This isn’t scare language—it’s straight from trusted health groups like the CDC and the American Cancer Society. Every time you smoke, your cells are exposed to a messy mix of substances: tar, formaldehyde, polycyclic aromatic hydrocarbons, and benzene, just for starters. Each one can mess with your cell’s DNA, and that’s where the whole cancer risk snowballs.
Doctors spell out two main paths for how tobacco smoke inflicts harm:
- Direct contact with tissues: Your mouth, throat, and lungs take a beating every time you inhale.
- Chemical absorption: Many chemicals seep into your bloodstream and travel to other organs—sometimes in places you’d never expect, like the bladder or pancreas.
This damage adds up over time. At first, coughs or warnings may seem like a minor annoyance, but over time, cells continue to be chipped away, and the risks accumulate.
The Science Connecting Smoking and Lethal Cancers
The hard truth: Smoking is the leading cause of preventable cancer deaths worldwide. It’s essential to understand the level of certainty in this area. The primary cancer types with the nearest connection to smoking include:
- Lung cancer
- Mouth, throat, larynx (voice box), and esophagus cancer
- Bladder cancer
- Pancreatic cancer
- Stomach, kidney, and cervical cancers
Doctors have long recognized these links, but now dozens of extensive studies have confirmed them. The World Health Organization (WHO) says around 85% of lung cancer deaths are due to smoking. For other cancers, smokers are usually two to five times more likely to get the disease than nonsmokers.
If someone says, “My grandpa smoked every day and never got cancer,” that’s just a personal story. Researchers look at whole populations rather than single anecdotes, and the science keeps showing a significant connection between smoking and cancer.
Looking Beyond Lung Cancer: Other Risks Worth Knowing
Lung cancer steals most of the spotlight—and, honestly, it deserves it—but it’s far from the only cancer strongly linked to tobacco. Here’s how smoking boosts risk elsewhere in your body:
- Mouth and throat cancer: Every cigarette’s puff passes right through your lips, gums, and throat, so those tissues get hit first by dangerous chemicals.
- Bladder cancer: Your kidneys filter your blood and send toxins (including those from smoke) out through your urine. The bladder gets exposed over and over to these damaging chemicals.
- Pancreatic cancer: Smokers are at greater risk here, too. Recent studies suggest up to a quarter of pancreatic cancers could be related to tobacco.
- Cervical and kidney cancers: Both organs face attack from chemicals absorbed into your blood. Even less obvious cancers like stomach and colorectal types are more often found in those who smoke.
So while lung cancer is the big concern, smoking takes a toll on a wide range of organs you might not have thought about.
Spotting Myths and Clearing Up Confusion
With such a flood of information, sorting fact from fiction gets tricky. Let’s break down some common myths I’ve come across:
- Myth: “Filters keep out the dangerous stuff.” Filters might help a hair, but they can’t remove most of the cancer-causing chemicals. The danger is still there.
- Myth: “Light or ‘natural’ cigarettes are safer.” Swapping to ‘light’ or ‘herbal’ smokes doesn’t strip out carcinogens. Your cancer danger basically stays the same.
- Myth: “Switching to cigars or pipes can’t hurt.” Actually, these options can carry similar or even higher risks for certain cancers, especially in your mouth and throat, since the smoke sits in your mouth longer, even if you don’t inhale deeply.
For solid, unbiased resources with more information, consult the National Cancer Institute or the CDC for accurate data and statistics.
Common Signs & What to Watch For
Symptoms from smoking-connected cancers can seem pretty ordinary at first, but recognizing warning signs might help catch a problem sooner. Some key things to keep an eye on:
- A persistent cough or one that worsens over time
- Blood in spit, urine, or when coughing
- Difficulty swallowing or pain when swallowing
- Unexplained weight loss
- Ongoing hoarseness or consistent mouth/throat pain
- Changes in bladder or bowel routines
If anything, if a strange or persistent symptom persists for more than a couple of weeks, consulting a healthcare professional is a smart move.
Staying Informed & Taking Steps for Health
It’s key to know the risks that come with smoking—and remember it’s not just about lung cancer. Even for long-time smokers, medical evidence says quitting, at any age, slashes your risk for nearly every smoking-related cancer. Within just a few years, your risk of cancer (especially in the mouth or bladder) goes down.
You can take some practical steps to boost your odds and stay healthy:
- Consider quitting: Health improvements begin immediately after you stop using it. You don’t have to go it alone—nicotine replacements, support groups, or counseling can give you a big lift.
- Screening tests: For older or heavy smokers, certain screenings can catch issues when they’re most treatable. Consult with your doctor to determine if this option is suitable for your needs.
- Building healthy habits: Consuming balanced meals, engaging in regular physical activity, and limiting alcohol consumption significantly increase your body’s ability to fight cancer risks.
People often think, “It’s too late for me,” but research shows health improvements can show up at any age, and even tiny changes can pay off.
Practical Concerns and Challenges
Kicking the smoking habit can feel like climbing a mountain, especially if it’s been part of your routine for years. Nicotine has a fierce hold, which is part of why folks have trouble quitting. Here’s what to expect and some valuable ideas for getting through:
- Withdrawal: You may experience rough patches, including irritability, sleep disturbances, or cravings. Nicotine gum, patches, or even certain medications can make things more manageable.
- Stress or familiar triggers: Everyday stress or specific social situations can trigger cravings. Having alternatives ready, like popping gum or stepping out for fresh air, really helps some people.
- Find your support: Don’t underestimate help from friends, family, or even online groups. Encouragement and accountability can be gamechangers.
If quitting feels impossible on your own, discussing it with a healthcare provider can reveal resources you may not be aware of. Free quit lines and smartphone apps can connect you with encouragement anytime you need it.
Frequently Asked Questions
Question: How many cigarettes must you smoke before your cancer risk goes up?
Answer: Even a few cigarettes a day increases cancer danger—there’s no totally safe “low” number. The longer you smoke, and the more you smoke, the more the risk racks up.
Question: What about vaping or smokeless tobacco? Do they have cancer risks too?
Answer: While e-cigarettes and smokeless options might seem safer, they aren’t without risk. Some of their chemicals are known or suspected to cause cancer, and there’s still plenty we don’t know about long-term effects.
Question: Can quitting drop your cancer risk to that of a nonsmoker?
Answer: Risk falls a lot after you quit—sometimes by half in just five to ten years—but it might not totally equal someone who never smoked. Still, the reduction is significant compared to ongoing smoking, and the health payoff is real.
Question: What action is best to start quitting?
Answer: Seek support. Teaming up with your doctor, finding a local program, or calling a quit line all increase your chances. Having a plan makes it much easier than toughing it out on your own.
Why This Info Matters
Knowing how smoking matches up to deadly cancers puts a real choice in your hands about how to take charge of your future health. Science-backed resources are there to help you with questions, quitting advice, or even deeper info about tobacco’s effect on your cancer risk. If you’re struggling with this habit or considering a fresh start, reaching out for support is always worthwhile. The rewards show up quicker than you might guess, and you’ll be grateful you made the move.
Video: What Happens to Your Body When You Smoke?